Hodgkin Lymphoma
advertisement
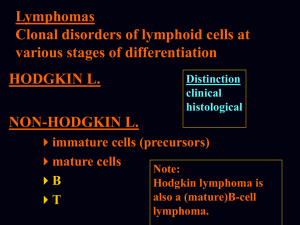
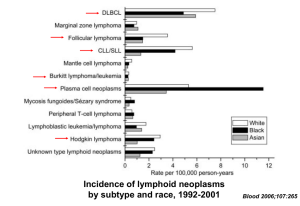
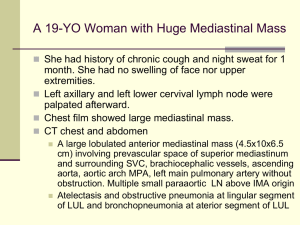
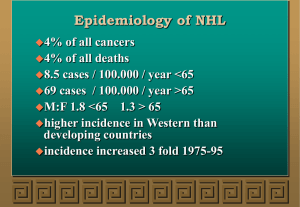
Goals • Understand the differences between Hodgkin Lymphoma and non-Hodgkin Lymphoma – Clinically and biologically • Understand the differences between aggressive NHL and indolent NHL – Clinically and biologically C Definition of Lymphoma • Heterogeneous group of lymphoproliferative malignancies – Results from clonal expansion of tumor cells derived from B, T, or NK cells – 85%-90% in the US are derived from B cells • Variable clinical presentations – Range from asymptomatic pick up on routine blood work to painless adenopathy to an emergent medical problem • Pain, failure to thrive, organ failure • Characterized by variable natural histories and therapeutic responses Age at Diagnosis for Hodgkin’s and Non-Hodgkin’s Lymphoma 120 ~56,390 NHL cases/y ~7,350 HD cases/y Cases/100,000 100 NHL 80 60 40 20 Hodgkin’s 0 0 5 10 15 20 25 30 35 40 45 50 55 60 65 70 75 80 85 Age at diagnosis (y) Data for diagnoses from 1997 to 2001. At: http://seer.cancer.gov. Accessed March 23, 2005. Estimated annual incidence Non-Hodgkin’s Lymphoma: Epidemiology United States 60,000 45,000 30,000 ~4% compound annual increase in incidence 15,000 0 1980 1985 1990 Year Adapted from Greenlee et al. CA Cancer J Clin. 2001;51:15. Adapted from Jemal et al. CA Cancer J Clin. 2005;55:10. 1995 2000 2005 Hodgkin’s Disease Hodgkin Biology • RS is a “crippled” germinal center B cell – does not have normal B cell surface antigens – micromanipulation of single RS followed by PCR demonstrates clonally rearranged, but non functional immunoglobulin genes • somatic mutations result in stop codon (no sIg) • no apoptotic death malignant transformation – unclear how this occurs; ? EBV – unclear how cells end up with RS phenotype Hodgkin’s Disease • Clinical features – Often seen in young adults – Wide variety of presentations • • • • • B symptoms (fevers, night sweats, wt loss) Pruritis Cough/SOB Pain Painless adenopathy Hodgkin’s Disease • Approach to the Patient – staging evaluation • • • • • • H&P CBC, diff, plts ESR, LDH, albumin, LFT’s, Cr CT scans chest/abd/pelvis bone marrow evaluation PET scan in selected cases Ann Arbor Staging System for Hodgkin's Disease and NonHodgkin's Lymphoma Stage I Stage II Stage III Stage IV Reprinted with permission. Adapted from Skarin. Dana-Farber Cancer Institute Atlas of Diagnostic Oncology. 1991. Hodgkin’s Disease • Typical staging results – Most often disease is localized to above the diaphragm – Common to have extensive mediastinal disease • Tends to spread to contiguous nodal groups – Unlike NHL Approach to the Patient • Hodgkin’s Disease – approach dictated mainly by where the disease is located rather (results of staging) than the exact histologic subtype • NHL – approach is often dictated more by the histologic subtype than the results of staging Hodgkin Lymphoma: Treatment of limited stage disease Hodgkin Lymphoma: Prognostic Factors Hodgkins Disease Summary • B cell lymphoma - several histologic subtypes - Generally does not affect the approach to the patient – Reed-Sternberg Cells • • • • • Tends to occur in young adults Mediastinal disease common Spreads to contiguous nodes Common to