nephrotic syndrome ( ns)1
advertisement

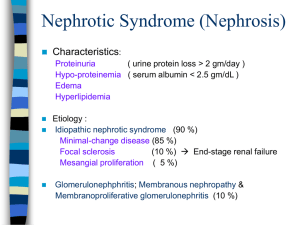
NEPHROTIC SYNDROME ( NS) Asist. prof. Magdalena Stârcea IVth Pediatric Clinic DEFINITION: pathogenic entity clinically manifested by edema and proteinuria biological> 50mg/kg/day in urine over 24 hours, hypoalbuminemia below 30g / l, dyslipidemia and hypercholesterolemia. After the last diagnostic guide KDIGO (Kidney Disease The: Improving Global Outcomes), nephrotic syndrome is clinical entity associated pathogenic edema, compared urinary protein / urinary creatinine ≥ 2000 mg / g, proteinuria ≥ 300 mg / dL, or 3 + on dipstick urine and hypoalbuminemia ≤ 2.5 mg / L. EPIDEMIOLOGY: 90% of cases of idiopathic nephrotic syndrome is primitive It affects children aged 2-10 years. It affects mainly males (but not exclusively!). Is 15 times more common in children than in adults. The incidence is 2-7 cases per 100 000 children under 16 years. Incidence of nephrotic syndrome corticorezistent seems to be in black race and hispanic population greater than in the general population. The Asian population is 6 times more affected than the European (as The Kidney Disease: Improving Global Outcomes - KDIGO). Congenital nephrotic syndrome have an increased incidence (1 / 10000-1 / in 5000 births) in the Finnish population. CLASSIFICATION: I. Primitive nephrotic syndrome Minimal (MCNS) ( 79 % cases) - is the most common form of NS in children, and its prevalence is inversely proportional to the age at onset. MCNS have the highest rate of responsiveness to standard therapy and the best long-term prognosis - - Chronic glomerulonephritis : segmental glomerulosclerosis and focal ( GSFS ) , membranous, glomerulonephritis , membranoproliferative glomerulonephritis (deposit IgM, IgG , IgA , complement) - Primitive congenital nephrotic syndrome ( Finnish type, Denys - Drash , Frasier , Schimke ) or secondary infections/ intoxications maternal-fetal or maternal, systemic disease (SLE, amyloidosis ) II. Secondary nephrotic syndrome : - Systemic diseases : SLE, Henoch- Schonlein purpura , sickle cell disease, hepatitis B / C , syphilis , malaria, chickenpox, AIDS , diabetes, amyloidosis , infections ventriculo - peritoneal shunt , endocarditis subacute thyroiditis Hashimoto - Metabolic diseases : Diabetes - Malignancies : lymphoma , neuroblastoma, carcinoma (rare) - Hereditary diseases : Alport - Drugs: gold salts , D -penicillamine , mercury , NSAIDs (diclofenac, etc) , ACE ( catopril , etc). - Others: Snake venom , injecting drugs (heroin ) poisoning with volatile aromatic hydrocarbons , vaccines ETIOLOGY: unclear, involving both genetic and immunological factors, and may not be shown exactly their role. - Genetic factors: have been identified gene belonging to HLADR7, and HLA-DQW2 in children with nephrotic syndrome. Podocinei mutations, a membrane protein encoded by the gene NPHS2 have been identified in cases of nephrotic syndrome with autosomal recessive corticorezistent, and sporadic cases. Nephrotic syndrome with GSFS was reported in patients with mitochondrial disease, Galloway-Mowat syndrome (nephrotic syndrome, microcephaly, hiatus hernia) and Schimke syndrome (nephrotic syndrome, primary immunodeficiency T cell line, dysplasia spondiloepifizară). - Immunological factors - demonstrate the increased expression of IL-2 receptor in patients with relapse of nephrotic syndrome and its receptor expression in the absence of remission. PATHOPHYSIOLOGY: the essential change is the increase in glomerular basement membrane permeability, which causes loss of protein in the urine (albumin, immunoglobulins, clotting factors, proteins transport of iodine, iron, vitamin D, etc.). Proteinuria arise in connection with the change of the glomerular basement membrane discharges, the reduction of sialic acid, heparan-sulfate neutralization of the membrane structure. Proteinuria is variable during the day, averaged over 40mg/m2/h. Hypoalbuminemia is secondary to renal losses, increased catabolism, decrease synthesis and digestive losses (through mucosal