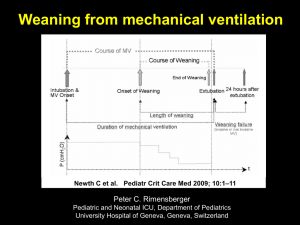
Weaning from Mechanical Ventilation
advertisement

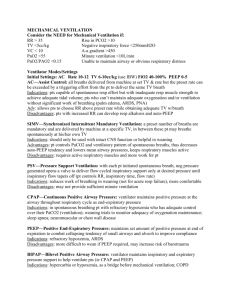
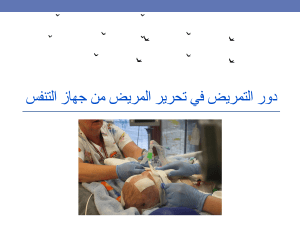
Weaning from Mechanical Ventilation Ghamartaj Khanbabaee,MD Pediatric Pulmonologist Mofid Children’s Hospital SBMU Definition of Weaning The transition process from total ventilatory support to spontaneous breathing. This period may take many forms ranging from abrupt withdrawal to gradual withdrawal from ventilatory support. Weaning and Extubation • Mechanical ventilation is a life-saving intervention • Risk of complications increases with duration • Short periods of mechanical ventilation, weaning and extubation can often be accomplished 2%and 4% of the total duration of mechanical ventilation • Longterm MV 60% to 70% of total duration Weaning Discontinuation of IPPV is achieved in most patients without difficulty Up to 20% of patients experience difficulty requires more gradual process so that they can progressively assume spontaneous respiration weaning – Is the cause of respiratory failure gone or getting better ? – Is the patient well oxygenated and ventilated ? – Can the heart tolerate the increased work of breathing ? Extubation • Extubation – Control of airway reflexes – Patent upper airway (air leak around tube?) – Minimal oxygen requirement – Minimal rate – Minimize pressure support (0-10) – “Awake ” patient Clinical criteria used to determine readiness for trials of spontaneous breathing Required criteria 1. The cause of the respiratory failure has improved 2. PaO2/FiO2≥150* or SpO2≥90 percent on FiO2≤o.4 percent and positive end-expiratory pressure (PEEP) ≤5 cmH2O 3. pH >7.25 4. Hemodynamic stability (no or low dose vasopressor medications) 5. Able to initiate an inspiratory effort Clinical criteria used to determine readiness for trials of spontaneous breathing Additional criteria (optional criteria) 1. Hemoglobin ≥8 to 10 mg/dL 2. Core temperature ≤38 to 38.5 degrees Centigrade 3. Mental status awake and alert or easily arousable * A threshold of PaO2/FiO2≥120 can be used for patients with chronic hypoxemia. Some patients require higher levels of PEEP to avoid atelectasis during mechanical ventilation. (1) The resolution of the etiology of respiratory failure and attainment of stable respiratory status (decreased FIO2 and PEEP level); absence of tachypnea with a respiratory rate <60 for infants younger than 12 months, <40 for the preschool and school-aged child, and <30 for adolescents; absence of acidosis [pH <7.35]; or hypercapnia [PCO2 >60 mm Hg]; the parameters to indirectly assess oxygenation and compliance include PaO2:FIO2 ratio >267 [PaO2 >80 mm Hg on an FIO2 of 0.3] and oxygen saturation [SpO2] >94% on an FIO2 < 0.5, PIP <20 cm H2O, and PEEP < 5 cm H2O) and adequate respiratory muscle function (2) Hemodynamic stability, including no evidence of shock this criterion includes good perfusion (capillary refill <3 seconds), age-appropriate blood pressure, and good cardiac function (3) Neurologic stability Pediatric Glasgow Coma Score > 11 (4) Metabolic factors serum potassium, magnesium, and phosphorus RCP blood gas analyses, pulse oximetry, end-tidal CO2 measurements, and airway function screenings Adjuncts to Weaning Pharmacologic Agents: corticosteroid Heliox: Helium-oxygen (HeO2) mixture has a low density and a high kinematic viscosity, allowing for a reduction in airway resistance Epinephrin Noninvasive Mechanical Ventilatory Support Weaning The best approach for all patients is to question (perhaps several times) every day: Why are they receiving mechanical ventilation? Do they require the current levels of support? Do they actually still need to be ventilated? Methods of Weaning 1- T tube trials - 30 minute T tube trial is sufficient -Attention to increased effort ( nasal flaring, accessory muscle recruitment, suprasternal