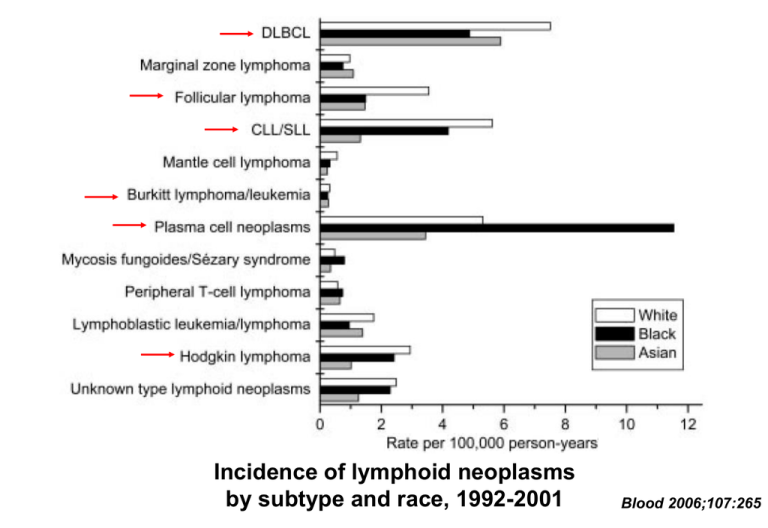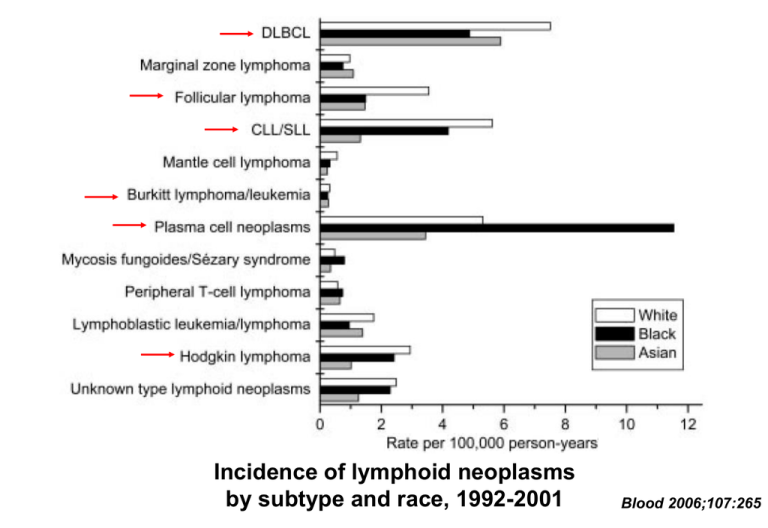
Incidence of lymphoid neoplasms
by subtype and race, 1992-2001
Blood 2006;107:265
CHRONIC LYMPHOCYTIC LEUKEMIA
• 25-30% of all leukemia in Western Hemisphere
• Rare at age < 40; incidence rises with age
• B-cell phenotype
About half of cases resemble “naïve” B-cells, half have
post-germinal center phenotype with mutated Ig Vh gene
Unmutated Ig Vh gene associated with worse prognosis
• Dx:
persistent, absolute lymphocytosis in blood &
marrow
Confirm clonal B-cell population via flow cytometry
• Most patients have diffuse lymph node involvement
Incidence of CLL/SLL by race, sex, and age, 1992-2001
Blood 2006;107:265
CHRONIC LYMPHOCYTIC LEUKEMIA
Smudge cell
Blood smear
Nodular marrow infiltration
Packed marrow
CHRONIC LYMPHOCYTIC LEUKEMIA
COMPLICATIONS
• Constitutional symptoms (fatigue)
• Anemia, thrombocytopenia
• Progressive lymph node enlargement
• Other organ infiltration
• Infection (bacteria, fungi, zoster, Pneumocystis)
• Autoimmune hemolysis/thrombocytopenia
• Transformation to aggressive lymphoma
• Other solid tumors (skin, lung, GI most common)
NEJM 1995;333:1052-1057
CHRONIC LYMPHOCYTIC LEUKEMIA
Treatment options
• Chlorambucil (25-35% overall response, 2-10% CR)
• Cytoxan, vincristine, prednisone (CVP)
• Nucleoside analogs (fludarabine, cladribine)
– Response rates higher than chlorambucil but overall
survival similar; somewhat more toxic
• Rituximab, other immunotoxins
• More aggressive chemotherapy for refractory
•
•
disease
IVIG for hypogammaglobulinemic patients with
recurrent infection
No advantage to treating asymptomatic disease
Fludarabine Compared with Chlorambucil as Primary
Therapy for Chronic Lymphocytic Leukemia
NEJM 2000;343:1750
Event-free survival
Overall survival
Fludarabine Compared with Chlorambucil as Primary
Therapy for Chronic Lymphocytic Leukemia
NEJM 2000;343:1750
FLUDARABINE WITH SEQUENTIAL OR CONCURRENT RITUXIMAB
IN PREVIOUSLY UNTREATED, SYMPTOMATIC CLL
Blood 2003;101:6
Event free survival
Overall survival
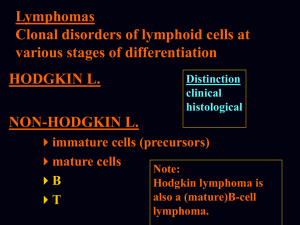
NON-HODGKINS LYMPHOMA
BIOLOGY
• Often associated with chromosome translocations
linking oncogene with immunoglobulin gene (B-cell
phenotypes) or T-cell receptor gene (T-cell
phenotypes)
