Glomerular Diseases
advertisement

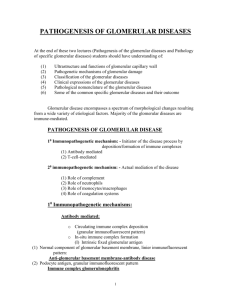
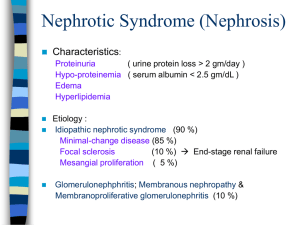
Glomerular Syndromes & Disorders Nephrotic Syndrome Immune Mediated Membranoproliferative Gromerulonephritis Membranous Glomerularnephritis Non-Immune Mediated IgA Nephropathy Focal Segemental Glomerulonephritis Minimal Change Disease Nephritic Syndrome Chronic Renal Failure Post-Steptococcal Glomerulonephritis Rapidly Progressive Crescentric Glomerulonephritis IgA Nephropathy Type 1 Type 2 Anti-GBM Antibody Immune Complex Pauci-Immune ANCA Associated 1. Goodpasture Syndrome 1. Idiopathic 1. Idiopathic 2. Post Infection 2. Idiophatic 3. SLE 2. Wegener Granulomatosis 4. Henoch-Schonlein Purpura Type 3 3. Microscopic Angiitis Differences Between Nephrotic and Nephritic Syndrome Nephrotic Syndrome Nephritic Syndrome Definition Causes Laboratory Finidngs Hallmarks Condition marked by o Very high level of protein in the urine o Low level of protein in the blood o Anasarca especially at Around the eyes Feet Hands o Hyperlipideamia o At onset, little or NO Azotemia Heamaturia Hypertension It is not a disease by itself, it is a manifestation of other underlying disease, therefore lots of diseases are associated with it, such as o Minimal Change Glumerulonephritis o Membranous Glomerulonephritis o Membranoproliferative Glomerulonephritis o Focal Segmental Glomerulosclerosis Children due to primary lesion on the kidney, but adult due to underlying disease such as o Diabetes Mellitus o Amyloidosis o SLE Proteinuria o 3.5g/day Hypoalbuminaemia Edema Hyperlipidaemia Lipiduria Massive proteinuria o Loss of protein in the urine at 3.5g or more per day Hypoalbuminaemia o Plasma albumin less then 3g/dl Anasarca o Obvious clinical manifestation Hyperlipidaemia and Lipiduria It is a clinical complex Usually an acute onset characterized by o Heamaturia o Oliguria o Azotemia (increase nitrogen level in body) o Hypertension Common lesion that can cause Nephritic Syndrome is o Proliferation of cells within the glomeruli o Accompanied by Lymphocytic infiltration o Injury to the capillary walls of the tubule Leads to the release of RBC into the urine Causing heamodynamic changes that leads to reduction in GFR o Reduction of GFR Oliguria Reciprocal fluid retention Azotemia Proteinuria Hypoalbuminaemia Edema Heamaturia Oliguria Hypertension Heamaturia Oliguria Azotemia Hypertension Glomerular Syndromes and Disorders Nephrotic Syndrome Immune Mediated Epidemiology, Etiology & Clinical Features Diseases Membranous Glomerulonephritis Other names Epimembranous Glomerulonephritis Extramembranous Glomerulonephritis 40-60 years old 50% of adult Nephrotic Syndrome Morphology o o o Etiology ‘ Chronic Immune complex disease Idiopathic in most patients Sometimes associated with o Infection o Drugs o Carcinomas o Heavy metals Clinical Features o Children and young adults 5-25 years old Etiology Chronic immune complex glomerulonephritis Associated with (generally) o Chronic infections o SLE o Cancer o Cirrhosis o Heroin abuse Can be further categorized into 2 o Type 1 – More common Can be due Hepatitis B and C SLE Infected AV shunt o Type 2 (Dense Deposit Disease) Can be due Autoantibodies – C3 Nephritic Factor (C3NEF) Clinical Features o o Basement Membrane Diffused Uniform thickening Coarsely granular deposits of IgG C3 Subepithelial projection (spikes) Electron dense Subepithelial deposits Diffuse proliferative basement membrane Thickening of glomerular capillary walls Splitting of glomerular basement membrane (tram-tracking) Diffuse coarse deposits of IgG and C3 along the GBM Electron dense subendothelial deposits o o Non-selective proteinuria Albumin Globulin With or without heamaturia Clinical Course Prognosis Children Excellent o Adults Some develop End Stage Renal Disease (ESRD) o Nephrotic Syndrome in 80% Assymptomatic proteinuria in 20% Microscopic Hematuria Indolent course Membranoproliferative Glomerulonephritis Laboratory Findings Can be either Nephrotic Syndrome 50% Acute Nephritic Syndrome 20% Recent history of URTI in 50% Hypertension with/out renal insufficiency Specifically Type 1 o Subendothelial deposits Type 2 o Intramembranous deposits Decrease in complement proteins o Classical pathway o Alternative pathway C3 Nephritic Factor (C3NEF) Circulating immune complex Prognosis Generally poor prognosis Development of ESRD within 10 years Children – 50% Adults – 80% o Progressive deterioration of renal function with/out short remission o o Glomerular Syndromes and Disorders Nephrotic Syndrome Non-Immune Mediated Epidemiology, Etiology & Clinical Features Diseases Minimal Change Glomerulonephritis Other names Nil Disease Lipoid Nephrosis Foot Process Disease Male Incidence o Children 1-8 yrs old o Adults 20-30 yrs old 80% Nephrotic Syndrome in children Etiology Idiopathic Maybe o T-cell derived factor o Loss of net negative charge on capilarry basement membrane Clinical Features Insidious Nephrotic syndrome History of URTI – 30% of cases Associated with Hodgkin’s Lymphoma Sometimes overlap with FSGS patients Without Hypertension 10% of all cases of Nephrotic Syndrome Common in adult rather than children Focal Segmental Glomerulosclerosis Lesion characterized by o Sclerosis affecting Somepart of glomeruli Focal involvement Some part of a given glomerulus