Highlights of Mechanical ventilation Unit 4
advertisement
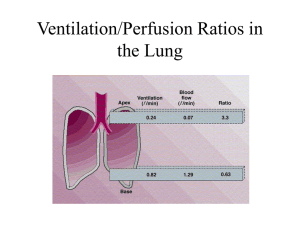
Modes and initiation of ventilation By Elizabeth Kelley Buzbee AAS, RRT-NPS HIGHLIGHTS OF MECHANICAL VENTILATION UNIT 4 The modes of ventilation: A spontaneous breath is one that the patient triggers and cycles the breath, and he controls the VT . This breath could be assisted by the application of positive pressure. A mandatory breath is defined as one that is triggered and cycled by the machine. All mandatory breaths are assisted breaths. The modes of ventilation: full support modes • CMV: continuous mandatory ventilation in which all breaths are mandatory. • VC-CMV volume control also called Assist/Control mode – Set VT, f to get VE; guaranteed VT – Default ventilatory mode for full support with adults • PC-CMV pressure control mode. Patient can trigger breaths just like with A/C – Set PIP, f and TI no guaranteed VT – Default ventilator mode for full support for infants Indications for PC: the RCP selects pressure ventilation when: The adult patient who cannot be managed with VC In this case, we keep the PIP less than 30 cmH20. PC results in better distribution of ventilation in persons with unequal RAW, but consistent compliances. There is such an airway leak so that the VT are unstable [most common with infants and small children with uncuffed ET or tracheostomy tubes] Compare PC to VC In PC, the airway pressures; mPAW and PIP will stay the same, but the VE and VT can vary based on patient’s time constants In VC the VE and VT are basically stable [patient can increase f so VE could vary] the PIP and the mPAW can be altered by patient time constants Compare control mode to Assist/control • We control patients by giving them sedation and paralytic agents so that the VE we set on VC-CMV is exactly the same • We can control their PaC02 thus their acid base balance • In A/C, the patient can trigger breaths that will increase the VE, so that the VE based on set VT and f could be lower than the actual measured VE Controlling the chronic hypercapnic patient If your patient has a hypoxic drive, administrate enough Fi02 to get his Pa02 between 80-100 mmHg. This will result in apnea and works as a form of sedation in the first 24 hours. Must wean the Fi02 to get Pa02 between 5565 mmHg before weaning Problems with A/C Excessively high PAW can cause problems with hemodynamics once patient starts to breath. Another problem with A/C mode is the risk of auto-PEEP and air trapping. Inverse Ratio Ventilation [with PC or with VC] This is a form of full support that uses increased Ti to raise the mPAW when patient’s compliance is so bad that PIP and Pplateau are excessive In IRV, the expiratory time is so short that the patient never completely exhales. This works like PEEP to recruit alveoli Raising mPAW with IRV mPAW = PIP [I] + PEEP [E] I+E Because we raise the inspiratory time so much we can decrease the PIP Because we create auto-PEEP with the short TE, we can decrease the PEEP Negative pressure ventilation The negative pressure ventilator is a box in which the patient’s body [or chest wall] is placed. A suction device is attached to the box. The NPV merely replaces the ventilatory muscles. Problems with Negative pressure Ventilation: patient must be able to: protect airway Handle being supine all the time hemodynamically stable be comfortable in one position all the time handle being disconnected from vacuum for short time spans More problems with NPV Patient can get skin lesions from movement of body inside the device Patient can get cold from ‘wind’ Best 02 device is nasal cannula because 02 can be sucked into the neck opening NPV Classified as controllers, but newer models can be A/C if there is a flow sensor placed on the patient’s nose Old metal iron lungs have a constant I:E of I:I; newer fiberglass devices can have altered I:E ratios Setting parameters on NPV: Change level of the vacuum to increase the VT [he could use a Wright’s spirometer attached to an IPPB mask to measure exhaled VT] Change the respiratory rate. CSV continuous spontaneous ventilation in which all breaths are spontaneous. patient who can completely control his VE and only needs a little help such as with increased baseline pressures [CPAP] or some application of assisted breaths such as pressure support [PS] or who might require monitoring of VE Pressure support ventilation • PSV is the most common form of pressure cycled CSV. • Although this does raise the airway pressure so that we have a higher and lower pressure, we call this PS rather than PIP because of the specific characteristics of PS • Flow triggered and flow cycled • Patient controls his VT, f and inspiratory time Indications for PS: When used with SIMV to reduce the WOB by increasing the spontaneous VT. We generally select the PS that will deliver a reasonable VT [watch the spontaneous RR] Can be used alone during weaning. Once a patient is on a PS of 5-10 cmH20, he is considered at a level that only compensates for RAW of the tubing, so is considered consistent with spontaneous breathing. PSV flow patterns The flow pattern is descending till it reaches 5 LPM [or 25% of the peak flow] in which the flow stops abruptly. The flow slows down as the device attempts to keep the PS at the preset pressure. VT on PS There is no guaranteed VT, nor VE, but we can increase the VT by increasing the PS pressure We need to set VE & high f alarms closely to warn us of problems The patient sends more air to Zone III because he is using his diaphragm more with PS To choose the correct level of PSV there are three methods: • get an appropriate VT [10-15 ml/kg] and titrate the PS level to achieve this VT • increase the PS level till the respiratory rate is normalized [25 bpm or less] • increase the PSV until you decrease the work of breathing through the ET tube • – To select the appropriate level of PSV to overcome the RAW use this formula PSV= (PIP - Pplateau) x spont insp. Flow rate [l/sec] Ventilator flow rate [l/sec] PSmax • or ‘straight pressure support’ or ‘stand alone PS’ [ PS without SIMV.] In this case, the PS is not used as a weaning modality but for initial of mechanical ventilation. • We generally select a PS level that will deliver 1012 ml kg IBW. • The RCP must remember that this mode is an assist only and the patient’s VT and VE will vary base on lung dynamics. There is no guaranteed VT. • Patient must have an intact ventilatory drive for this to work CPAP mode spontaneous mode • application of PEEP without any positive pressure breathes. • CPAP is merely a raised baseline with a flow rate with adjustable Fi02 • recruits alveoli which will improve diffusion of 02 • CPAP can help return a low compliant lung back to normal once atelectasis has been resolved. The FRC should rise. • should decrease WOB. • proper application of CPAP should decrease WOB- watch respiratory rates on this CPAP interfaces CPAP via the ET tube or a trach tube is called CPAP CPAP via a nose mask, face mask or full face mask is called nasal-CPAP [n-CPAP] Obviously we select the interface based on the patient’s ability to protect his airway n-CPAP indications The successful candidate for n-CPAP would be the patient who is oriented, has good ventilatory drive without excessive WOB and who has the ability to protect his airway. n-CPAP contraindications Persons at risk for vomiting and aspiration persons with skin necrosis, claustrophobia. CPAP indications • Management of the person who is in hypoxemia respiratory failure. This patient will have refractory hypoxemia without respiratory acidosis.. • Treatment of Congestive Heart Failure [CHF] in the patient who has an intact ventilatory drive and can keep his PaC02 down. CPAP of 8-12 with Fi02 100% is suggested. [Egans pp, 1095] • A weaning modality This invasive CPAP may be the last step before extubation. Generally a patient can be extubated from a CPAP of 5-7 cmH20 [or can be extubated at a stand-alone PSV of 5-7 cmH20. • • Non-invasive management of persons with obstructive sleep apnea [OSA APRV a spontaneous mode • airway pressure release ventilation • Patient is breathing on two different levels of CPAP • Initial settings for APRV ARDS: for • The higher CPAP is set with the Phigh, while the P low sets the • • • • • lower pressure. The RCP should also set the time interval [Thigh] for Phigh and the time interval [Tlow]for Plow To initial APRV, the RCP looks to the patient’s Pplateau on PPV and uses that figure for the Phigh. The Thigh is started at 4 