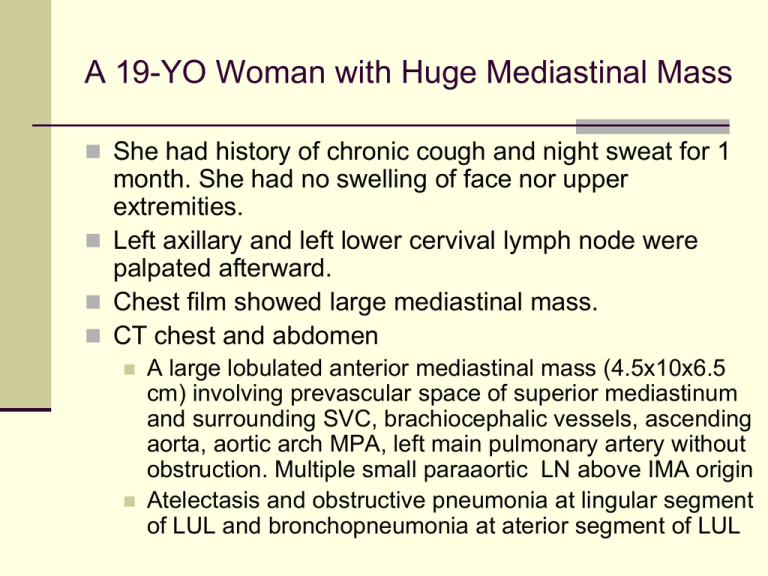
A 19-YO Woman with Huge Mediastinal Mass
She had history of chronic cough and night sweat for 1
month. She had no swelling of face nor upper
extremities.
Left axillary and left lower cervival lymph node were
palpated afterward.
Chest film showed large mediastinal mass.
CT chest and abdomen
A large lobulated anterior mediastinal mass (4.5x10x6.5
cm) involving prevascular space of superior mediastinum
and surrounding SVC, brachiocephalic vessels, ascending
aorta, aortic arch MPA, left main pulmonary artery without
obstruction. Multiple small paraaortic LN above IMA origin
Atelectasis and obstructive pneumonia at lingular segment
of LUL and bronchopneumonia at aterior segment of LUL
CT Image of Neck
and Chest
Pretreatment FDG-PET/CT Image
Echocardiography
Good LV contraction, LVEF 65.1%, no LA
dilatation, no significant valvular dysfunction
No abnormal wall motion. No intracardiac
shunt, no intracardiac mass, normal
pericardium, no pericardial effusion
Lymph Node Tissue Diagnosis
Lymph node biopsy, left cervical group
Diffuse large B-cell lymphoma, anaplastic
variant
Some resembling Hodgkin or Reed-Sternberg
cells
Lymphoma cells mark distinctly with CD20, not
CD3 or EMA. Some mark with CD30
Bone marrow biopsy
Negative for lymphoma cells
High LDH 1037 U/L (N 225-450), ECOG 2
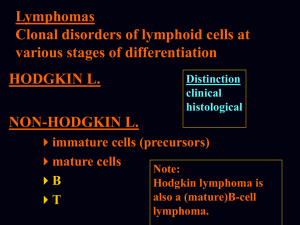
Diffuse Large B-cell Lymphoma: At
Least Three Disease
Activated
Germinal Center
B Cell-like
B Cell-like
(GCB DLBCL) (ABC DLBCL)
Cell of
origin
Germinal
center
Oncogenic
Mechanisms
cell
•B
BCL-2
Translocation
• C-rel
amplification
Favorable
59% 5-yr
survival
Clinical
outcome
Primary Mediastinal
B Cell
Lymphoma (PMBL)
? Post-germinal
? Thymic B cell
Center B cell
Constitutive
activation
Of NF-kB
Chr. 9q24
Amplification
PDL2
Poor
30% 5-yr
survival
Favorable
64% 5-yr survival
Primary Mediastinal B-Cell
Lymphoma (PMBL)
Large cells with polymorphic nuclei that have an
abundant rim of clear cytoplasm. Fibrosis commonly
results in compartmentalization of the neoplastic cells
Immunophenotyping demonstrates the presence of Bcell antigens in all cases (CD19, CD20, CD22 and
CD79a).