edema). Edema, the main clinical signs of nephrotic syndrome is caused by colloid osmotic pressure drop which causes extravasation in the interstitial water with intravascular space contraction and renal hypoperfusion. Secondary stimulation of the renin-angiotensin-aldosterone system, retention of Na and water (under the action of ADH). Secondary to hypoalbuminemia apears hypercholesterolemia and hypertriglyceridemia by increasing hepatic synthesis. An important complication NS thrombosis. Two mechanisms are involved in the etiology of thrombosis: decreased antithrombotic factors (urinary loss of antitrombină III, protein S and C) and increased prothrombotic factors (thrombocytosis, increased platelet adhesiveness and increase serum levels of factors V, VIII, von Willebrand factor, fibrinogen, etc). PATHOGENY: On light microscopy, glomeruli may be normal with normal capillary walls and normal cellularity. Swelling and vacuolation of epithelial cells and a slight increase in mesangial matrix are often observed. A mild mesangial hypercellularity may be noted as well as tubular lesions and interstitial fibrosis. Imunofluorescence are negative in MCNS. Ultrastructural changes are always present, involving podocytes and mesangial stalks. Podocyte foot process fusion is generalized and constant; its extent is closely related to the degree of proteinuria. The glomerular basement membranes are normal with no parietal deposits. The endothelial cells are often swollen. Mesangial alterations include mesangial cell hyperactivity, increased mesangial matrix, and occasionally granular, deposits located along the internal side of the basement membrane. These ultrastructural alterations are nonspecific and are probably related to massive proteinuria. Minimal change disease - glomeruli appear normal by light microscopy with no tubulointerstitial lesions EM -FUSION OF THE EPITHELIAL CELL PODOCYTES. NEPHROTIC SYNDROME DIAGNOSIS: HISTORY: - Family history: nephrotic syndrome or other familial nephropathy -Personal history: viral, bacterial, parasitic, recent vaccinations CLINICAL EXAMINATION Measurements: weight, height, temperature, TA, ingestion, diuresis 1. Debut: insidious, with pallor, loss of appetite, swelling (eyelid, labia, scrotum), oliguria and digestive disorders, tachycardia, abdominal pain, sometimes fever. - 2. Period status: - Edema dominate the clinical picture from localized edema to generalized edema, accompanied by ascites, pleural effusion. - Urine output falls below 1ml/kg/hour (oliguria). Renal function is generally preserved. - AP is usually normal. It is possible to have moderate increases in blood pressure in the early days of NS. - Moderate hepatomegaly, liver - soft consistency. - May be associated diarrhea, vomiting and abdominal pain due to swelling parietal association tract, which may be from low intensity to violent mimicking the acute abdomen surgery. - Respiratory disorders occur in case of pleurisy massive association infections asecensionarea diaphragm with massive ascites. - Rarely fever and clinical picture of sepsis with peritoneal starting point / respiratory / urinary - Specific rash systemic disease manifested by secondary SN - Behavior changes, anxiety Complications : 1. Thrombosis : occurring in 10 % cases of NS congenital up to 25 % of primitive NS. The risk of thrombosis increases with age, being higher in adolescents than in children. It is also higher in children with NS in SLE or other systemic disease secondary . This complication occurs on average in the first three months of disease onset . The most common are venous thrombosis in the veins within the renal vein, inferior cava vein and pulmonary vein thrombosis. Cerebral venous thrombosis is rare, as arterial thrombosis (axillary artery , mesenteric, subclavian , coronary rarely ). 