مشعر التنفس السريع والسطحي
سفن تلا زاهج نم ضيرملا ريرحت يف ضيرمتلا رود
يسفنتلا قيرطلا ةيامح ىلع رداق
بواجتمو يعاو ضيرملا
نواعتم ضيرملا
ميلس لاعس سكعنم
ميلس نايثغ سكعنم
NIF : ةيفيظو ةيسفنت تلاضع
<30
•
•
•
•
•
ماطفلل زهاج ضيرملا له
يسفنتلا روصقلا نسحت •
ةيسيئرلا ءاضعلأا دحأ روصق بايغ •
ةمئلام ةيوهت ةلاح
30 نم لقأ سفنت ةعرس
رتيل 12 نم لقأ ةقيقدلاب ةيوهت
ميلس ةيوهت زكرم
ةيفيظو ةيسفنت تلاضع
ي حطسلاو عيرسلا سفنتلا رعشم
100 نم لقأ
•
•
•
•
•
لوبقم ةجسكأ ىوتسم
P a
O
2
≥ 60 mm Hg
F i
O
2
≤ 0.40
PEEP ≤ 5 cm H
2
O
•
•
•
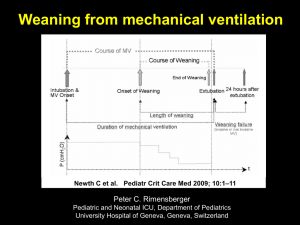
Readiness To Wean
• Improvement of respiratory failure
• Absence of major organ system failure
• Appropriate level of oxygenation
• Adequate ventilatory status
• Intact airway protective mechanism (needed for extubation)
Oxygenation Status
• Pa
O2
≥ 60 mm Hg
• Fi
O2
≤ 0.40
• PEEP ≤ 5 cm H
2
O
Ventilation Status
• Intact ventilatory drive : ability to control their own level of ventilation
• Respiratory rate < 30
• Minute ventilation of < 12 L to maintain Pa
CO2 range in normal
• RSBI < 105 ( RR / Vt < 105) , ( I use < 80)
• Functional respiratory muscles i.e.
NIF < -25 cm H2o & VC > 10 ml /kg)
Intact Airway Protective Mechanism
Appropriate level of consciousness •
Cooperation •
Intact cough reflex •
Intact gag reflex •
Functional respiratory muscles with ability to support a strong and effective cough
•
Function of Other Organ Systems
• Optimized cardiovascular function
• Arrhythmias
• Fluid overload
• Myocardial contractility
• Body temperature
• 1 ◦ degree increases CO
2 consumption by 5% production and O
2
• Normal electrolytes
• Potassium, magnesium, phosphate and calcium
• Adequate nutritional status
• Under- or over-feeding
• Optimized renal, Acid-base, liver and GI functions
ماطفلا ميقو تارعشم
Criteria Used in Several Large Trials To Define
Tolerance of an SBT *
*HR heart rate; Spo2 hemoglobin oxygen saturation. See Table 4 for abbreviations not used in the text.