Segemental involvement Etiology o o o o o Most are idiopathic Nephrotic Syndrome in adults Due to HIV, heroin abused Secondary event to IgA Nephropathy Maladaptation to nephron loss Congenital anomalies affecting the cytoskeleton of Podocytes Idiopathic Morphology o o o o o o o o o o o Laboratory Findings Light Microscope Normal finding Tubular appearance Protein droplets Lipids These are due to to reabsorption of lipoprotein in the Proximal Convulated Tubule Immunoflourescent Negative; no remarkable findings, No Ag/Ab compolex Electron Microscope Efacement of Podocytes processes Focal fusion Loss of foot processes Light Microscope Focal segmental glomerular collagenous sclerosis Immunoflourescent Deposition of IgM and complement protein In the areas of hyalinosis Electron Microscope Visceral epithelial cells exhibit loss of foot processes Grate degree of epithelial cells detachment Denudation of underlying GBM Clinical Course Selective proteinuria Confined to smaller Albumin No specific lab findings Urinalysis Blood test o o o o Prognosis Spontaneous recovery 25-40% Complete recovery 65-70% Steroid resistance pts may progress to FSGS 50% individuals with FSGS develop ESRD within 10 years of time Children has better prognosis compared to adults Glomerular Syndromes and Disorders Nephritic Syndrome Epidemiology, Etiology & Clinical Features Diseases Peak incidence in children 3-14 years old Sporatic in nature o Mostly happens during winter and spring Etiology Ab/Ag complex from o Beta hemolytic streptococci Group A Type 12 o Acute Post-Streptococcus Glomerulonephritis Other names Acute Proliferative Glomerulonephritis Acute Post-infectious Glomerulonephritis Clinical Features Acute Nephritc Syndrome Post streptococcal pharyngitis and other infections Categorized into 3 types Type 1 Anti GMB disease o Type 2 Immune-complex mediated disorder o Type 3 Pauci-immune type of CrGN o Rapidly Progressive Crescentric Glomerularnephritis (CrGN) Morphology Glomeruli Enlarged Hypercellular Proliferation of o Endothelial cells o Mesengial cells Evidence of acute inflammation Basement membrane o Deposition of IgG and C3 o Appeared coarsely granular pattern along the GBM Immunes deposits are distributed in the capillary loops o In granular, bumpy pattern o Due to the focal nature of immune complex deposition process Gross Kidneys appaer o Enlarged o Pale o Petechial heamorrhage on cotex Microscopy Light microscope o Glomeruli surrounded by crescents o Crescents are formed by Proliferation of partial cells Migrations of Monocytes and Macrophages into Bowman’s capsule Immunoflourescent o Fibrin arranged in the crescents o Ig are absent Electron Microscope o Rupture of GBM Laboratory Findings o o o o Nephritic Urine with RBC casts Evidence of streptococcal infection Serologic evidence of recent infection Decreased serum level of complement Serological markers Type 1 Anti-GBM antibodies o Type 2 Circulating immune complex o Type 3 Anti-Neutrophil Cytoplasmic Antigen (ANCA) Clinical Course Prognosis Children Best prognosis o Adult Worse prognosis Some develop progressive disease o o Rapidly progressive loss of renal function Nephritic Syndrome Progress to renal failure Can present with acute renal failure Progression to Ureamia is rapid unless prompt treatment is initiated Glomerular Syndromes and Disorders Nephritic Syndrome Diseases IgA Nephropathy (Buerger Disease) Epidemiology, Etiology & Clinical Features Young adults 15-30 years old Most common type of Glomerulonephritis Etiology IgA deposits in the mesangium Clinical Features Assymtomatic heamaturia – 40% o Happens within 1-2 days during URTI Macro heamaturia – 40% Nephrotic syndrome -10% Renal failure – 10% Very rare familial renal disease More common in males Etiology Genetic defect resulting in disturbance in composition of the basement membrane X-linked disease Clinical Features Often associated with nerve deafness Gross and micro heamturia Normal level of serum creatinine Collagen type4 Hereditary Nephritis (Alport Syndrome) Morphology Laboratory Findings Light Microscope Mesangial widening Segemental inflammation Diffuse mesangial proliferation or crescentic glomerulonephritis may also be present Immunoflourescent o mesangial deposition of IgA often with C3 and properdin and smaller amounts of other immunoglobulins (IgG or IgM) Electron Microscope o Electron-dense deposits in the mesangium that may extend to the subendothelial area of adjacent capillary walls in a small subset of cases, usually those with focal proliferation. Localized involvement of kidney Idiopathic Light Microscope Segmental glomeruli Proliferation Sclerosis o Interstitial foam cells are frequent Immunoflourescent o Absence of Ig deposition Electron Microscope o Glomerular capillary basement membrane appears Thickened Split Splintered Heamaturia Electromicroscopy o o o o Heamaturia Protein electrophoresis IgA immunoglobulin increased Clinical Course o o o o o o Difference Buerger Disease Poor prognosis in patient with Hypertension Proteinuria Male gender Smoking Hyperlipidaemia Older age Henoch-Scheloin Purpura Systemic manifestation of a disease Presented with o GIT disturbance o Arthritis o Skin rash and purpura Prognosis Males who develop renal failure and ESRD in early adulthood Por prognossi o Women Variable prognosis o