seconds for adults and can be progressively increased to 10-15 seconds Set the Plow at zero and use the release time [Tlow] to keep the pressure from dropping to zero Set the Tlow at about .5 to .8 [one time constant] so that the breath ends with the expiratory flow at 50-75% of peak flow What happens if the patient goes apnic? During APRV ventilation if the patient was stop breathing, the time-cycling between high and low pressures would appear similar to PC-IRV. So this is a spontaneous mode that happens to have a back up of sorts Contraindications to APRV persons with COPD or other problems associated with air trapping. persons with excessively high intracranial pressures [high ICP] Bilevel ventilation An alternative to APRV is ‘bilevel ventilation.’ The only difference between bilevel ventilation and APRV is that the patient spends more time at the [Plow] lower airway pressure than at the high airway pressure [Phigh]. BiPap- NIPPV Non-invasive positive pressure ventilation These BiPap breathes tend to be flow or time triggered, flow cycled off with the operator selecting PIP [called IPAP] and PEEP [called EPAP] and bleeding in supplementary 02. The newer Vision can get a Fi02. http://emedicine.medscape.com/article/1417959-treatment contraindications/hazards of NIPPV – do not put this device on an apnic patient because it – – – – – – – is NOT a ventilator—it is ‘a breath augmenter’. Persons who cannot protect their airways Hemodynamically unstable patients Facial burns or trauma Uncooperative patients Persons at risk for aspiration: vomiting, nose bleeds, unconscious, poor gag reflex Copious secretions Anatomical problems with gas exchange Indications for NIPPV: acute care of: congestive heart disease [n-CPAP or BiPap] COPD patient who doesn’t want to be intubated recently extubated patient who is at risk of failing. immune-suppression for whom we may not want to risk VAP Indications for long-term NIPPV Long-term management of both obstructive sleep apnea and central sleep apnea Long-term management of patients with skeletal or neuromuscular disorders Long-term management of the COPD patient who has s/s of chronic hypoventilation [especially at night] and who is optimally treated with drugs and other care. Initial settings for BiPap: IPAP at 8 cmH20 and EPAP at 4 cmH20. . Increase IPAP in increments of 2 cmH20 to deliver more VT. To hypoxemia, increase the EPAP in increments of 2 cm H20. Oddly enough, if the EPAP is raised without raising the IPAP, the VT might decrease because the VT is a function of the change in pressure or the ‘delta P’ [ Δ P] The BiPap ST/D EPAP/CPAP: in this mode, all you get is CPAP IPAP: in this mode, again, all you get is CPAP. Spontaneous mode this is a form of PSV in which you select the PS with the IPAP and the PEEP with the EPAP. All breaths are patient triggered Spontaneous/timed: is their version of A/C PC with each breath patient or time triggered. In this mode you select the bpm Timed mode: their version of control ventilation in which you now select the rate and the inspiratory time What is so strange about the BiPAP ST/D circuit? only a single, large-bore tubing going from the compressor to the patient’s mask. constant leak at the “Whisper swivel” this will leak a minimal amount of gas out of the circuit and between the very high flow rates and the leak, the patient doesn’t rebreathe his C02. Never plug up this hole! Adding extra 02 to the BiPap STD without starting a fire add 02 at the mask, start machine first before adding 02 so gas will not leak back into machine never exceed 15 LPM Compare the BiPap STD to the Vision BiPap machine The BiPAP ST/D has no 02 inlet The Respironics Vision plugs into 50 psig 02 & can get 21% to 100% Fi02 The BiPAP ST/D has no internal alarm, you must buy a separate alarm The Respironics Vision can be used for invasive ventilation with A/C, SIMV +PSV and CPAP as well as NIPPV [CPAP and S/T] Use of critical care ventilators such as BiPap machines in the ICU. As a rule, we would operate these machines in the PSV mode with PEEP to mimic the BiPap. It is important to understand that the alarms on these machines may have to be adjusted out of range Dual modes combine mandatory ventilation with spontaneous ventilation IMV: intermittent