Bcl-2 is expressed in 80% of cases,
CD10 is infrequently expressed and CD21 is negative.
Surface immunoglobulin (sIg) expression is absent,
CD30 staining is common, but weak.
In contrast to HL, the transcription factors PAX5,
BOB.1, Oct-2 and PU.1 are always expressed and CD15
is negative.
Haematologica 2008;93:1364-71.
Comparison of DLBCL and PMLBCL
DLBCL
PMLBCL
Median age (years)
55
35
Nodal/extranodal presentation
65%/35%
0%/100%
Sex distribution (M:F)
1:1
1:4
Stage I-II/III-IV
40%/60%
80%/20%
Bulky disease
30%
60%-70%
PMBL vs HL vs MGZL
Dunleavy K, et al. Gray zone lymphoma; better treated like Hodgkin lymphoma
or mediastinal large B-cell lymphoma. Curr Hematol Malig Rep 2012;7:241-7.
Diagnosis and Treatment
Diffuse large B-cell lymphoma, primary
mediastinal B-cell lymphoma stage IIIBX
IPI = 3 (LDH, stage, ECOG); Bulky
Treatment
R-CHOP-21 x 8 cycles
After CR, autologous stem cell transplantation
was done without prior radiotherapy
Interim PET after 2nd R-CHOP
A soft tissue density mass at left
anterosuperior mediastinum, 4.5x6.0 cm at
prevascular, paraaortic, AP window, lower
paratracheal to left hilar region; no cervical
lymphadenopathy
No FDG avidity at soft tissue density mass.
Mild FDG avidity at left hilar node (residual
tumor)
CT whole body after 4th R-CHOP
Decreased size of soft tissue mass at anterior
mediastinum, 3.7x1.9x3 cm. No pericardial
effusion
Decreased size of multiple lymph nodes at
left gastric, EG junction, paraaortic,
aortocaval, celiac region
PET/CT after 8th R-CHOP
No pathological size of lymph nodes in head and
neck regions, normal orbits and paranasal sinuses
No pulmonary mass or nodule. An ill-defined
isodensity mass in anterosuperior mediastinum
(5x2.8 cm) occupying in prevascular space,
paraaortic and AP window
No demonstrable mass or cyst or fluid in abdominal
and pelvic cavity
No demonstrable bony destruction
IMP: complete response, no active lymphoma
Haematologica 2008;93:1364-71.
The recommended first-line therapy is chemotherapy and radiotherapy (grade
B). An anthracycline-based chemotherapy with CHOP, MACOP-B or VACOP-B
is recommended (grade B)
Patients with an inadequate early response should be candidates for early
intensification with high-dose chemotherapy (grade C)
Patients with refractory or relapsed disease should undergo rescue programs
including intensive, non-cross-resistant debulking treatment followed, in
chemosensitive patients, by high-dose chemotherapy and ABMT (grade B).
Overall survival by chemotherapy subtype in the IELSG study of 426
patients with primary mediastinal large B-cell lymphoma (PMBL)
100%
HDS/ABMT, n = 44
80
3rd generation regimens, n = 277
60
40
CHOP, n = 105
P < .0001
20
0
2
4
426 pts
6
8
10
Haematologica 2002;87:1258-126
12
14
16
18 years
The Therapeutic Outcome with the Inclusion
of Radiation Therapy
Chemotherapy
subgroup
Patients who
achieved CR
after CHT
Conversions
to CR among
patients who
received RT
while in PR
Global CR
after
chemotherapy
and RT
First-generation
50/105 (49%)
14/21 (67%)
64/105 (61%)
Thirdgeneration
142/277 (51%)
76/90 (84%)
218/277 (79%)
High-dose
23/44 (53%)
10/13 (77%)
33/44 (75%)
215/426 (51%)
100/124 (81%)
315/426 (74%)
Overall
Haematologica 2002;87:1258-64.