يحطسلاو عيرسلا سفنتلا رعشم
سفنتلا ةعرس
يراجلا مجحلا
= يحطسلاو عيرسلا سفنتلا رعشم
Spontaneous Breathing Trials
SBT to assess extubation readiness •
T-piece or CPAP 5 cm H2O •
30-120 minutes trials •
If tolerated, patient can be extubated •
SBT as a weaning method •
Increasing length of SBT trials •
Periods of rest between trials and at night •
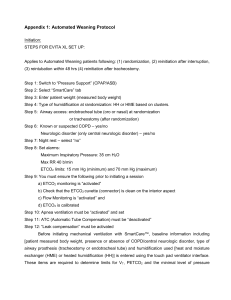
Protocols
• Developed by multidisciplinary team
• Implemented by respiratory therapists and nurses to make clinical decisions
• Results in shorter weaning times and shorter length of mechanical ventilation than physician-directed weaning
Mechanical Ventilation
PaO2/FiO2 ≥ 200 mm Hg
PEEP ≤ 5 cm H2O
Intact airway reflexes
No need for continuous infusions of vasopressors or inotrops
> 100
Rest 24 hrs
RSBI
Stable Support Strategy
Assisted/PSV
24 hours
<100
Daily SBT
Low level CPAP (5 cm H2O),
Low levels of pressure support (5 to 7 cm H2O)
“T-piece” breathing
30-120 min
Yes
RR > 35/min
Spo2 < 90%
HR > 140/min
Sustained 20% increase in HR
SBP > 180 mm Hg, DBP > 90 mm Hg
Anxiety
Diaphoresis
No
Extubation
رقتسم يسفنت معد
(PSV)
ةيلآ ةيوهت
ةعاس 24 ةحار
200 ≤ PaO2/FiO2
PEEP ≤ 5 cm H2O
نيميلس لاعسو علب سكعنم
طغضلا معاودل ةجاحلا مدع
> 100
يحطسلاو عيرسلا سفنتلا رعشم
RSBI
<100
ةعاس 24
Yes
يوفع سفنت ةلواحم
SBT
30-120 min
ةقيقدلاب ةرم 35 < سفنتلا تارم ددع
90% < نيجسكلأا عابشا
ةقيقدلاب ةبرض 140 < ضبن ةعرس
20% < ضبن ةعرس عافترا
طقض وأ قبئز ملم 180 < يضابقنا طقض
قبئز ملم 90 < يطاسبنا
قرعت
جايه
ءام مس
ءام مس
5 ىوتسمب CPAP
T
ةعطق وأ
7 5 يطغض معد وأ
ةقيقد 120 30 ةدمل
No
بوبنلأا بحس
Extubation Criteria
•
•
Ability to protect upper airway
Effective cough
Alertness
Improving clinical condition
•
Adequate lumen of trachea and larynx
“Leak test” during airway pressurization with the cuff deflated
Discontinuation of Mechanical Ventilation
To discontinue mechanical ventilation requires:
• Patient preparation
• Assessment of readiness
For independent breathing
For extubation
• A brief trial of minimally assisted breathing
An assessment of probable upper airway patency after extubation
• Either abrupt or gradual withdrawal of positive pressure, depending on the patient ’s readiness
يماغرلا بوبنلأا بحس ءارجأ
تازرفملا طفاشو تاودلأا يرضح
ضيرملل ءارجلاا يحرشأا
سولجلا ةيعضوب ضيرملا يعض
ةمامكو تازافق يعضو كيدي يلسغأ
% 100 ةجسكا ضيرملا يطعأ
بوبنلأا تبثم يعفرأ
يماغرلا بوبنلأا تازرفم يبحسأ
موعلبلاو مفلا تازرفم يبحسا
قم عو ءطبب سفنتلا ضيرملا نم يبلطاو يماغرلا بوبنلأا ىلا ةديدج ةرطثق يلخدأ
بوبنلأا نولاب يسفن
ده جلا ةمق دنعو يبلس طغض يقبطو لعسيو قيمع سفن ذخأي نأ ضيرملا نم يبلطأ
ةعرسب بوبنلأا يبحسا ضيرملل يقيهشلا
ضيرملل بطرم نيجسكأ يعض
. يسفنت داهجا ةملاع يلأ ضيرملا ةبقارم يعبات •
•
•
•
•
•
•
•
•
•
•
•
•
Failure to Wean
Respiratory:
Increased resistance
Decreased compliance
Increased WOB and exhaustion
Auto-PEEP
Cardiovascular:
Backward failure: left ventricular dysfunction
Forward heart failure
Metablic/Electrolytes:
Poor nutritional status
Overfeeding
Decreased magnesium and phosphate levels
Metabolic and respiratory alkalosis
Infection/fever
Major organ failure
Stridor
Preparation: Factors Affecting Ventilatory
Demand
Give Your Patient a
FAST HUG everyday!
• F Feeding
• A Analgesic
• S Sedation & S. Vac.
• T Thrombembolic prophylaxis
• H HOB 30 º
• U Ulcer Prophy.
• G
Glucose Control