• Etiology:
EBV, HTLV-1
Immunodeficiency states
Environmental (pesticides, etc)
Familial predisposition
Pagano JS. Viruses and lymphoma. NEJM 2002;347:78
NON-HODGKINS LYMPHOMA
CLASSIFICATION
• "Favorable" (indolent)
• Intermediate
• High-grade (aggressive)
NON-HODGKIN'S LYMPHOMA
INFORMATION USED IN CLASSIFICATION
• Morphology
• Immunohistochemistry
• Immunophenotype (flow cytometry)
• Cytogenetics
• Molecular features (gene expression, etc)
• Clinical setting
• Pattern of spread
Low-grade non-Hodgkin’s lymphomas
Small lymphocytic lymphoma/CLL
Follicular lymphoma
Intermediate- and high-grade non-Hodgkin’s lymphomas
Large B-cell lymphoma
Burkitt’s lymphoma
NON-HODGKINS LYMPHOMAS
"FAVORABLE" SUBTYPES
• Follicular (nodular) or diffuse histology
• Small, well-differentiated cells or small cleaved
cells
• Primarily B-cell phenotype
• Slow growth
• Usually advanced stage at presentation
• Asymptomatic patients may not need Rx
• Often good response to initial treatment
• High relapse rate (? incurable) but prolonged
survival possible
FOLLICULAR LYMPHOMA
• About 20% of all non-Hodgkin’s lymphoma
• Median age about 60; rare in young people
• Usually presents with widespread disease
– <20% stage I, 50% stage IV; 40-50% have
marrow involvement
• Typically CD20+, CD5-, CD10+
• t(14;18), overexpression of BCL-2 oncogene
Incidence of follicular NHL by race, sex, and age, 1992-2001
Blood 2006;107:265
SURVIVAL IN FOLLICULAR LYMHOMA
J Clin Oncol 23:5019-5026
NON HODGKINS LYMPHOMA
Treatment options for low grade disease
• Low dose alkylators (chlorambucil)
• Cytoxan, vincristine, prednisone (CVP)
• Nucleoside analogs (fludarabine, cladribine)
• Rituximab, other immunotoxins
• Local XRT
• More aggressive chemotherapy/ABMT for
•
refractory/transformed disease
No advantage to treating asymptomatic disease
Immediate treatment vs
watchful waiting in
asymptomatic patients
with advanced stage lowgrade NHL
Lancet 2003;362:516
CVP vs R-CVP in Advanced Follicular Lymphoma
Blood 2005;105:1417
NON-HODGKINS LYMPHOMAS
INTERMEDIATE SUBTYPES
• Diffuse histology (> 90%)
• Large cells or small cleaved cells
• B-cell or T-cell phenotype
• Moderate growth rates
• May present in extranodal sites
• 40-50% curable with combination
chemotherapy
Diffuse large cell lymphoma