Multivariate analysis of poor prognostic
factors influence OS
P-value
Exp (B)
95% Cl
Increasing age
0.0002
1.02
1.01-1.03
Male sex
0.02
1.49
1.05-2.12
Poor performance status
0.001
0.51
0.34-0.77
Advanced stage
0.004
0.57
0.39-0.83
Induction chemotherapy
0.0002
0.49
0.34-0.71
R-CHOP RT vs CHOP RT
Vassilakopoulos TP, et al. Rituximab, cyclophosphamide, doxorubicin, vincristine, and
prednisone with or without radiotherapy in primary mediastinal large B-cell
lymphoma: the emerging standard of care. The Oncologist 2012;17:139-49.
R-CHOP RT vs CHOP RT
Vassilakopoulos TP, et al. Rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone with or
without radiotherapy in primary mediastinal large B-cell lymphoma: the emerging standard of care. The
Oncologist 2012;17:139-49.
Comparative Outcome of 76 PMBL with R-CHOP
RT and 45 Historical Control with CHOP RT
Vassilakopoulos TP, et al. Rituximab, cyclophosphamide, doxorubicin, vincristine, and
prednisone with or without radiotherapy in primary mediastinal large B-cell
lymphoma: the emerging standard of care. The Oncologist 2012;17:139-49.
Leuk Lymphoma 2012; early online:1-7,
All Patients
Early Stage
Patients
Leuk Lymphoma 2012; early online:1-7,
Front-line ASCT in PMBL
OS
PFS
DFS
Rodriguez J, et al. Primary mediastinal large cell lymphoma (PMBL): frontline treatment with autologous stem cell
transplantation (ASCT). The GEL-TAMO experience. Hematol Oncol 2008;26:171-8.
A 30-YR Female with Bilateral Cervical
Lymphadenopathy
She had chronic intermittent fever with night
sweats for 3 months. Bilateral enlarged cervical
lymph nodes were palpated.
Physical examination revealed moderate
anemia without jaundice, bilateral cervical and
supraclavicular lymphadenopathy, and
palpable splenomegaly.
Cervical lymph node biopsy revealed classical
Hodgkin lymphoma, nodular sclerosis type.
CT whole body
Multiple matted LN at
bilateral supraclavicular
regions, right upper
paratracheal,
paraesophageal, subcarina,
intraabdominal cavity,
bilateral iliac regions
Hepatomegaly and
splenomegaly with multiple
splenic lymphoma nodules
Initial Laboratory Results
CBC : Hb 8.6 g/dl, WBC 4880/mm3 (N 75, band
15, L 6, M 2), platelet 295,000/mm3
ESR 75 mm/h
LDH 964 U/L (N 225-450 U/L)
Albumin 3.2 g/dl, Ca 8.5 mg/dl
Bone marrow study
Multifocal marrow necrosis with diffuse
myelofibrosis with abnormal medium to large
mononuclear cells marked with CD30+, CD20-,
CD3-, ALK-, CD15-
Diagnosis
Classical Hodgkin’s lymphoma, nodular
sclerosis
Stage IVBS
Advanced Stage with 4 risk factors
Hb < 10.5 g/dl
Stage IV
Albumin < 4 g/dl
Lymphocyte < 8%
Treatment
group
EORTC/GELA
GHSG
Limited stage
CS I-II without risk factors
(supradiaphragmatic)
CS I-II without risk factors
Intermediate
stage
CS I-II with ≥1 risk factors
(supradiaphragmatic)
CS I, IIA with ≥1 risk factors
CS IIB with risk factors C/D, but not A/B
Advanced stage
CS III-IV
CS IIB with risk factors A/B, CS III/IV
Risk factors
A large mediastinal mass
B age ≥50 years
C elevated ESR
>50 mm/h without B
symptoms;
>30 mm/h with B
symptoms
D ≥4 nodal areas
A large mediastinal mass
(>1/3 maximum horizontal chest
diameter)
B extranodal disease
C elevated ESR
D ≥3 nodal areas
GHSG, German Hodgkin Study Group
EORTC, European Organisation for Research and Treatment of Cancer
GELA, Groupe d’Etude des Lymphomes de l’adulte
Advanced Stage HL
Associated with failure rate 30-40% with
anthracycline polychemotherapy
Treatment
Evaluation of regimens comprising multi-agent
chemotherapy
