The Hazardous Headache of Nephrotic Syndrome
advertisement

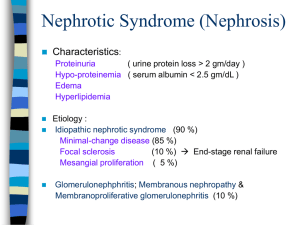
The Hazardous Headache of Nephrotic Syndrome Amy Dickey, MD Resident, Department of Internal Medicine Priyanka Duggal MD Attending, Department of Internal Medicine University of Washington, Seattle, WA The Case A 20yo female presented to the hospital with a severe headache. It is a bilateral frontal, throbbing headache, associated with emesis, photophobia, and fatigue. Three months earlier, she was diagnosed with minimal change disease by renal biopsy. Her initial symptoms of lower extremity edema and decreased exercise tolerance improved with immunosuppressive therapy; however, she was then started on a steroid taper. Two weeks prior to presentation, she noticed increased edema and breathlessness with exercise. Prior History • Past medical history: minimal change disease, onset approximately 4 months prior, diagnosed by renal biopsy • Medications: – prednisone 20mg po qday, – lasix 40mg po tid – KCL 20meq po qday • Family medical history: – – – – Great grandfather – Wegener’s granulomatosis Grandmother – migraine headache Father – hypothyroidism Mother – migraine headache • Social: – No history of alcohol, tobacco, or drug use – Currently a college business student – Previously ran triathlons Physical Exam • T 36.5 HR 55 BP 116/66 R 18 O2 sat 98% • CONSTITUTIONAL/GENERAL APPEARANCE: tired appearing female • MENTAL STATUS/NEURO: alert and oriented x4, CN II-XII intact, PERRL, strength 5/5 symmetric throughout, reflexes 2+ throughout • EYES: PERRL, significant peri-orbital edema • NECK: trachea midline, edema of neck and jaw • RESPIRATORY: clear to auscultation bilaterally • CARDIOVASCULAR: normal rate, regular rhythm, no murmurs • ABDOMEN/GI: soft, slight tenderness in epigastric region, no rebound • MUSCULOSKELETAL: no joint swelling, ROM preserved, trace LE edema • SKIN: no rashes Initial Laboratory Data 23 286 22.28 52 133 92 16 136 3.4 32 0.75 Lipids: Tchol 418, Trig 118, LDL 244, HDL 136 Urinalysis: 3+ blood, 3+ protein Protein/creatinine ratio 19.7 LP – Opening pressure of 31mmHg, otherwise normal Non-contrast head CT – slit ventricles, otherwise normal 1.4 20 5.4 59 0.8 27 1.0 CT Venogram – superior sagittal and straight sinus thrombosis and … Bilateral transverse sinus thrombosis CT venogram venous thrombosis of the superior sagittal sinus, bilateral transverse sinuses, and the straight sinus. The Anticoagulation Obstacle • • • • Baseline PTT 27. Started heparin drip at 6pm. 430am – PTT 36 1030am – PTT 36 130pm – anti-Xa heparin activity assay 0.05 (therapeutic range 0.5-0.7) • 6pm – anti-Xa activity 0.55 – therapeutic! • An initial therapeutic heparin drip rate was 1700U/hr. Several days later, this was decreased to 1200U/hr. At that time, her proteinuria had resolved on high dose steroids. A Happy Ending! • A complete work-up for other predisposing factors contributing to thrombosis was negative • Duplex scans of renal arteries, veins and vessels of the legs and arms all negative • MRI of the brain negative for infarction • Her headache resolved, and she was discharged on subcutaneous enoxaparin with no residual neurological deficits. Nephrotic Syndrome and Venous Thrombosis • In adults with nephrotic syndrome, there is an absolute risk of venous thromboembolism at 1.02% per year. • Risk of VTE is especially great in the first 6 months, approximately 9.85%! • With nephrotic syndrome there is increased prothrombotic factors (fibrinogen, factor VII, platelet adhesions), decreased antithrombotic factors (antithrombin, protein C and S levels) • Heparin complexes with antithrombin, increasing its inactivation of factors II and X. • In nephrotic syndrome, lower circulating antithrombin, results in decreased responsiveness to heparin References • Glassock R. Prophylactic Anticoagulation in Nephrotic Syndrome: A Clinical Conundrum. Circulation 2008; 117:224-30 • Mahmoodi B, et al. High Absolute Risk and Predictors of Venous and Arterial Thromboembolic Events in Patients with Nephrotic Syndrome. J Am Soc Nephrol 2007; 18:2221-2225 • Sung S, et al. Central Venous Thrombosis In Patients with Nephrotic Syndrome: Case Reports. The Journal of Vascular Diseases 1999; 50: 427-432 Thank you! Annual Incidence of Types of Thromboembolism Among Patients with Nephrotic Syndrome The incidence of cerebral venous thrombosis in adults with nephrotic syndrome is extremely low and has not been quantified. Nephrotic Syndrome and AntiCoagulation • Other contributors – volume depletion, diuretic or steroid therapy, venous stasis, immobilization, activation of the clotting cascade • In nephrotic syndrome, LWMH preferred over warfarin because of unreliable kinetic in patient with hypoalbuminemia