• About 30% of NHL
• Median age about 65; can occur in young people
• About equal proportions of localized and
disseminated disease at presentation. Often
involves extranodal tissue
• CD20+
• t(14;18), t(8;14), t(3;14)
• Oncogenes: BCL-2, C-MYC, BCL-6
Incidence of B-large cell lymphoma by race, sex, and age, 1992-2001
Blood 2006;107:265
Comparison of a Standard Regimen (CHOP) with Three Intensive
Chemotherapy Regimens for Advanced Non-Hodgkin's Lymphoma
NEJM 1993;328:1002
Time to treatment failure
Overall survival
CHOP vs CHOP + rituximab in elderly patients with
large B-cell lymphoma
J Clin Oncol 2005;23:4117
Event-free survival
Overall survival
Initial Treatment of Aggressive Lymphoma with High-Dose
Chemotherapy and Autologous Stem-Cell Support
N Engl J Med 2004;350:1287
Event-free survival
All patients
“High intermediate” risk pts
NON-HODGKINS LYMPHOMA
AGGRESSIVE SUBTYPES
• Blastic morphology
"small non-cleaved" = Burkitt's
lymphoblastic
• Propensity for marrow, blood, CNS
involvement
• Rapid growth
• Cure possible with aggressive combination
chemotherapy
BURKITT LYMPHOMA
• <1% of NHL
• Median age 31; some cases in children
– Same as L3 ALL
• Most present with localized disease, about 40% with
disseminated disease. Extranodal involvement common
(up to 80% of pts)
• Very fast-growing, most have high LDH
• CD20+, CD10+, CD5-, tdT• t(8;14), t(2;8), t(8;22) with overexpression of C-MYC
Incidence of Burkitt lymphoma by race, sex, and age, 1992-2001
Blood 2006;107:265
NON-HODGKINS LYMPHOMA: SURVIVAL VS TIME
% SURVIVING
100
INTERMEDIATE & HIGH GRADE
LOW GRADE
0
10 yrs
Survival patterns in NHL - 1
ALCL, anaplastic large T/null-cell lymphoma; MZ, MALT,
marginal zone B-cell lymphoma of mucosa-associated
lymphoid tissue; FL, follicular lymphoma
Blood 1997;89:3909-3918
Survival patterns in NHL - 2
MZ, nodal, marginal zone B-cell lymphoma of nodal type; LP,
lymphoplasmacytoid lymphoma; SL, small lymphocytic lymphoma
Blood 1997;89:3909-3918
Survival patterns in NHL - 3
Med LBC, primary mediastinal large B-cell lymphoma; DLCBL,
diffuse large B-cell lymphoma; HG, BL, high-grade B-cell Burkittlike lymphoma
Blood 1997;89:3909-3918
Survival patterns in NHL - 4
T-LB, precursor Tlymphoblastic lymphoma; PTCL, peripheral Tcell lymphoma; MC, mantle cell lymphoma.
