Case Study 5
advertisement
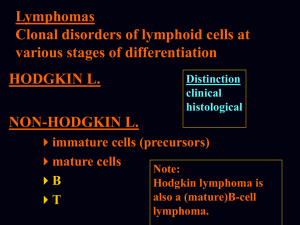
Case Study 5 Gabrielle Yeaney, M.D. Question 1 63-year-old female with progressive weakness of upper and lower extremities, in additiona to confusion, who is s/p CABG 2 years prior; history of smoking 2-1/2 packs a day for several years. Describe the MRI findings (location, enhancement, mass effect). MRI T2 FLAIR images MRI T1 pre and post contrast MRI side-by-side FLAIR and postcontrast images Answer Several abnormal FLAIR lesions are noted in bilateral cerebral peduncles, basal ganglia and deep white matter. Areas of enhancement include (1) left posterior limb of the internal capsule; (2) right basal ganglia; (3) deep and peripheral white matter of the right centrum semiovale posteriorly; (4) right cerebral peduncle (not pictured). There is no midline shift and no effacement of the sulci or ventricles. Question 2 Give a differential diagnosis based on MRI. Answer Lymphoma Metastasis Gliomatosis cerebri Infectious disease (Toxoplasmosis, Amebic encephalitis, Viral, PML) Demyelinating lesion (Multiple sclerosis) Multiple infarcts (Embolic / Vasculopathy) Question 3 A stereotactic biopsy of the left internal capsule is performed. Before you leave the OR, you ask the surgeon for additional clinical history. What might be helpful given what you know about the patient's history? Answer Given her age and history of smoking, it would be helpful to know if full body CT was performed and were there any masses. Also, is there any previous history of malignancy? An signs/symptoms of infection? What did CSF show? Did she receive any previous treatment (steroids)? Question 4 The surgeon tells you that a full body CT showed no masses, an HIV test was negative and the CSF showed lymphocytes. You receive 2 cores of tissue in consultation for intraoperative guidance. Describe the cytologic features of the touch prep and smear. Click here to view slides. Answer The smear is more cellular than normal white matter. Both the touch prep and smear show abundant large cells with high N:C, nuclear pleomorphism, clumped chromatin, multiple nucleoli. The tumor cells are dyshesive. There are several mitotic figures, apoptotic figures and lymphoglandular bodies. Question 5 What is your intraoperative diagnosis? (A. Neoplastic/Defer/Non-neoplastic, B. ________) Answer A. Neoplastic B. Lymphoma Question 6 What immunohistochemical studies would you get on the permanent sections to validate your diagnosis? Answer LCA, CD20/L26 & CD3. Other hematopoietic markers (ie CD79a, kappa, lambda, CD10, MUM-1, etc) and vimentin/GFAP (to highlight gliosis) might also be helpful in certain cases. Question 7 Review the permanent section and describe the microscopic features. Click here to view slide. Answer Neoplastic cells are arranged in sheets with foci of perivascular cuffing. The neoplastic cells are large-tomedium sized with atypical nuclear contours, moderate amphophilic cytoplasm, vesicular chromatin and multiple prominent nucleoli. There are frequent apoptotic figures and mitotic figures. Question 8 Review the following immunohistochemical studies and reticulin stain and give your interpretation. Click here to view slides. Answer Immunohistochemical studies show that the large atypical cells express CD20, LCA and BCL2. There are scattered small CD3-positive T cells in the background. GFAP highlights reactive astrocytes. Ki-67 shows a very high proliferation index (>95%). A reticulin stain highlights an increase in perivascular reticulin fibers in areas with tumor cells. Question 9 What is your final diagnosis? Answer (Primary) Diffuse large B-cell lymphoma or Large cell lymphoma, CD20-positive (previously known as reticulum cell sarcoma due to the bands of reticulin that form around vessel walls--see reticulin slide Q8). Question 10 Secondary involvement by lymphoma is most common in what part of the CNS? Answer Dura / leptomeninges Question 11 What is the most common type of primary CNS lymphoma? 1.Hodgkins lymphoma 2.Lymphoblastic lymphoma 3.T-cell lymphoma 4.Diffuse large B-cell lymphoma Answer Diffuse large B-cell lymphoma Question 12 What are some diseases associated with PCNSL? Answer HIV infection Immunosuppressive therapy (post transplantation) Hodgkin's disease Epstein-Barr virus Primary immunodeficiency syndromes: Wiskott-Aldrich, X-linked lymphoproliferative, Severe combined immunodeficiency, Ataxia-telangiectasia Question 13 True or False. Intravascular lymphomatosis affects multiple organ systems but rarely involves the CNS. Answer False Question 14 In a separate case, a 70-year-old woman who presented with two weeks of imbalance, right lower extremity weakness, decrease in taste, decrease in short-term memory, blurred vision on the left, and decreased hearing on the left. MRI showed an enhancing left posterior corona radiata lesion extending to the corpus callosum. She was placed on corticosteroids with improvement in her symptoms. Biopsy was done, and a diagnosis of primary central nervous system lymphoma (PCNSL) was rendered. Review this patient's biopsy. Note the differences from the previous case. What do you think caused the histologic differences in this patient compared to the previous case? Click here to view slides. Answer Cellularity is relatively lower, gliosis is more prominent and apoptotic figures abound in this biopsy. This case could easily be mistaken for infection or glioma without immunohistochemical studies to reveal the CD20-positive tumor cells. Why? This patient received steroids prior to surgery.