2. Primitive peritonitis : occurs in 2-6% of children, most commonly caused by Streptococcus pneumoniae , Staphylococcus aureus, Escherichia coli. 3. Infections (cellulitis, viral infections, meningitis, oto-rhino-laryngeal infection, etc) - with an increased incidence of both onset and during immunosuppressive therapy (cortisone or other immunosuppressive drugs). They attributed the low level of IgG, urinary losses of factor B (involved in opsonization of encapsulated bacteria by activating the alternate complement pathway), modified T cell function and induced immunosuppression therapy. 4. Acute renal failure - occurs rarely (0.8 - 1% of onset of NS), being due to a glomerulonephritis rapidly progressive, renal vein thrombosis, acute interstitial nephritis (induced by antibiotic therapy or NSAIDs , diuretics), tubular necrosis acute (induced sepsis or severe hypovolemia) . METABOLIC BALANCE – aims diagnosis of NS, determining disease severity and type of NS ( primitive pure / impure , secondary) CBC: moderate anemia (inflammatory and deficiency, plus the loss of iron transport proteins), thrombocytosis, leukocytosis (in association with infections) Inflammatory syndrome: ESR, PCR, fibrinogen Total protein, electrophoresis and immunelectrophoresis: dramatic decrease of total proteins and serum albumin below 25g /l, decreased IgG and IgA levels, increased IgM level . Lipid profile: cholesterol, triglycerides, total lipids Renal urea, creatinine, GFR (by Schwartz formula) Urinary dipstick - highlights nephrotic proteinuria , hematuria association Urine culture in case of fever, urinary symptoms , leucocyturia , nitrite per strip 24 Hour Urine: level of proteinuria Report urinary protein / urinary creatinine over 2000mg / g Immunoassays for excluding secondary NS: HBsAg, HCV Ac, HIV, RBW. In case of association of hematuria - Addis test , report urinary calcium / urinary creatinine for hipercaciuria, erythrocyte morphology - excluding impure NS, hypercalciuria , CGN If existe signs of systemic disease with impure aspect of NS: ANA, lupus cells, RF, dsDNA, pANCA, cANCA, complement (C3 , C4) Abdominal ultrasound: highlights ascites, hepatomegaly, any processes manifested by NS secondary of tumor (lymphoma. Look for the permeability of the renal vein and caval system (using Doppler) . Chest X-ray and PPD (10 units) in case of suspicion of TB Echocardiography - in case of persistent hypertension , arrhythmia, congestive heart failure or signs of cardiac tamponade (massive pericarditis) The suspicion of thromboembolic complications: D-dimer, antithrombin III, protein S, protein C, fibrinogen Pulmonary perfusion scintigraphy reveals pulmonary thromboembolism. Cultures - blood cultures, urine culture, secretory otitis, hypopharyngeal aspirate DEXA, endocrinology and orthopedic exam after prolonged cortisone therapy for secondary osteoporosis assessment Renal biopsy has the following indications: Before initiation of therapy: 1. major indications: - Debut under the 6 months - Initial macroscopic hematuria without infection - important HTA + persistent microscopic hematuria and low complement 2. relative indications: - Onset between 6-12 months - HTA + persistent hematuria - Unassigned renal hypovolemia After therapy: - corticorezistant NS - Frequent relapses DIFFERENTIAL DIAGNOSIS 1. Extrarenal diseases associated with edema: - Angioedema - Protein-calorie malnutrition - Chronic liver disease - Endocrine - Heart failure 2. Chronic glomerulonephritis manifested by NS: - Segmental glomerulosclerosis and focal, macroscopic hematuria + / - hypertension and glycosuria (need renal biopsy) - Congenital NS: age <6 months (need renal biopsy) - Rapidly progressive glomerulonephritis: hematuria, hipocomplementemie (need renal biopsy) 3. Secondary SN - IgA nephritis, hepatitis, malaria, lymphoma, AIDS, amyloidosis, syphilis - NS associated medications: antiinflammatory, D penicillamine, salts of Au, heroin - NS associated toxins, allergens TREATMENT Objectives: - Complete remission - Relapse prevention - Treatment of acute complications or those related to long-term medication - Patient's quality of life Management of edematous patient: - Bed rest - need in case of important generalized edema - Diet – no salt, normoproteic, normocaloric, hypolipidaemic, hypoglucidic