Blood 1997;89:3909-3918
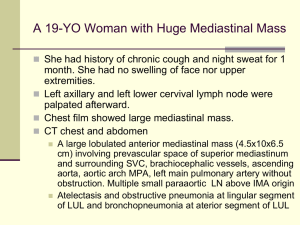
HODGKIN’S DISEASE
Cervical lymphadenopathy
Hilar and mediastinal
lymphadenopathy
Hodgkin’s disease: ReedSternberg cell (blue arrow)
and Hodgkin’s cell (red arrow)
in marrow biopsy
HODGKIN'S DISEASE
EPIDEMIOLOGY
• Annual incidence in US: 5-7 cases/100,000
persons
• Median age approx 30 yrs
• Bimodal age distribution
• More common in upper socioeconomic strata
• Role of EBV in pathogenesis
NEJM 2003; 349:1324
Incidence of Hodgkin lymphoma by race, sex, and age, 1992-2001
Blood 2006;107:265
HODGKIN'S DISEASE
BIOLOGY
• Virtually all cases originate in lymph nodes
• Most present with supradiaphragmatic disease
• Initial spread to adjacent node groups
• Immune response to tumor
Non-malignant lymphocyte infiltration
Fibrosis/sclerosis
Constitutional signs
HODGKIN'S DISEASE
STAGING
I - single node or group of contiguous nodes
II - two node groups, same side of diaphragm
III - nodes (or spleen), both sides of diaphragm
IV - extranodal (other than by direct extension)
(liver, marrow, lung most common)
"B" symptoms: fever, weight loss, night sweats
HODGKIN’S DISEASE
Potential sites of lymphatic spread
HODGKIN'S DISEASE
TREATMENT
• Stage I or IIA: radiotherapy or combined
modality (chemo + local XRT)
• Stage IIB or greater: combination
chemotherapy (ABVD, etc)
• Bulky tumors may require both modalities
• Cure rates > 70-80% possible
Lancet 2003;361:943
Lancet 2003;361:943
Long-term cause-specific mortality in patients treated for
Hodgkins disease
J Clin Oncol 2003;21:3431
PLASMA CELL DYSCRASIAS
CLASSIFICATION
• Monoclonal gammopathy of uncertain
significance (MGUS)
"Benign"/idiopathic
Associated with other diseases (autoimmune,
infectious, non-heme cancer, etc)
• Plasma cell or lymphoid malignancy
Waldenstrom's macroglobulinemia
Other lymphoproliferative disorders
Smoldering multiple myeloma
Multiple myeloma
Incidence of plasma cell neoplasm by race, sex, and age, 1992-2001
(predominantly multiple myeloma)
Blood 2006;107:265
MONOCLONAL GAMMOPATHY
COMPLICATIONS
• Hyperviscosity (IgM >> IgA > IgG)
• Renal dysfunction (light chains)
Glomerular
Tubular
Neuropathy
Other organ damage (rare)
Cryoglobulinemia (types I and II)
Amyloidosis
•
•
•
•
CRYOGLOBULINEMIA IN IgM GAMMOPATHY
Brit J Haematol 2004; 124:565
MULTIPLE MYELOMA – BONE MARROW ASPIRATE
MULTIPLE MYELOMA
Serum and urine protein electrophoresis
Monoclonal IgG
Serum
Urine
Free light chain
MULTIPLE MYELOMA
Lytic bone lesions
Nephropathy
MULTIPLE MYELOMA
EPIDEMIOLOGY
• Incidence in US approx 3 cases/100,000/yr
• 98% of cases > 40 yrs old
• Risk factors:
genetic
radiation exposure
? chemical exposure
MULTIPLE MYELOMA
CLINICAL MANIFESTATIONS
• Anemia progressing to pancytopenia
• Bone pain/destruction
• Hypercalcemia
• Humoral immune defect
• Local effects of plasmacytomas
• Systemic effects of paraprotein
MULTIPLE MYELOMA
DIAGNOSIS
• Monoclonal paraprotein
Intact immunoglobulin in serum (SPEP)
Light chains in serum or urine (IEP)
• Marrow plasmacytosis (> 20% - may be patchy)
• Lytic bone lesions
• Plasmacytoma
MULTIPLE MYELOMA
INDICATIONS FOR TREATMENT
• Symptomatic disease
• Bone destruction
• Anemia
• Organ dysfunction
• Hypercalcemia
• Increasing paraprotein
microglobulin level
or ß2-
MULTIPLE MYELOMA
TREATMENT
• Initial treatment: alkylating agent +
prednisone
• Alternative: vincristine, adriamycin +
dexamethasone (VAD)
• High dose cytoxan, thalidomide for relapsed
or refractory disease
• Proteasome inhibitor (bortezomib)
• Median survival 3-4 yrs; essentially no cures
with chemotherapy alone
• Auto-BMT prolongs survival
• Allo-BMT has curative potential for younger
pts
Overall and progressionfree survival in multiple
myeloma: standard
chemotherapy vs highdose chemotherapy with
stem cell rescue
NEJM 2003;348:1875
Proteasome inhibition