Nephrotic/Nephritic presentation (Becky)
advertisement

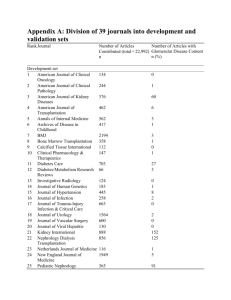
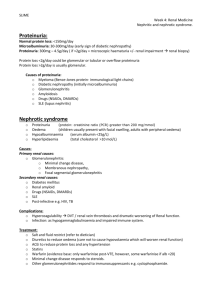
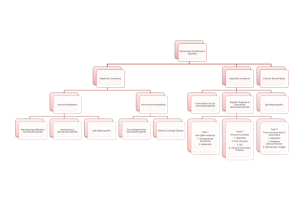
Glomerular Diseases Dr Rebecca Martin F2 Learning objectives 1. Appreciate the fact that glomerular diseases fall onto a wide spectrum 2. Be able to define the nephritic and nephrotic syndromes 3. Understand the pathology of 4 key glomerular diseases which serve as archetypal examples of nephritic and nephrotic syndrome 4. Know how to assess and manage a patient with suspected glomerular disease Exercise 1: Histology of the glomerulus Bowman’s Capsule Capillaries Endothelial cells Mesangium Podocytes (Foot processes) (GBM) Terminology Glomerulonephritis = inflammation of the glomeruli ‘Glomerulopathy’ is a more accurate term NEPHRITIC SYNDROME Collection of symptoms and signs associated with inflammatory glomerular disorders NEPHROTIC SYNDROME Collection of symptoms and signs associated with proliferative glomerular disorders • Haematuria • Hypertension • Oliguria • (Oedema) • Overt proteinuria (> 3.5g/24h) • Hypoalbuminaemia (< 30g/L) • Oedema Spectrum of glomerular diseases SLE IgA nephropathy Minimal change nephropathy Membranous nephropathy Diabetic nephropathy Post-infective glomerulonephritis Haematuria Proteinuria * Adapted from Davidson’s Principles and Practice of Medicine, 20th Edition Presenting features of glomerular disease SYMPTOMS • Asymptomatic • Fatigue, lethargy • Haematuria • Frothy urine • Swelling • Oliguria SIGNS • Hypertension • Oedema • Positive urine dipstick for protein/blood • Signs of related pathology Exercise 2: Glomerular diseases Match the conditions to their histological and clinical features Glomerular diseases CONDITION HISTOLOGICAL FEATURES CLINICAL FEATURES Minimal change nephropathy Usually normal histology Good response to steroids Membranous nephropathy Thickened GBM Commonest cause of nephrotic syndrome in adults IgA nephropathy Increased mesangial matrix Common cause of ESRF Post-infective glomerulonephritis Diffuse proliferation of endothelial/mesangial cells, infiltration by neutrophils Usually resolves spontaneously Glomerular diseases 1 Minimal change nephropathy - Commonest cause of nephrotic syndrome in children Accounts for 25% adult nephrotic syndrome Proteinuria usually remits on high dose steroids Does not progress to CKD Issues: nephrotic syndrome and complications of treatment Membranous nephropathy - Commonest cause of nephrotic syndrome in adults - 1/3 spontaneous resolution, 1/3 remain in nephrotic state, 1/3 progress to CKD - Watch and wait/steroids/cyclophosphamide Glomerular diseases 2 IgA nephropathy - Common cause of ESRF - Commonest cause of nephritic syndrome - Acute exacerbations can occur, particularly with respiratory infections - Mild variant associated with HSP in children - Poor response to immunosuppressive therapy Henoch-Schonlein Purpura • Systemic vasculitis • 3-10 years M:F 2:1 • Skin rash, arthralgia, abdominal pain • 40% glomerulonephritis (IgA nephropathy) Glomerular diseases 3 Post-infective glomerulonephritis - More common in children, now rare in developed world 10 day latency, usually after streptococcal throat infection Renal function improves spontaneously after 10-14 days Management by fluid and sodium restriction Rapidly progressive glomerulonephritis General term Extreme inflammatory nephritis Loss of renal function over days to weeks Biopsy can show necrotising lesions in glomerulus Goodpasture’s disease > SLE > IgA nephropathy. Diabetic nephropathy • • • • • Commonest cause of ESRF in UK 30% with T1DM develop after 20 years Poor glycaemic control strongest risk factor Microalbuminuria is earliest indicator Treatment with good glycaemic control and ACEi Thickening of GBM Microalbuminuria (Albumin: creatinine ratio > 2.5 M > 3.5 F) Increased mesangial matrix Nodular deposits Glomerulosclerosis and loss of glomeruli Heavy proteinuria Exercise 3: Case based discussion 24 year old male presents to medical outpatient clinic More tired than usual No systemic symptoms on questioning Only thing he has noticed is his urine is frothy Group 1: What else would you like to ask in the history? Group 2: What would you examine? Group 3: What investigations would you perform? Investigations in glomerular disease Bedside tests Urine dip Laboratory tests FBC, U&E, CRP, ESR, HbA1C, complement, ANCA, ANA, antidsDNA, anti-GBM, ASOT Urine microscopy, urine albumin:creatinine ratio, 24h protein Throat/skin swabs Imaging Renal ultrasound Invasive tests Renal biopsy Management of glomerular diseases • • • • • • • Refer to a nephrologist! Control hypertension (BP <130/80) Tight control of blood glucose if appropriate Restrict fluid and salt intake if proteinuria Watch and wait? Steroids? Immunosuppressants? Summary • • • • Nephritic and nephrotic syndromes Archetypal diseases for each Key investigations to perform Management principles Learning at home • Please link this evening’s learning to rheumatology teaching • SLE and Goodpasture’s disease (anti-GBM) are also causes of glomerulopathy • These are potential causes of rapidly progressive glomerulonephritis Thank you Any questions?