diet, imposed by dyslipidaemia associated with cortisone therapy. Oliguria is required fluid restriction (intake = 400 ml + diuresis) - Diuretic therapy: only recommended short courses at patient in preserved diuresis (in case of hypovolemia may precipitate acute interstitial nephritis or acute tubular necrosis) . Generally used loop diuretics (furosemide) 1-2mg/kg/dosis, after infusion of albumin /plasma. Spironolactone can be associated to the potassium - sparing effect. - Hypovolemia associating severe hypotension and tachycardia can be improved by albumin infusion 1g/kg (5ml/kg of 20% solution), infused slowly direct iv way, diluted with glucose 5% with BP control. A low serum albumin level is not an indication for albumin infusion! - Immunization: the live attenuated vaccines are contraindicated during cortisone therapy and at least 6 months thereafter . 1. Specific therapy Primitive NS: oral prednisone 5 mg/tb - One month coticoterapie attack: daily 60mg/m2/day (or 2mg/kg/day), - A month discontinuous, the same dose - 2 months - gradual dose reduction with 10mg/week up to 0.25 mg / kg and stop the therapy after 4 months. After ISKDC (International Study of Kidney Disease in Children ) Classic mode : Prednisone • 60 mg/m2/day (maximum 60 mg / day) 4 weeks • 40 mg/m2/la 2 days , 4 weeks Prednisone therapy should receive adjuvant, needed to counter adverse effects : - Gastric protector (protector or nhibitor mucosa proton pump ) - Calcium and vitamin D for osteoporosis - KCl - Antiplatelet agents - in situations of significant thrombocytosis Depending on the initial response to therapy evolutionary describes several forms: - Initial Responder: remission after 4 weeks of therapy - Rare relapse: relapse within 6 months of first remisune - Frequent relapses: two or more relapses within 6 months of first remisune - Steroid dependent after attack therapy - 4 week: relapse at the end of the attack or the onset of therapy staple - Initial steroid - resistant lack of response in the first 4 weeks after the onset - Secondary steroid - resistant: initial responder does not respond to therapy later, after first relapse - Nonresponder lack any response to therapy - Remission: Urinary protein removal under 4mg/m2/hour, or trace for 3 consecutive days Steroid-dependent nephrotic syndrome therapy 1. Oral therapy with cyclophosphamide at a dose of 2-3 mg / kg / day from 8 - 12 weeks can induce remission steroid-dependent nephrotic syndrome Precautions: - Reduce the dose to 50 % when neutrophils are between 1500 1000/mmc - Suspended therapy if neutrophils fall below 1000/mmc therapy and/or if occurs significant cytotoxicity (neutropenia, hemorrhagic cystitis, gonadal toxicity, rare secondary malignancies) 2. In steroid-dependent nephrotic syndrome can be used as second-line therapy: - Pulsterapie with MTP – 30mg/Kgbw/dailly - Cyclosporine A 3-5 mg / kg / day , in two divided doses, 3 years - Tacrolimus 0.05 - 0.1 mg / kg / day in 2 divided doses - Mycophenolate mofetil 24-36 mg / kg / day or 1,200 mg/m2 / day divided in 2 doses up to 3 years Follow-up therapy with cyclosporine dosing is done by initial serum 2 weeks after initiation of therapy , the optimal level of 50-100 nmol / l initially. During therapy is contraCy - grapefruit use and administration of macrolide antibiotics. Steroid-resistant nephrotic syndrome therapy Renal biopsy is necessary for classification. Subsequent regimens should be individualized according to histology. Patients receive supportive therapy associated immunosuppression. Steroid-resistant nephrotic syndrome involves risk of complications such as the progression to end-stage chronic kidney disease. The goal of therapy is to achieve remission and preservation of renal function. Three broad categories of treatments are available for Steroidresistant nephrotic syndrome: - immunosuppressive therapy include pulsterapie with MTP , calcineurin inhibitors , mycophenolate mofetil , alkylating agents - immunostimulatory therapy include levamisole - dose 2.5 