Nephrotic Syndrome..…(NS)
Prepared by:Mohammad Ali Al-shehri
…..
Supervised by :
Dr.
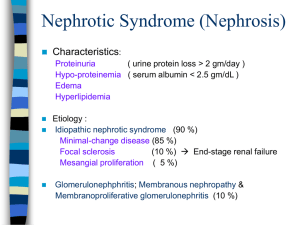
Nephrotic syndrome
Nephrotic syndrome (NS) results from increased
permeability of Glomeulrar basement membrane
(GBM) to plasma protein.
It is clinical and laboratory syndrome
characterized by massive proteinuria, which
lead to hypoproteinemia ( hypo-albuminemia),
hyperlipidemia and pitting edema.
(4-increase,
1-decrease).
Nephrotic Criteria:*Massive proteinuria:
qualitative proteinuria: 3+ or 4+,
quantitative proteinuria : more than 40 mg/m2/hr in
children (selective).
*Hypo-proteinemia :
total plasma proteins < 5.5g/dl and serum albumin : <
2.5g/dl.
*Hyperlipidemia:
serum cholesterol : > 5.7mmol/L
*Edema: pitting edema in different degree
Nephritic Criteria
-Hematuria: RBC in urine (gross hematuria)
-Hypertension:
≥130/90 mmHg in school-age children
≥120/80 mmHg in preschool-age children
≥110/70 mmHg in infant and toddler’s children
-Azotemia(renal insufficiency):
Increased level of serum BUN 、Cr
-Hypo-complementemia:
Decreased level of serum c3
Classification:
A-Primary Idiopathic NS (INS): majority
The cause is still unclear up to now. Recent 10 years
,increasing evidence has suggested that INS may result
from a primary disorder of T– cell function.
Accounting for 90% of NS in child. mainly discussed.
B-Secondary NS:
NS resulted from systemic diseases, such as anaphylactoid
purpura , systemic lupus erythematosus, HBV infection.
C-Congenital NS: rare
*1st 3monthe of life ,only treatment renal transplantation
Secondary NS
Drug,Toxic,Allegy: mercury, snake venom, vaccine, pellicillamine,
Heroin, gold, NSAID, captopril, probenecid, volatile hydrocarbons
Infection: APSGN, HBV, HIV, shunt nephropathy, reflux
nephropathy, leprosy, syphilis, Schistosomiasis, hydatid disease
Autoimmune or collagen-vascular diseases: SLE, Hashimoto’s
thyroiditis,, HSP, Vasculitis
Metabolic disease: Diabetes mellitus
Neoplasma: Hodgkin’s disease, carcinoma ( renal cell, lung,
neuroblastoma, breast, and etc)
Genetic Disease: Alport syn, Sickle cell disease, Amyloidosis,
Congenital nephropathy
Others: Chronic transplant rejection, congenital nephrosclerosis
Idiopathic NS (INS): Pathology: Minimal Change Nephropathy (MCN): <80%
The glomeruli appear normal basically Under Light
microscopy, and Under Immunofluorescence
*under Electron microscopy – fusion of the foot
processes of the podocytes
(2) Non—MCN: <20%
*Mesangial proliferative glomerulonephritis
(MsPGN): about 10%
*Focal segmental glomerulosclerosis (FSGS): 5%
*Membranous Nephropathy (MN) : 2%
*Membrane proliferative glomerulonephritis
(MPGN) : 1%
*Others: rare,Cresent glomerulonephritis
NB:-
*Nephrotic syndrome is 15 times more common in
children than in adults.
*Most cases of primary nephrotic syndrome are in
children and are due to minimal-change disease. The
age at onset varies with the type of nephrotic
syndrome.
Pathophysiology:
The Main Trigger Of primary Nephrotic Syndrome
and Fundamental and highly important change of
pathophysiology :Proteinuria
Pathogenesis of Proteinuria: Increase glomerular permeability for proteins due to loss of
negative charged glycoprotein
Degree of protineuria: Mild less than 0.5g/m2/day
Moderate 0.5 – 2g/m2/day
Sever more than 2g/m2/day
Type of proteinuria: A-Selective proteinuria: where proteins of low molecular
weight .such as albumin, are excreted more readily than
protein of HMW
B-Non selective :
LMW+HMW are lost in urine
pathogenesis of hypoalbuminemia
*Due to hyperproteinuria----- Loss of plasma
protein in urine mainly the albumin.
*Increased catabolism of protein during acute
phase.
pathogenesis of hyperlipidemia:*Response to Hypoalbuminemia → reflex to liver --→
synthesis of generalize protein ( including
lipoprotein ) and lipid in the liver ,the lipoprotein
high molecular weight no loss in urine →
hyperlipidemia
*Diminished catabolism of lipoprotein
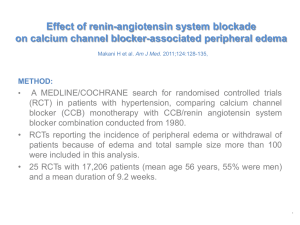
pathogenesis of edema: *Reduction plasma colloid osmotic pressure↓
secondary to hypoalbuminemia Edema and
hypovolemia
*Intravascular volume↓ antidiuretic hormone (ADH
) and aldosterone(ALD) water and sodium
retention Edema
*Intravascular volume↓ glomerular filtration rate
(GFR)↓ water and sodium retention Edema
How many pathological types causes
nephrotic syndrome?
