Nephrotic & Nephritic Syndromes: Approach & Management
advertisement
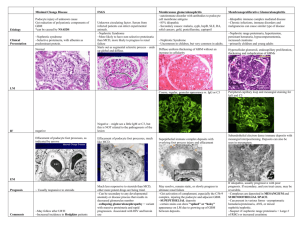
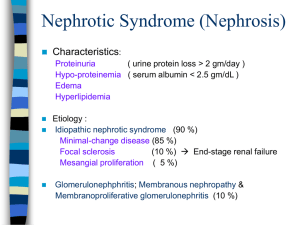
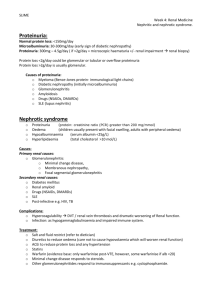
Approach to Nephrotic & Nephritic Syndromes Academic Half-Day Aug 2, 2012 Nephrology Olympics! Name two NBA athletes with Nephrotic Syndrome Proteinuria • • • Some protein in urine is normal (< 4mg/m2/hr or < 100 mg/m2/24h) Non-pathologic • • • Postural (orthostatic) Febrile Exercise-induced Pathologic • • Tubular • • Inherited (cystinosis, Wilson ds, Lowe syndrome) Acquired (antibiotic, AIN, ATN, heavy metal poisoning) Glomerular • Gross • • • • Hematuria Trauma - perform imaging and cystoscopy Pain - rule out renal stones, mass, UTI Painless - consider stones, mass, HSP, familial (thin BM), hematologic, other glomerular disease, systemic disease Microscopic • • Symptomatic - symptoms direct investigation • Asymptomatic hematuria and proteinuria - more worrisome, requires thorough evaluation by nephrology. Isolated hematuria - rarely have significant renal disease (benign familial hematuria or hypercalciuria) Edema • Differential diagnosis • Loss of oncotic pressure • • • increased protein loss Increased capillary permeability • • • • • decreased protein synthesis viral/bacterial immune mediated mechanical/thermal trauma drugs Increased hydrostatic pressure • • congestive heart failure lymphatic blockage What is the term for extreme, generalized edema? ANASARCA Golmerular Disease • Presents in one of 4 ways: • Acute Nephritic Syndrome • Nephrotic Syndrome • Rapidly Progressive Glomeruloneprhitis • Asymptomatic Nephrotic Syndrome • Nephrotic range proteinuria • • • • • • 3+ or 4+ > 250 mg/mmol creatinine > 40 mg/m^2/hr Hypoalbuminemia Hyperlipidemia Hypercoagulable Pathophysiology Glomerular Filtration Barrier NEPHROLOGY AND INFECTIOUS DISEASE! What is this fictional doc’s specialty? Etiology • Primary or idiopathic • • • • Minimal change disease FSGS MPGS Membranous nephropathy Minimal Change Disease 85% of cases FSGS 10-15% of cases Membranous Nephropathy 4% of cases In what event did this athlete win a bronze medal? 100m freestyle Etiology • Secondary causes • • • • • • • Genetic Metabolic Infections Drugs Immunologic/Allergic Malignancy Glomerular hyperfiltration • • Idiopathic Nephrotic Syndrome 90% of childhood nephrotic syndrome • 85% of all cases due to MCD Consider diagnosis other than MCD in: • • Children < 1 year and > 10 years • Extra-renal findings • More than minimal hematuria Family history nephrotic syndrome Idiopathic Nephrotic Syndrome • Clinical manifestations: • • • • Most common between age 2 and 6. Often follows minor infection. Mild edema progressing to generalized. • • • Ascites Pleural effusions Genital edema Anorexia, abdo pain, diarrhea, irritability common. What food item is known scientifically as Phaseolus vulgaris? Diagnosis • Laboratory findings • • • • • Low serum albumin High cholesterol, triglycerides, lipoproteins Low serum sodium Nephrotic range proteinuria Indications for biopsy: • • • • Age > 10, gross hematuria, hypertension Renal insufficiency Low C3 complement value Persistent proteinuria following 4 week course of steroids Treatment • Prednisone drug of choice. • Dose: 