have a “localized” presentation Highly curable with current treatments Non-Hodgkin’s Lymphoma • 30ish histologic subtypes – B cell (85%), T cell, NK cell – Histologic subtype dictates the approach to the patient • Median age at diagnosis 60 • Often widespread disease at diagnosis • Wide variation in outcome – Some cases rapidly fatal – Some cases readily curable – Some cases incurable but patient can live for many years with good quality of life WHO Classification: B-Cell Malignancies Precursor B-cell neoplasm • Precursor B-lymphoblastic leukemia/lymphoma Mature (peripheral) B-cell neoplasms • B-cell chronic lymphocytic leukemia/ small lymphocytic lymphoma • Hairy cell leukemia • B-cell prolymphocytic leukemia • Plasma-cell myeloma/ plasmacytoma • Lymphoplasmacytic lymphoma • Follicular lymphoma • Splenic marginal-zone B-cell lymphoma • Mantle-cell lymphoma • Nodal marginal-zone lymphoma • Diffuse large B-cell lymphoma (DLBCL) • Extranodal marginal-zone B-cell lymphoma, mucosa-associated lymphoid tissue (MALT) type • Burkitt's lymphoma/Burkitt's cell leukemia • Blastic NK-cell leukemia Harris NL et al. J Clin Oncol. 1999;17:3835-3849. WHO Classification: T-Cell Malignancies Precursor T-cell neoplasm • Precursor T-lymphoblastic leukemia/lymphoma Mature (peripheral) T-cell neoplasms • T-cell prolymphocytic leukemia • T-cell granular lymphocytic leukemia • Subcutaneous panniculitis-like T-cell lymphoma • Aggressive NK-cell leukemia • Mycosis fungoides/Sézary syndrome • Adult T-cell lymphoma/leukemia (HTLV1+) • Primary cutaneous anaplastic large cell lymphoma, T/null cell • Extranodal NK/T-cell lymphoma, nasal type • Enteropathy-type T-cell lymphoma • Hepatosplenic gamma-delta T-cell lymphoma • Peripheral T-cell lymphoma, unspecified • Angioimmunoblastic T-cell lymphoma • Primary systemic anaplastic large cell lymphoma, T/null cell • Blastic NK lymphoma Harris NL et al. J Clin Oncol. 1999;17:3835-3849. B-Cell Development Stem cell Immature B cell s-IgM CD79a TdT HLA-DR HLA-DR CD79a CD22 CD21 CD20 CD34 Follicle-center B cell s-IgM/G/A CD22 CD10 bcl6 HLA-DR CD21 CD20 CD19 CD19 Pre-pre–B cell Immunoblast s-IgM/G/A TdT c-CD22 c-CD79a CD22 CD79a Mature B cell HLA-DR CD19 CD20 CD79a CD19 HLA-DR MUM1 CD22 CD10 TdT c-CD22 c-CD79a c-m HLA-DR CD21 HLA-DR Pre–B cell CD138± c-Ig s-IgM & IgD CD20 CD19 CD20 CD19 Plasma cell CD79a c-Ig Precursor cells Virgin (naïve) B cells Germinal-center and post–germinal-center B cells CD138 PCA-1 MUM1 Antigen Expression in BCell Lineage ALL Stem cell MCL, CLL Pre-B Early B Burkitts, FL, DLBCL Mature B Activated B WM Plasmacytoid B Germinal center Type of B cell lymphoma is a function of: 1) Where the cell was in development/maturation when it went “bad” 2) What molecular derangement occurred Jaffe. In: Non-Hodgkin’s Lymphoma. 1997:84. MM Plasma Models of Chromosomal Translocations in NHL REG CODING REG CODING REG CODING REG Protooncogene TRANSLOCATION REG CODING TRANSCRIPTIONAL DEREGULATION CODING Protooncogene TRANSLOCATION REG CODING FUSION PROTEIN REG = regulatory sequence. Harris NL et al. Hematology (Am Soc Hematol Educ Program). 