Soft Tissue Sarcoma
advertisement

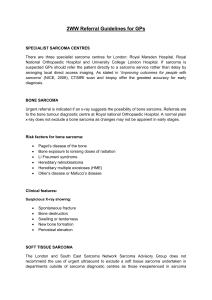
Management of Sarcomas Soft Tissue Sarcomas: A Multi-Disciplinary Strategy of Care Darin J. Davidson, MD, MHSc, FRCSC Department of Orthopaedics and Sports Medicine Assistant Professor, University of Washington School of Medicine Orthopedic Oncologist, Seattle Cancer Care Alliance October 25, 2014 Missoula, Montana CASE STUDY -- 62 year old male with right posterior arm soft tissue mass -Close approximation to radial nerve -Close approximation to humerus • Image guided needle biopsy- synovial sarcoma • Neoadjuvant chemotherapy – Pazopanib trial • Neoadjuvant radiation therapy – Planned positive margin on radial nerve and humerus • No increased risk of local recurrence • Preserve function Excision Negative margin Innervated latissimus flap to restore function Sarcoma: Multi-disciplinary Team • Treatment decisions not made independently by one specialty • Essential to have multidisciplinary discussion – Surgeon(s) – Radiation oncologist – Medical oncologist – Radiologist – Pathologist All have input into management of every case One modality may optimize management of another SCCA: Multi-disciplinary Sarcoma Program Medical Oncology Orthopaedic Oncology Radiation Oncology General Surgery Jones, Robin Conrad, Ernest ‘Chappie’ Kane, Gabrielle Mann, Gary Loggers, Elizabeth Davidson, Darin Kim, Edward Pillarisetty, Venu Pollack, Seth Lindberg, Antoinette Pathology Radiology Pediatrics Plastic Surgery Hoch, Ben Ha, Alice Hawkins, Doug Neligan, Peter How to contact us • Scheduling Contact: Leslie Fischer Telephone: 206.288.2018 Fax: 206.288.6996 Email: lfischer@seattlecca.org; pccsarcoma@seattlecca.org • Nursing Telephone: Email: 206.288.2018 sarcomarn@seattlecca.org Darin Davidson Telephone: Email: 206.543.3690 djdavi@uw.edu • Soft Tissue Sarcoma • Benign soft tissue masses much more common than malignant masses –Approximately 100:1 • Red flags for STS vs benign mass –Large (>5cm) –Deep to fascia • Age, presence of symptoms, duration not contributory Clinical Presentation And Assessment • Usually painless mass –Pain suggestive of neural origin, rapid growth • History- NF, sarcoma associated syndromes (Li-Fraumeni, Retinoblastoma) • Key on physical exam –Depth of lesion relative to fascia Imaging • MRI is preferred imaging modality • Sarcoma suggested by signal intensity heterogeneity – Imaging characteristics are not typical of particular type of soft tissue sarcoma – Fluid signal may be present in setting of necrosis or hemorrhage High grade soft tissue sarcoma with areas of hemorrhage and necrosis Management • Local and systemic staging –MRI of affected area –Biopsy –CT chest • Mainstay of treatment is surgical resection • Adjuvants –Radiation therapy –Chemotherapy Indications for Biopsy • Aggressive or malignant appearing bone or soft tissue lesions • Soft tissue mass- >5cm, deep to fascia or overlying bone or neurovascular structures • Except definitive imaging of benign mass (eg. lipoma) • Unclear diagnosis in symptomatic patient • Solitary bone lesion in a patient with a history of carcinoma • Even if fractured!! • Just need to confirm not sarcoma Biopsy Principles • An asymptomatic (latent) or symptomatic bone lesion (active) that appears entirely benign on imaging does not need a biopsy • A soft tissue lesion that appears entirely benign on MRI (lipoma, hemangioma) does not need a biopsy • When in doubt, it is safer to do a biopsy Biopsy Principles • Extensile incision – longitudinal in extremities • Tract needs to be excised • Avoid developing planes • Use involved compartment • Do not expose neurovascular structures • Meticulous hemostasis • Release tourniquet prior to wound closure • If using drain, bring out in line with incision • For bone lesions, ok to biopsy soft tissue mass • Frozen section Importance of the Biopsy • Whatever is exposed to the tumor is potentially contaminated and must be excised at definitive treatment • When biopsy principles aren’t followed – Increased risk of • Wrong diagnosis • Altered treatment • Altered outcome • Complications • Local recurrence of STS Mankin et al, 1996 Noria et al, 1996 Surgical Resection • Goal is complete resection of tumor with ‘adequate’ margin –Definition of adequate margin controversial –Use of preoperative radiation can affect extent of margin required • Marginal excision of STS- LR >30% • Marginal excision of STS after neoadjuvant XRT- LR <10% • Consideration for preservation of vital (major nerves, vessels, bone) structures to preserve function Gerrand et al, JBJS-B 2001 Radiation Therapy • Neoadjuvant XRT ‘sterilizes’ reactive zone surrounding the tumor –Allows for closer margin (still complete resection with negative margin) • Preserve critical structures and improve function • Neoadjuvant XRT uses lower dose (50 Gy) compared to postop (66 Gy) –Decreased fibrosis, edema (Davis et al, JCO 2002) –Decreased risk of radiation induced fracture (Holt et al, JBJS-A 2005) Overall survival comparing preoperative and postoperative XRT, indicating slightly higher overall survival in the preoperative group. O’Sullivan et al, Lancet, 2002 Radiation Therapy • The downside to neoadjuvant XRT –Higher risk of wound healing complications, infection –RCT of neoadjuvant vs adjuvant XRT (O’Sullivan et al, Lancet 2002) comparing wound healing complications requiring return to OR • Neoadjuvant XRT 35% • Adjuvant XRT 17% Radiation Therapy • Decision between neoadjuvant and adjuvant is balance of risks – Edema and fibrosis are not treatable and are disabling – Radiation associated fracture can be difficult to treat – Wound complications can be managed (may require prolonged treatment, multiple procedures) Local Control • Goal of local treatment is local control • Traditional predictors of local recurrence – Grade, size, depth • Competing risk model demonstrates margin status at resection is the most important predictor of local control (Biau et al, 2012) – Multi-modal local treatment Chemotherapy • Role of chemotherapy – Role in metastatic disease – Controversial for localized disease • Meta-analyses have shown slight survival advantage with chemotherapy Meta-analysis of adjuvant chemotherapy in localized soft tissue sarcoma Lancet , 1997 Hazard ratio of survival for meta-analysis of adjuvant chemotherapy in localized soft tissue sarcoma Pervaiz et al, Cancer 2008 Outcome • Outcome best considered on basis of initial disease –Localized disease • Superficial, low grade ≈ 100% 5 year survival • Deep, high grade ≈50% 5 year survival –Metastatic disease at presentation (Ferguson et al, Cancer 2010) • Pulmonary mets- 8% 5 year survival • Lymph node mets- 59% 5 year survival Soft Tissue Sarcoma Pitfalls • Soft tissue sarcoma grow quickly and are painful – Synovial sarcoma known for slow growth • Well circumscribed, smooth border of mass = benign and infiltrative, irregular border = sarcoma 47 year old male with well circumscribed mass; biopsy proven synovial sarcoma Fibromatosis Summary • Benign soft tissue masses are far more common than sarcoma, but beware –Large mass –Deep mass • MRI is imaging modality of choice • Biopsy principles essential • Surgical resection is mainstay of treatment of localized soft tissue sarcoma –XRT- consider advantages and disadvantages to preoperative vs postoperative –Chemotherapy- slight survival advantage