Multiple consolidative strategies
Improved disease control
Higher Intensive regimens to increase
efficacy
BEACOPP-based regimen (GHSG)
standard BEACOPP
Escalated BEACOPP
BEACOPP-14
> 2000 patients treated: esc BEACOPP
CR: >90% (RT: 15-65%)
FFTF: 82-88%, 4-10 yr follow up
OS: 86-90%, 4-10 yr follow up
MDS/AML: 0.9%
Significant more hematological and infectious toxicity,
secondary leukemia/MDS, infertility
Hodgkin Lymphoma Advanced Stages
1.0
BEACOPP escalated
BEACOPP base
Probability
0.8
C/ABVD
0.6
Only alkylating agents
(1965)
0.4
0.2
No treatment
(1940)
0.0
0
1
2
3
4
5
6
7
Overall Survival (y)
8
9
10
Other intensive regimen
Standford V regimen and RT to any bulky
disease
Consolidation treatment
Consolidation RT
Patient with poor risk or residual lesions
Less toxic than ASCT
Supported by EORTC (MOPP/ABV IFRT) in PR
cases
Not recommended in PET-CR patients (GELA
H89, GHSG H15)
Autologous stem cell transplant (ASCT)
Only in very high risk patient
Not recommended in 1st CR patient
Risk Adapted Treatment
Assessing chemosensitivity by interim PET
Prognostic value of PET after 2 cycles of chemotherapy
(PET2)
PET2 – negative better FFS
High negative predictive value for disease progression
Low positive predictive value
Ongoing trial
2xABVD PET2+ BEACOPP-14 or EB; PET2-
ABVD or ABV (UK RATHL)
2xEB PET2+ 6xEB rituximab; PET2- 2x vs 6xEB
(GHSG HD18)
Gallamini A, et al. Early interim 2-[18F] Fluoro-2-deoxy-D-glucose positron
emission tomography is prognostically superior to international prognostic score
in advanced-stage Hodgkin’s lymphoma: a report from a joint Italian-Danish
study. JCO 2007;25(24):3746-52.
BEACOPPesc vs ABVD in advanced HL
3 Italian cooperative group
Michelangelo Foundation
The Gruppo Italiano di Terapie Innovative nei Linfomi
(GITIL)
The Intergruppo Italiano Linfomi (IIL)
Unfavorable and advanced HL patients (331 patients)
6x ABVD
4x BEACOPPesc/ 4x BEACOPPstd
For CR and VGPR pt 30 G IFRT
For <CR, relapse salvage with ifosfamide-based
and HDT/ASCT with BEAM
Viviani S, et al. NEJM 2011;365(3):203-12.
Better initial
control in
BEACOPP
No difference
in long-term
clinical
outcome
Viviani S, et al. NEJM 2011;365(3):203-12.
esc BEACOPP vs ABVD in early
unfavorable and advanced stage HL
4 published trials (2868 adult patients)
GHSG HD9 and HD14 from Germany
HD2000 and GSM-HD from Italy
PFS significantly longer for escBEACOPP
OS, not statistically significant
More toxicity in escBEACOPP than ABVD
Hematological, infection, AML/MDS
No differences in 2nd cancer, TRM or infertility
16-60 adult patients with unfavorable/
advanced HL benefited from escBEACOPP for
PFS, no difference in OS
Bauer K, et al. Cochrane Database of Systematic Reviews 2011, Issue 8.
Bauer K, et al. Cochrane Database of Systematic Reviews 2011, Issue 8.
Case continued
The patient was treated with ABVD x4
CT whole body after 4x ABVD
Much improvement of multiple lymph nodes
and masses
Small cervical, surpraclavicular nodes < 1 cm
No mediastinal mass
Multiple paraaortic node 1-1.7 cm
Normal live and spleen
No pelvic mass, no ascites
Before
After
ABVDx4
Case continued
Much improvement after 4 cycles of ABVD
Another 2 cycles of ABVD was added
PET/CT after completion of 6th ABVD was
done
No hypermetabolic or enlarged lymph node in
neck, chest and intraabdominal regions and
no abnormal uptake in the bony structure that
indicated no evidence of active lymphoma
Suggestive of hypermetabolic intramural
myoma at posterior fundus
Thank You for Your Attention