Clinical Manifestation:IN MCNS , The male preponderance of 2:1
: 1.Main manifestations:
Edema (varying degrees) is the common symptom
Local edema: edema in face , around eyes( Periorbital swelling) , in
lower extremities.
Generalized edema (anasarca), edema in penis and scrotum.
2-Non-specific symptoms:
Fatigue and lethargy
loss of appetite, nausea and vomiting ,abdominal pain , diarrhea
body weight increase, urine output decrease
pleural effusion (respiratory distress)
Investigations: 1-Urine analysis:-
A-Proteinuria : 3-4 + SELECTIVE.
b-24 urine collection for protein
>40mg/m2/hr
for children
c- volume: oliguria (during stage of edema formation)
d-Microscopically:microscopic hematuria 20%, large number of hyaline cast
Investigations: 2-Blood:
A-serum protein: decrease >5.5gm/dL , Albumin levels are
low (<2.5gm/dL).
B-Serum cholesterol and triglycerides:
Cholesterol >5.7mmol/L (220mg/dl).
C-- ESR↑>100mm/hr during activity phase
.
3.Serum complemen: Vary with clinical type.
4.Renal function
Kidney Biopsy:-
Considered in:
1-Secondary N.S
2-Frequent relapsing N.S
3-Steroid resistant N.S
4- Hematuria
5-Hypertension
6- Low GFR
Differential Diagnosis of NS:
D.D of generalized edema: 1-Protein –losing enteropathy
2-Hepatic Failure.
3-HF
4-Protein energy malnutrition
5-Acute and chronic GN
6-urticaria? Angio edema
Complications of NS:1-Infections:Infections is a major complication in children with
NS. It frequently trigger relapses.
Nephrotic pt are liable to infection because :
A-loss of immunoglobins in urine.
B-the edema fluid act as a culture medium.
C-use immunosuppressive agents.
D- malnutrition
The common infection : URI, peritonitis, cellulitis and UTI
may be seen.
Organisms: encapsulated (Pneumococci, H.influenzae),
Gram negative (e.g E.coli
Complication …
Vaccines in NS;polyvalent pneumococcal vaccine (if not previously
immunized) when the child is in remission and off daily
prednisone therapy.
Children with a negative varicella titer should be given varicella
vaccine.
Complication…..
2-Hypercoagulability (Thrombosis).
Hypercoagulability of the blood leading to venous or arterial
thrombosis:
Hypercoagulability in Nephrotic syndrome caused by:
1-Higher concentration of I,II, V,VII,VIII,X and fibrinogen
2- Lower level of anticoagulant substance: antithrombin III
3-decrease fibrinolysis.
4-Higher blood viscosity
5- Increased platelet aggregation
6- Overaggressive diuresis
3-ARF: pre-renal and renal
4-
cardiovascular disease :-Hyperlipidemia, may be a risk
factor for cardiovascular disease.
5-Hypovolemic shock
6-Others: growth retardation, malnutrition,
adrenal cortical insufficiency
Management of NS:
General (non-specific )
*Corticosteroid therapy
General therapy: Hospitalization:- for initial work-up and evaluation of
treatment.
Activity: usually no restriction , except
massive edema,heavy hypertension and infection.
Diet
Hypertension and edema: Low salt diet (<2gNa/ day) only
during period of edema or salt-free diet.
Severe edema: Restricting fluid intake
Avoiding infection: very important.
Diuresis: Hydrochlorothiazide (HCT) :2mg/kg.d
Antisterone : 2~4mg/kg.d
Dextran : 10~15ml/kg , after 30~60m,
followed by Furosemide (Lasix) at 2mg/kg .
Induction use of albumin:-
Albumin + Lasix (20 % salt poor)
1-Severe edema
2-Ascites
3-Pleural effusion
4-Genital edema
5-Low serum albumin
Corticosteroid—prednisone therapy:-
Prednisone tablets at a dose of 60 mg/m2/day (maximum
daily dose, 80 mg divided into 2-3 doses) for at least 4
consecutive weeks.
After complete absence of proteinuria, prednisone dose
should be tapered to 40 mg/m2/day given every other
day as a single morning dose.
The alternate-day dose is then slowly tapered and
discontinued over the next 2-3 mo.
Treatment of relapse in NS:
Many children with nephrotic syndrome will experience
at least 1 relapse (3-4+proteinuria plus edema).
daily divided-dose prednisone at the doses noted earlier
(where he has the relapse) until the child enters
remission (urine trace or negative for protein for 3
consecutive days).
The pred-nisone dose is then changed to alternate-day
dosing and tapered over 1-2 mo.
According to response to prednisone
therapy:
*Remission: no edema, urine is protein free for 5 consecutive
days.
* Relapse: edema, or first morning urine sample contains > 2 +
protein for 7 consecutive days.
*Frequent relapsing: > 2 relapses within 6 months (> 4/year).
*Steroid resistant: failure to achieve remission with
prednisolone given daily for 28 days.
Side Effects With Long Term Use of
Steroids “Steroid toxicity
-Stunted growth
Cataracts
hyperglycemia
myopathy
peptic ulcer
- Pseudotumor cerebri
poor healing of wound.
-Psycosis
Hirsutism
-Osteoporosis
Thromboembolism
- Cushingoid features
-Adrenal gland suppression
Alternative agent: When can be used:
Steroid-dependent patients, frequent relapsers, and steroid-
resistant patients.
Cyclophosphamide Pulse steroids
Cyclosporin A
Tacrolimus
Microphenolate
THE END….
THANK YOU….