2001:194-220. Chromosomal Translocations Commonly Associated With Activation in B-Cell Malignancies Oncogene Protein Translocation Disease bcl-1 Cyclin D1 t(11;14) MCL bcl-2 BCL2 (antiapoptosis) t(14;18) FL myc Transcription factor t(8;14) Burkitt’s NHL bcl-6 Zinc-finger transcription factor t(3;14) DLBCL (some follicular NHL) National Comprehensive Cancer Network. Practice Guidelines in Oncology. v.1.2005. Lymphoma Biology • Aggressive NHL – short natural history (patients die within months if untreated) – disease of rapid cellular proliferation – Potentially curable with chemotherapy • Indolent NHL – long natural history (patients can live for many years untreated) – disease of slow cellular accumulation – Generally incurable with chemotherapy NHL: Presentation and Staging • Aggressive NHL – Patients likely to present with symptoms • Indolent NHL – Patients likely to present with painless adenopathy • Initial workup similar to Hodgkin Lymphoma NHL: Approach to the Patient • Approach dictated mainly by histology – reliable hematopathology crucial • Aggressive NHL – Cure is often the goal • Indolent NHL – Cure is rarely the goal – Control is the goal Most Common NHLs Category Frequency (%) Diffuse large B-cell 31 Follicular 22 Marginal-zone B-cell, MALT 8 Peripheral T-cell 7 Small B-lymphocytic/CLL 7 Mantle-cell lymphoma 6 Primary mediastinal large B-cell 2 Anaplastic large T/null cell 2 High-grade B-cell, Burkitt-like 2 Marginal-zone B-cell, nodal 2 Precursor T-lymphoblastic lymphoma 2 Armitage JO, Weisenburger DD. J Clin Oncol. 1998;16:2780-2795. Follicular Lymphoma Approach to Indolent NHL • Indolent NHL: guiding treatment principle • immediate treatment does not prolong overall survival for many patients – When to treat? • constitutional symptoms • compromise of a vital organ by compression or infiltration, particularly the bone marrow • bulky adenopathy • rapid progression • evidence of transformation • Will often begin with relatively non-toxic treatments and escalate the intensity of the therapy Diffuse Large B Cell Lymphoma Approach to Aggressive NHL • Patients have the potential to be cured – Administer most effective therapy (no matter how harsh) at diagnosis – If not cured, patients typically die within a few years of diagnosis International Prognostic Index for Age-Adjusted Factor Adverse PS LDH Stage ≥2 >Normal III-IV Number of Factors Present 5-year DFS Age≤60 (%) 5-year OS Age≤60 (%) Low 0 86 83 Low-Intermediate 1 66 69 High-Intermediate 2 53 46 High 3 58 32 Risk Group The International Non-Hodgkin's Lymphoma Prognostic Factors Project. N Engl J Med. 1993;329:987-994. DLBCL: Subtypes Revealed by Expression Array Probability 1.0 Germinal-center B-cell–like 0.8 0.6 Activated B-cell–like 0.4 0.2 P = 7.9 E-6 0.0 0 Single histology with multiple molecular subtypes 2 4 6 8 Overall survival (years) 10 …with different outcomes Alizadeh AA et al. Nature. 2000;403:503-511. Summary • NHL incidence increasing • Hodgkin incidence stable or decreasing • Hodgkin Lymphoma – – – – – – – Characterized by the Reed-Sternberg Cells Stage more important that histologic subtype Often limited stage (stage I or II) Spreads to contiguous nodes Often affects younger patients Very responsive to therapy Cure rate quite high Summary • NHL cure rate mediocre – Many histologic subtypes • Often more important that the stage – indolent vs. aggressive • Function of underlying biology – indolent: • Often asymptomatic • Treatment: Less is more – aggressive: • Often symptomatic • require aggressive treatment ASAP to achieve cure