mandatory ventilation: in which some breaths are mandatory and others are spontaneous. In this type of breath, the ventilator will give a PPV usually based on VC at timed intervals. The patient can breathe off a constant flow rate or from a demand valve at a VT and flow rate determined by his muscle strength, ventilatory drive and lung mechanics. Advantages of IMV/ SIMV patient comfort maintains muscle coordination & muscle strength reduces V/Q mismatch;Zone III is being utilized, [4] lower PAW and is an excellent weaning modality less likely to cause air-trapping Disadvantage of IMV/ SIMV: If the patient’s PPV support is removed too quickly the patient can suffer increased WOB We need to monitor the spontaneous VE , RR and VT, we may need to increase support by: increasing the SIMV rate adding PS Indications for IMV/SIMV: IMV is a partial mode of ventilation that usually includes dual modes. weaning from CMV when the patient’s ventilator muscles are weakened an initial ventilator setting when the patient is at risk for air trapping and is breathing on his own, or if the patient who is able to breathe partially for himself is at risk for decreased CO. The difference between SIMV and IMV: SIMV stands for ‘synchronized intermittent mandatory ventilation.’ The mandatory breath can come in sooner if patient triggers within the synchronization window of fractions of seconds. Special modes: PRVC In a pressure regulated volume control mode, PRVC we are attempting to deliver the VT [because we are in VC mode] but we want to keep the airway pressures low. ventilator will attempt to deliver the VT at 5 cmH20 below a preset pressure setting. Special modes: VAPS volume assured, pressure support, the ventilator will be attempting to deliver a stable VT with PS breaths so that the patient has the advantage of stable VE as well as the advantages of If a PS breath fails to reach the pre-set VT, the breath will continue at a constant flow until the volume is reached. If the patient got the pre-set VT with the PS breath, it stays PS. Unlike normal PS, these breaths aren’t just flow triggered, but can be time triggered. Special modes: MMV Mandatory minute ventilation gives the patient extra breaths or extra PS pressure to keep a predetermined minimal VE. This differs from apnea parameters in that the patient doesn’t have to actually go apneic for 20 seconds or more for this to activate. He merely needs to have hypoventilation. One problem with MMV when the patient starts the rapid, shallow breathing associated with respiratory distress. If a patient keeps the VE up with rate only, he can be in a lot of distress It is suggested to keep the maximal high respiratory rate 10 BPM above the average Special modes: ASV adaptive support ventilation: the RCP inputs the patient’s IBW and a percentage of the VE. The ventilator will deliver a VE based on the patient’s IBW. As the patient takes over more of the breathing the VE is maintained with PS breaths. The level of PS changes to give the VT calculated by the machine, The VT will be determined by the patient’s IBW and VD ventilation. Special modes: PAV In proportional assist ventilation mode similar to ASV in that the ventilator will collect data about patient’s elasticity and resistance and flow or volume demands in order to arrive at PS levels that varies. High frequency ventilation controlled ventilation- the patient is sedated and paralyzed VT of less or equal to the VD anatomical respiratory frequencies of 60 BPM-3600 bpm All HFV counts on the gas stream going down the ET tube (inside) AT THE SAME TIME and the gas flow existing (outside stream). How does HFV work Penduluft action due to various time constants of different portions of the lungs, the gas moves from one lobe to another , there is some bulk transfer What are the types of HFV high frequency jet ventilation high frequency positive pressure ventilation high frequency oscillation combination of HFJ with CMV Special modes: PRVC In pressure regulated volume control, an effort is made to maintain both a safe level of airway pressure and delivered VT. In PRVC, the RCP selects a PIP that will not be exceeded. To keep the VT, at this safe PIP, the inspiratory time and the flow rate must vary. Special modes: Auto-mode: in