Orbital Lymphoma - University of Louisville Department of
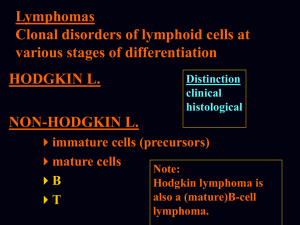
advertisement

Grand Rounds Conference Eric Downing MD University of Louisville Department of Ophthalmology and Visual Sciences Subjective CC/HPI: 77M referred by a local oncologist for a painless “bump” on RUL for 2 months. Pt had similar bumps on LUL in 2006, which were excised and identified as benign, per pt. History POH: lump removed over left eye, CEIOL OU, non-ischemic CRVO PMH: Throat cancer (2003) treated with 6 rounds of chemotherapy, multiple kidney stones (2012)TIA (2008), HTN Eye Meds: artificial tears Meds: Norvasc, ASA, Ativan Objective VA: Pupils: IOP: EOM: OD 20/70 4 19 full OS 20/20 4 21 full Objective SLE: E/L/L: Superotemporal mass under RUL, second mass under right nasolabial fold C/S: White, quiet OU K: Clear OU AC: Deep and quiet OU I/L: Round, PCIOL OU Hertel 18, 18 Differential diagnosis Benign lymphoproliferative disorder Metastatic lesion Inflammatory lesion Infectious lesion Epithelial tumor Assessment 57M with history of throat cancer (2003), treated with chemotherapy, previously in remission, who presented with a right superotemporal orbital mass for two months. Plan MRI with gadolinium Excision of masses with biopsy MRI T1 T2 Surgery Right orbitotomy with bone flap for lacrimal gland excisional biopsy Right nasolabial fold mass excision Pathology Biopsy: Follicular lymphoma, grade 3A CD 10, CD 20, BCL-2, and BCL-6 positive Ki67 positive in 30-40% of cells CD10, BCL-2: Follicular CD10/19/20/22/23: B cell Ki67 is a cell proliferation marker CD2/3/4/5/7/8/56: T-cell lymphoma Post-op Pt doing well VA OD improved slightly from 20/70 to 20/50 Release back to Dr. Woodcock for further workup/therapy Orbital Lymphoma Orbital lymphomas account for 8-15% of extranodal non-Hodgkins lymphomas MALT lymphomas are the most common (~50%), followed by the follicular type (~25%) Systemic involvement in approx 1/3 of cases 5 year survival rate approaches 100% for follicular lacrimal gland tumors, and 70% overall for extranodal marginal zone tumors Divided into 3 grades which refer to the number of centroblasts per HPF Pathophysiology Progressive clonal expansion of B, T, or NK cells due to mutations affecting the protooncogenes or tumor-suppressor genes Majority are non-Hodgkin B-cell lymphomas (90%) Often associated with infectious entities, such as Chlamydia psittaci Epidemiology Lifetime risk for NHL is 2% Typically affects elderly patients, with mean ages in the seventh decade Slight female predominance Asians/Pacific Islanders>whites>blacks Increases of >6% annually between 1975-2001 Increasing incidence, most likely due to better diagnostic techniques, the aging population, increased use of immunosuppressive drugs, and HIV/AIDS History & Physical Painless proptosis with or without motility deficits Ptosis Rarely have decreased VA If conjunctival, can have the characteristic salmon-patch appearance Cervical or preauricular lymphadenopathy, parotid gland swelling, or abdominal mass can portend systemic disease Work-up Labortatory studies CBC, RPR, ESR, LDH, FTA-Abs, HIV Lumbar puncture Imaging CT: seen as well-defined, high density, lobulated or nodular masses with sharp margins. Usually no bony erosion. Usually extraconal 10-17% involve the lacrima Imaging (con’t) MRI Decreased ability to evaluate for bony destruction May miss conjunctival disease T1: isointense T2: hyperintense PET Best to check for systemic/nodal involvement Higher sensitivity than CT (86% vs. 72%) Biopsy and Histopathology Essential to confirm diagnosis Histology and immunophenotype Grading Monoclonal------>Polyclonal 20%--------->60% risk of systemic disease Treatment Radiotherapy is the treatment of choice (97-100% local control) Surgery is usually NOT recommended due to their infiltrative nature Systemic disease Dose of 20-40 cGy Low-grade generally refractory to chemotherapy, but often have a long survival rate, even if untreated Aggressive lesions are treated with radiation and chemotherapy—often Methotrexate +/- procarbazine, vincristine, thiotepa Intralesional Rituximab for low-grade lymphomas (Savino) Complications of radiotherapy: conjunctivitis, cataract, dry eye, corneal ulcer, NVG, optic neuropathy Follow up Every 6 months for 2 years with repeat imaging Annually thereafter Prognosis Decreases with systemic involvement and/or bilateral disease Major factors Anatomic location Stage at presentation Subtypes (ENMZ(0-20%)>FL(20-37%)>MCL(38100%>LPL(14-100%) Immunohistochemical markers 20-25% will develop disseminated disease within 5 years ENMZ: extranodal marginal zone, FL: follicular, MCL: mantle cell, LPL: lymphoplasmatic Research Analyzed scans of 23 patients with either orbital lymphoma or IgG4 disease All patients underwent both MRI and Diffusionsensitised driven-equilibrium prep (DSDE) Used an apparent diffusion coefficient to differentiate Lymphoma has a lower ADC than IgG4 tissue, appearing darker, and giving us an additional modality to differentiate the two MRI images DSDE images Lymphoma IgG4 disease References 1. 2. 3. 4. 5. BCSC: Orbit, Eyelids, and Lacrimal System. Pp79-84 Rasmussen P, Ralfkiaer E, Prause JU, et al. Malignant Lymphoma of the Lacrimal Gland. Arch Ophth. 2011 Oct. Vol 129(10):1275-1280. Eckardt et al. Orbital Lymphoma: diagnostic approach and treatment outcome. World Journal of Surgical Oncology. 2013. 11:17 Savino G, Battendieri R, Gari M, et al. Long-term outcomes of primary ocular adnexal lymphoa treatment with intraorbital rituximab injections. J Cancer Res Clin Oncol. 2013; 139(7):1251-5 Hiwatashi A, Yoshiura T, Togao O. Diffusivity of intraorbital lymphoma vs IgG4 related disease: 3D turbo field echo with diffusion-sensitised driveequilibrium preparation technique. Eur Radiol. 2014, 24:581-586