Pre Treatment Calcification of Hodgkin*s Lymphoma: A Case Report
advertisement
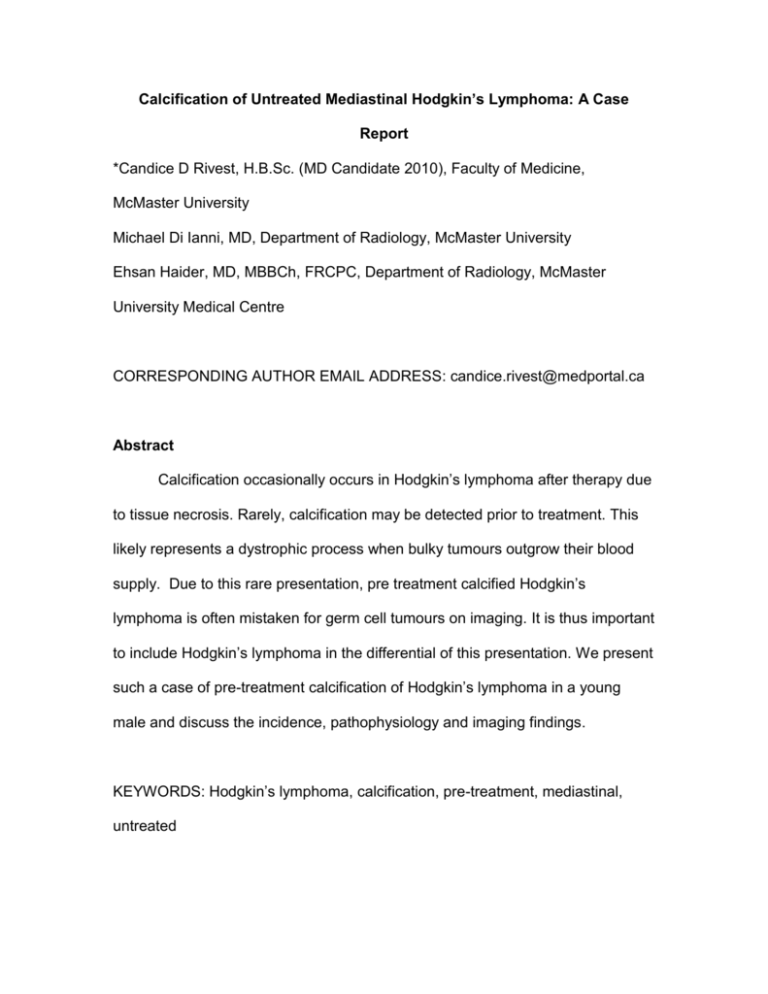
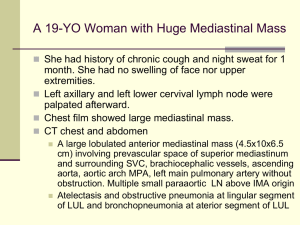
Calcification of Untreated Mediastinal Hodgkin’s Lymphoma: A Case Report *Candice D Rivest, H.B.Sc. (MD Candidate 2010), Faculty of Medicine, McMaster University Michael Di Ianni, MD, Department of Radiology, McMaster University Ehsan Haider, MD, MBBCh, FRCPC, Department of Radiology, McMaster University Medical Centre CORRESPONDING AUTHOR EMAIL ADDRESS: candice.rivest@medportal.ca Abstract Calcification occasionally occurs in Hodgkin’s lymphoma after therapy due to tissue necrosis. Rarely, calcification may be detected prior to treatment. This likely represents a dystrophic process when bulky tumours outgrow their blood supply. Due to this rare presentation, pre treatment calcified Hodgkin’s lymphoma is often mistaken for germ cell tumours on imaging. It is thus important to include Hodgkin’s lymphoma in the differential of this presentation. We present such a case of pre-treatment calcification of Hodgkin’s lymphoma in a young male and discuss the incidence, pathophysiology and imaging findings. KEYWORDS: Hodgkin’s lymphoma, calcification, pre-treatment, mediastinal, untreated Background Hodgkin’s lymphoma has an annual incidence of 2.8 out of 100,000 persons in the United States1. The World Health Organization (WHO) recognizes five subtypes of Hodgkin’s Lymphoma: nodular sclerosing, mixed cellularity, lymphocyte-rich, lymphocyte depleting, and lymphocyte predominate2. The former four encompass the classical type based on similar histological morphology which account for 95% of cases with the most common being nodular sclerosing (65-70%)1. The mean age at diagnosis is 38 years1. Case Presentation A 24 year old male presented to the Emergency Room complaining of shortness of breath that was ongoing for three weeks. The patient was using a budesonide/formoterol inhaler with no relief. His symptoms became worse when he lied on his right side and back. The patient was otherwise healthy and had no constitutional symptoms. He had a five year history of smoking and occasional alcohol use. On examination, the patient was afebrile with stable vital signs. There were no auscultatory findings on respiratory examination. There was palpable right supraclavicular lymphadenopathy. Abdominal and cardiac examinations were unremarkable. Laboratory examination revealed a decreased leukocyte count of 3.2 x 109/L with an absolute neutrophil count of 0.8 x 103/mm3. All other laboratory investigations were within the normal range. Chest radiographs showed a soft tissue density mass involving the right hilum and anterior mediastinum. Calcifications were not demonstrated radiographically. Figure 1: Chest radiograph showing a widened mediastinum Computed Tomography (CT) of the chest with intravenous contrast was performed which confirmed a large homogenous mass with soft tissue attenuation involving the anterior and middle mediastinum and right hilum. The mass contained a single, lobulated and coarse calcification measuring 12mm in diameter. The mass resulted in marked narrowing of the right main pulmonary artery and mild mass effect on the right mainstem bronchus. Bilateral supraclavicular, prevascular and pericardial adenopathy was also noted. There were no abnormalities seen in the upper abdomen. Figure 2: CT chest showing calcification (black arrow), mediastinal and hilar involvement of the mass (white arrows) Figure 3: CT chest showing narrowing of the right main pulmonary artery (white arrow) A needle core biopsy was taken from the right supraclavicular node suggesting the diagnosis of Hodgkin’s lymphoma of nodular sclerosing type. Immunohistochemistry for CD15, CD20, CD30 and fascin confirmed the diagnosis. Bone marrow biopsy was negative. Upon additional investigations including a CT of the abdomen and pelvis, a stage of 2A was assigned. The patient was referred to the Oncology service for therapy and is currently undergoing chemotherapy. Discussion Calcification in lymphoma is rare, occurring 1-5 years after chemotherapy or radiation therapy with an incidence of 2%3. This process has been shown to be associated with a good prognosis with 75% of patients being disease free 8 years after therapy3,4. In