some ventilators selection of the auto- mode will allow the ventilator to decrease support as a patient starts to take over the WOB. The ventilator reverts between a CMV mode and a spontaneous mode based on breath by breath assessment of the patient Special modes: ATC Automatic tubing compensation, in this mode the ventilator will compensate for the RAW of the ET tube. INITIAL VENTILATOR SETTINGS VT, set f and VE Full support A/C or SIMV rate 12-16 BPM Partial support SIMV below 10 BPM 8-10 ml/Kg IBW normal lungs 6-8 ml/kg IBW asthma 5-8 ml/ kg IBW for ARDS & COPD VE needs to be 80-100 ml/KgIBW TI and Flow rates Inspiratory flow rates of 60-80 LPM for most If air hungry raise above 80 COPD- 60-100 LPM Inspiratory times .80-1.2 seconds Flow wave pattern Constant flows will decrease inspiratory time and help with I:E ratios, but can raise the PIP. Descending flow curve has the advantage of better distribution of gas into the lung, but will increase the TI and increase the mPAW Sine wave: while considered more physiological, a classic sine wave may not have enough initial flow to satisfy a patient. Like the descending flow pattern it will raise the TI and change the I:E ratio Rise time or Ramp : in an effort to fine-tune flow patterns, the constant flow can be damped by a rise time adjustments. When set high, this almost mimics an ascending flow pattern. Inspiratory pause The temporary use of the inspiratory pause at about .5 to 1 second is generally reserved for gathering Pplateau Fi02 100% is a good place to Weaning rapidly to 40-50% after ABG Fi02 needs to be weaned about 20% at a step. PEEP may be started at zero, PEEP at 5 or less cmH20 is considered physiological and should not result in CV problems-but-- remember any PEEP that causes hemodynamic problems is excessive. Increase or decrease by units of 2 Humidification by HME is limited to persons with good fluid balances, normal secretions and VE less than 10 LPM and normal body temperatures. If the patient has a gross leak so that 30% of the delivered VT is lost, the HME will not work. Humidification by heated humidifier can be used with everyone but are necessary for patients with secretions. Keep the temperatures close to 330 C +/- 2 Sighs: multiple sighs every hour or so. These sigh volumes were about 1.5 x the VT. important if VT is less than 7 ml/kg s/p lung resection or lung transplants need lower VT and faster rates to protect the torn lung from rupture. Keep the Pplateau at or below 30 cmH20 [old Egan’s 1011] lobar pneumonia: place patient on the good lung side so gas goes to the bad lung avoid PEEP in lobar pneumonia if possible Try to prolong the Ti Consider double lumen ET tube so we can set two ventilators on the patient long-term neuromuscular patients more comfortable at higher than usual VT [decrease the RR] of 10-12 ml/kg. These patients also tend to want higher flow rates. They can be managed with low Fi02-even .21 as long as Sp02 is above 90-92% low PEEP of 3-5 to prevent atelectasis are ok Persons with Congestive Heart failure We can start with normal settings, but if the PIP and Pplateau are excessive, we need to decrease the VT PEEP at 10 cmH20 and wean the Once the patient’s compliance gets better, we must wean the PEEP If the patient has an intact ventilatory drive, & good VE, he could be maintained on CPAP Initial parameters when High RAW is an issue? start with SIMV because this mode is less likely to cause air trapping. minimize air trapping and auto-PEEP COPD SIMV rate between 10-12 BPM : decrease this to 6-8 to allow time to exhale start at 60 and raise to100 LPM]. A COPD patient can be started at 40-50% Fi02 Use of PEEP with COPD is dangerous, but if the set PEEP and the auto-PEEP are kept about the same, the gas is more likely to leave the lung , keep Sp02 at 90-92% and keep the PaC02 and pH close to baseline so the patient will not suffer post-hypercapnic alkalosis Asthmatic [AHI 2005 CPR CPG pp IV 141] Alert? may do well on BiPap machine SIMV rate 6-10 BPM VT of 6-8 ml/ kg IBW 80-100 LPM with a descending flow pattern to get 1:4 or 1:5 Start Fi02 at 100%. Use of PEEP with asthmatics is dangerous, but if the set PEEP and the auto-PEEP are kept the same, the gas is more likely to leave the lung. permissive hypercapnia,