60 mg/m^2 per day divided TID • Continue daily for 4 weeks, then 40mg/m^2 as single dose on alternate days for 4 weeks. • 90% of MCD is steroid responsive • Of those, 60% relapse • Frequent relapsers can be treated with cyclophosphamide Steroid-resistance • Up to 10% of all children with NS • Poor prognosis • Eventually leads to dialysis and renal transplant Complications of Nephrotic Syndrome • • • Thromboembolic events • Loss of antithrombin III and protein S • Increase in fibrinogen concentration Infection • Loss of factor B, low IgG, impaired Tcell function • Most common infection is peritonitis • Most common organisms are Strep pneumo or gramnegatives Steroid side effects Where did this duo rank in badminton at the 2012 Olympics? DISQUALIFIED for CHEATING! Nephritic Syndrome • Results from inflammation within glomerulus • Characterized by • Hematuria, RBC casts, dysmorphic RBCs • Mild to moderate proteinuria • Azotemia, oliguria • Hypertension Etiology Low complement Normal complement Primary Postinfectious GN Membranoproliferative GN IgA nephropathy Anti-GBM disease Secondar y SLE Endocarditis Abscess Cryoglobulinemia Polyarteritis nodosa Wegener’s HSP Goodpasture’s • • • • • Rapidly Progressive Glomerulonephritis Subset of nephritic syndrome Medical emergency Characterized by renal failure in days or weeks (months) Classfication: • • • Type I - anti-GBM (idiopathic, Goodpasture’s) Type II - immune complex (PIAGN, SLE, HSP) Type III - pauci-immune (idiopathic, Wegener’s, microscopic polyangitis, drugs) Treatment • • • Induction of remission (pulse steroids, cyclophosphamide 3-6 months) Maintenance therapy (azathioprine) Newer agents - Rituximab, MMF Crescent BAD NEWS. IgA Nephropathy • • • • Most common cause of GN Idiopathic or secondary (HSP, rheumatic ds, HIV, Celiac ds, chronic liver ds) Variable presentation: • Asymptomatic hematuria and mild proteinuria • Recurrent episodes of gross hematuria • Nephrotic range proteinuria or RPGN • Hematuria coincident with URTI Treatment depends on prognostic indicators • Watch & wait vs. immunosuppressive agents Poststreptococus glomerulonephritis • • • • • Prototypic acute nephritic syndrome Occurs 2-3 weeks after pharyngitis or skin infection with GAS (nephritogenic strain) Typical history plus low C3, normal C4, and high ASOT, positive antiDNase B Self-limited disease - three phases • • • latent phase acute phase recovery phase Supportive management of hypertension and edema • Indications for biopsy include normal complement level, failure to document strep infection, GFR < 30ml/min/1.73 m2 How much does the average adult kidney weigh? 120-140 grams! • • • • • • References Gordillio, R. and Spitzer, A. The Nephrotic Syndrome. Pediatr Rev, 2009;30: 94-105. Beck, L. and Salant, D. Glomerular and Interstitial Diseases. Prim Care Clin Office Pract 2008;35:265-296. Bergstein, J. A Practical Approach to Proteinuria. Pediatr Nephrol 1999;13:697-700. Massengill, S. Hematuria. Pedatr Rev 2008;29:342-348. Pais, P. and Avner, E. Nephrotic Syndrome. Nelson’s Textbook of Pediatrics, Ch 52:18011806. Eison, T., Ault, B., and Jones, D. Post-streptococcal cute glomerulonephritis in children: clinical features and pathogenesis. Pedatr Nephrol 2011;16:165-180.