mg / kg, up 150mg/zi. Effectiveness of therapy is determined by the maximum of 4 weeks. If 's success continues up to 3 years. Side effects include gastrointestinal upset, rash and severe neutropenia - supportive therapy includes treatment with inhibitors of angiotensin converting enzyme, angiotensin receptor (ARBs) and vitamin E. Protocol KDIGO recommends: - Therapy with calcineurin inhibitors (CyA , tacrolimus) if get full remisiunes - Extension of the calcineurin inhibitor therapy to 12 months if it was a partial remission after 6 months - Second-line therapy may be administered with low-dose prednisone (0.25 mg / kg / day) - In the absence of remision after one year can asssociate mycophenolate mofetil therapy or pulsterapie of MTP, or combinations of both immunosuppressive - Not recommended CTX therapy in steroid-resistant nephrotic syndrome - For relapse after complete remision resume therapy using oral corticosteroids or scheme under which there was previously used for remiosion. - Immunosuppressive doses and precautions are similar to those recommended for steroid-dependent nephrotic syndrome Management of complications Hypertension: - Sodium restrictions - Exercise - Weight loss if is associated obesity - First line therapy consists of inhibitopri angiotensin converting enzyme and angiotensin receptor Obesity: - Monitoring of BMI, stimulating sport for weight control - Decreasing doses of glucocorticoids / change medications Dyslipidemia: - Low- fat diet containing < 30 % of the daily calorie intake (saturated <10 % ) - Lipid-lowering statin class if the LDL cholesterol remains > 160mg/dl Infections are an important cause of morbidity and mortality in children with nephrotic syndrome. Streptococcus pneumoniae is the main bacteria involved in the genesis of peritonitis in patients with primitive NS. In this respect pneumococcal vaccination is recommended for all children with NS. Prophylaxis with varicella-zoster virus is also required in these children. In patients with onset varicella Acyclovir therapy is indicated. Immunization was repeated every 5 years. Live vaccines attenuated contraindicated during treatment with corticosteroids and at least 3 months after. Thromboembolism Up to 25 % of children with NS have thromboembolic complications. The risk seems to be greater in patients with Steroid-resistant nephrotic syndrome to those with corticosensibil NS. Specific therapy includes heparin, low molecular weight heparin and oral anticoagulants. During anticoagulant therapy encourage movement and contraindicate rest time EVOLUTION for NS with minimal damage: -1/3 patients had a single episode -1/3 patients have occasional relapses -1/3 patients become steroid dependent after attack period therapy PROGNOSIS - NS with minimal damage: favorable prognosis - NS with histological lesions - depends to the etiology, morphology and therapeutic response - Secondary SN: * good prognosis: allergic and toxic drug NS * poor prognosis systemic diseases References: 1. O. Brumariu, Florentina Cucer, Sindromul nefrotic, în Hematologie și nefrologie pediatrică, elemente practice de diagnostic și tratament, editura Junimea, Iași, 2008, cap. 5, pag. 226 – 228 2. KDIGO Clinical Practice Guideline for Glomerulonephrites, Chapter 3: Steroid-sensitive nephrotic syndrome in children, Kidney International Supplements (2012) 2, 163–171; 3. KDIGO Clinical Practice Guideline for Glomerulonephrites, Chapter 4: Steroid-resistant nephrotic syndrome in children, Kidney International Supplements (2012) 2, 172–176; 4. Nelson textbook of pediatrics - 18 ed. Behrman RE, Kliegman RM, Jenson HB: Nephrotic Syndrome, cap. 527, pag. 2190 – 2195, Saunders Elsevier, 2007. 5. Patrick H. Nachman, J. Charles Jennette, Ronald J. Falk, Primary Glomerular Disease, cap. 31, pag. 1100 – 1165, în BRENNER & RECTOR’S THE KIDNEY, ediția 9, , Saunders Elsevier, 2012. 6. Rees L., Brogan P., Bockenhauer D., Webb N., Glomerular disease, în Pediatric Nephrology, Oxford Specialist Handbooks in Pediatrics, second edition, cap. 9, pag. 181 – 224.