MECHANICAL VENTILATION Consider the NEED for Mechanical
advertisement

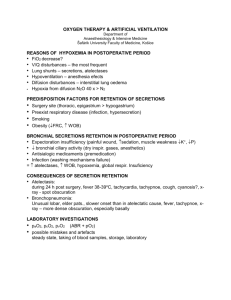
MECHANICAL VENTILATION Consider the NEED for Mechanical Ventilation if: RR > 35 Rise in PCO2 >10 TV <5cc/kg Negative inspiratory force <250mmH2O VC < 10 A-a gradient >450 PaO2 <55 Minute ventilation <10L/min PaO2/PAO2 <0.15 Unable to maintain airway or obvious respiratory distress Ventilator Modes/Settings Initial Settings: AC Rate 10-12 TV 6-10cc/kg (use IBW) FiO2 40-100% PEEP 0-5 AC—Assist Control: all breaths delivered from machine at set TV & rate but the preset rate can be exceeded by a triggering effort from the pt to deliver the same TV breath Indications: pts capable of spontaneous resp effort but with inadequate resp muscle strength to achieve adequate tidal volume; pts who can’t maintain adequate oxygenation and/or ventilation without significant work of breathing (pulm edema, ARDS, PNA) Adv: allows pts to choose RR above preset rate while obtaining adequate TV w/breath Disadvantages: pts with increased RR can develop resp alkalosis and auto-PEEP SIMV—Synchronized Intermittent Mandatory Ventilation: a preset number of breaths are mandatory and are delivered by machine at a specific TV, in between these pt may breathe spontaneously at his/her own TV Indications: should only be used with intact CNS function or helpful in weaning Advantages: pt controls PaCO2 and ventilatory pattern of spontaneous breaths, thus decreases auto-PEEP tendency and lowers mean airway pressures, keeps respiratory muscles active Disadvantages: requires active respiratory muscles and more work for pt PSV—Pressure Support Ventilation: with each pt initiated spontaneous breath, neg pressure generated opens a valve to deliver flow cycled inspiratory support only at desired pressure until inspiratory flow tapers off (pt controls RR, inspiratory time, flow rate) Indications: reduces work of breathing in weaning (not for acute resp failure), more comfortable Disadvantages: may not provide sufficient minute ventilation CPAP—Continuous Positive Airway Pressure: ventilator maintains positive pressure at the airway throughout respiratory cycle as end-expiratory pressure Indications: in spontaneous breathing pt with refractory hypoxemia who has adequate control over their PaCO2 (ventilation); weaning trials to monitor adequacy of oxygenation maintenance; sleep apnea; neuromuscular or chest wall disease PEEP—Positive End-Expiratory Pressure: maintains set amount of positive pressure at end of expiration to combat collapsing tendency of small airways and alveoli to improve compliance Indications: refractory hypoxemia, ARDS Disadvantages: more difficult to wean if PEEP required, may increase risk of barotrauma BIPAP—Bilevel Positive Airway Pressure: ventilator maintains inspiratory and expiratory pressure support to help ventilate pts (ie CPAP and PEEP) Indications: hypercarbia or hypoxemia, as a bridge before mechanical ventilation; COPD Start settings at 8-12/ 4-6; repeat ABG in 30 minutes and adjust as needed; inc PEEP to a tital volume of 5-7 L Ventilator Weaning DECREASE FiO2 after 24-48hrs to <0.60 as 100% will lead to O2 toxicity 1) Patients with acute respiratory failure should have a weaning trial daily (minimal or no CPAP) once initial insult has stabilized and FiO2 is <0.6 with sats >92%. 2) Patients with chronic respiratory failure (trach, ETT >10-14days) have chronic daily weaning trials (using PSV or CPAP) as tolerated to encourage lung mechanics (see Pre-Printed Orders) Weaning Parameters after 30-120minute weaning trial PaO2 > 60mmHg with FiO2 <0.6 PEEP <5 RR 12-30 TV >3.5ml/kg PSV <20 PaO2/FiO2 >150-200 VC >10ml/kg Minute Ventilation <10L/min Rapid shallow breathing Index = RR/TV in liters < 100 Failure to Wean, Consider Causes: 1) General: pain control, fluid status, sedation, need for bronchodilators or steroids 2) Neurologic: CVA, OSA, metabolic 3) Respiratory: fatigue, incr O2 demands, poor nutrition, electrolyte abnormalities 4) Cardiac: ischemia, CHF 5) Psych: sleep problems, depression, anxiety, fear, drug withdrawal Sedation on Mechanical Ventilation Goal: to keep pt calm, cooperative, able to follow commands, should turn off for weaning 1) Ativan: 2-4mg IV prn to sedate OR 2mg bolus followed by 1mg/hr infusion (titrate as needed for adequate sedation with max 5-10mg/hr) 2) Versed: 5-10mg IV prn to sedate OR 5mg bolus followed by 5mg/hr infusion (titrate by 1mg/hr or rebolus with 5mg for adequate sedation) 3) Propofol: initial 5-10mcg/kg/min for 10min and titrate at 5-10mcg/kg/min increments every 10-15minutes as needed for desired sedation to max 50mcg/kg/min 4) Fentanyl: 25-100mcg IV prn for sedation/analgesia OR 3mcg bolus followed by 25mcg/hr infusion (titrate 25mcg/hr or rebolus as needed for adequate sedation) Monitoring Lung Mechanics Peak Inspiratory Pressure (at end of inspiration): reflects inflation volume, airway resistance, lung and chest wall compliance Plateau Pressure (after expiration): reflects elastic recoil pressure of lungs & chest wall Incr in Peak Pressure with no change in Plateau Pressure = increased airway resistance aspiration, bronchospasm, secretions, tracheal tube resistance, obstruction Increase in both Peak Pressure and Plateau Pressure = decreased lung compliance atelectasis, auto-PEEP, pneumonia, pneumothorax, pulm edema, abd distention, asynchronous breathing