comparison, calcification before treatment in Hodgkin’s lymphoma is an even more rare finding, occurring in 0.4% of patients5-9. NonHodgkin’s Lymphoma has a higher rate of pre treatment calcification at 1%5,10. Even though the physiology of pre treatment calcification has yet to be established, two mechanisms have been proposed. The first mechanism is metastatic in nature resulting from an excessive serum concentration of unstable calcium ions11. Hypercalcemia can be caused by osteolytic metastases, tumor secretion of parathyroid hormone related protein, or by tumor production of calcitrol, which is the most common process occurring in lymphomas12. However, hypercalcemia in Hodgkin’s lymphoma is very rare with only one case reported in the literature13. A metastatic process is unlikely to be the cause of pre treatment calcification in our patient as his serum calcium concentration was within normal limits (2.47 mmol/L). The second potential mechanism is dystrophic calcification that is due to tissue necrosis. This occurs when excessive calcium enters the mitochondria of dying cells to form extracellular hydroxyapatite crystals. This process can occur in bulky tumors that outgrow their blood supply which present with multifocal areas of calcification6. It has been suggested that the nodular sclerosing type of Hodgkin’s Lymphoma may be more susceptible to calcification before and after treatment. In the reported cases of pre treatment calcified Hodgkin’s Lymphoma5-9, only one was found not to be of this type, but rather of mixed cellularity5. Predisposing factors include collagen fibrosis, cellular degeneration, and necrosis6. Awareness of this phenomenon is important as the finding of calcification might otherwise be used to exclude lymphoma from one’s differential diagnosis of an anterior mediastinal mass. In face, all four of the common anterior mediastinal masses (thyroid and thymic masses, germ cell tumors, and lymphoma) may present with calcification, thereby limiting this finding as a distinguishing feature14. A mediastinal mass in a young adult will most commonly be a germ cell tumor or Hodgkin’s lymphoma. The density, homogeneity, location, and degree of mass effect can help to differentiate between these two lesions6. References [1] SEER stat fact sheets [Internet]. Bethesda: National Cancer Institute; c19752006 [cited 2009 Feb 2]. Available from:http://seer.cancer.gov/statfacts/html /hodg.html. [2] Fritz A., ed., et al. International classification of diseases for oncology. 4th ed. Geneva: WHO; 2000. [3] Brereton HD, Johnson RE. Calcification in mediastinal lymph nodes after radiation therapy of Hodgkin’s disease. Radiology. 1974;112:705-707. [4] Bertrand M, Chen JT, Libshitz HI. Lymph node calcification in hodgkin’s disease after chemotherapy. AJR. 1977;129:1108-1110. [5] Apter S, Avider A, Gayer G, Portnoy O, Zissin R, Hertz M. Calcification in lymphoma occurring before therapy: ct features and clinical correlation. AJR. 2002;178:935-938. [6] Shinn SS, Bran comb BV, Ho KJ. Massive mediastinal hodgkin’s disease with calcification masquerading teratocarcinoma: differentiation by computed tomography. CT: The Journal of Computed Tomography. 1985;9:321-327. [7] Panicked DM, Hartly MP, Scicutella CJ, Carsky ED. Calcification in untreated mediastinal lymphoma. Radiology. 1988;166:735-736. [8] Cattleman B, Towne VM, eds. Massachusetts General Hospital: case record no. 42242. NEJM. 1956;254:1139-1141. [9] Wycoco D, Ravel B. An unusual presentation of mediastinal hodgkin’s lymphoma on computed tomography. Journal of Computed Tomography. 1983;7:187-188. [10] Apter s, Saks N, Hardan I, Amitai M, Langevitz P, Livneh A. Calcification in untreated non-hodgkin’s mediastinal lymphoma. Southern Medical Journal. 1998;91: 212-213. [11] Devita VT. Cancer: principles and practice of oncology. Philadelphia: Lippincott Williams & Wilkins; 2005. [12] Stewart AF. Hypercalcemia associated with cancer. NEJM. 2005;352:373379. [13] Korek-Amorosa J, Scheinman HZ, Clemett AR, Amoroso LF, McKenna PJ. Hypercalcemia and extensive lymph-node calcification in a patient with hodgkin’s disease prior to therapy. BJR. 1974;47:905-907. [14] Collins J, Stern EJ. Chest Radiology: The Essentials. Philadelphia: Walters Kluwer Health/Lippincott Williams & Wilkins; 2008.