and intercostal retraction, or paradoxic motion of the rib cage and abdomen). - New wheezing or crackles - Dyspnea and changes of mental status, blood pressure, heart rate, or cardiac rhythm Failing a T tube trial is a significant stress on the respiratory muscles Methods of Weaning 2-Intermittent Mandatory Ventilation(IMV) Gradual reduction in the amount of support Progressive increase in the amount of respiratory work The IMV rate is reduced, usually in steps of one to three breaths per minute An arterial blood gas is measured approximately 30 minutes after the IMV rate was reduced The IMV rate is further reduced as long as the pH remains above 7.30 or 7.35 IMV may contribute to the development of respiratory muscle fatigue or prevent recovery from it, which could delay weaning Methods of Weaning 3-Pressure Support Ventilation (PSV) PSV is an attractive weaning method Patient has control over the respiratory frequency and the depth, length, and flow of each breath PSV can compensate for the increased work imposed by the resistance of the endotracheal tube and the ventilator circuit Dyspnea is the same in PSV or IMV Resistance posed by an endotracheal tube varies as a result of diameter, flow rates, tube deformation, and adherent secretions, which makes it difficult to determine the level of PSV that overcomes the resistance of the endotracheal tube and ventilator circuit without assisting ventilation The gradual withdrawal of PSV is a poor predictor of a patient's ability to sustain ventilation after extubation (asynchrony in COPD) Methods of Weaning 4-Noninvasive ventilation Noninvasive positive pressure ventilation (NPPV) has been investigated as weaning method for patients with COPD and acute hypercapnic respiratory failure NIPPV was well tolerated Nasal abrasions and gastric distension. Exclusion : postoperative, altered neurologic status, hemodynamic instability, severe concomitant diseases • Recognition of Weaning Failure 1-Increased respiratory load: increased elastic load (unresolved lung disease, secondary pneumonia,abdominal distension, and hyperinflated lungs), increased resistive load (thickened airway secretions, partially occluded endotracheal tube, and upper airway obstruction), or increased minute ventilation (pain and irritability, sepsis /hyperthermia, and metabolic acidosis) 2- Decreased respiratory capacity: is represented by decreased respiratory drive (sedation, CNS infection, traumatic brain injury, and hypocapnia/alkalosis), muscular dysfunction (muscular catabolism and weakness ,malnutrition, and severe electrolyte disturbances), and neuromuscular disorder (diaphragmatic dysfunction, prolonged neuromuscular blockade, and cervical spinal injury) Weaning A trial of spontaneous breathing with assessment of the gas exchange and pattern of breathing with minimal pressure support(~10 cm H2O) or T-tube without pressure support appears to be equally useful approaches in order to evaluate readiness for extubation Levels of PaO2 <60 mm Hg, where FiO2 >0.4 constitutes a relative contraindication to extubation Increased respiratory rate or reduction in tidal volume(or particularly a combination of both) during spontaneous breathing strongly suggests that the patient is not ready for extubation. Difficult to wean : chronic pulmonary disease, neurologic disease, malnutrition Causes of extubation failure upper airway obstruction poor airway protection excess secretions pulmonary atelectasis young age (i.e., <3 years), duration of ventilation, severity of underline lung disease oxygenation impairment (i.e., oxygenation index >5) intravenous sedation. Extubation • Prerequisites to extubation include: 1) A good cough/gag (to allow the child to protect their airway). 2) NPO about 4 hours prior to extubation (in case the trial of extubation fails and reintubation is required). 3) Minimize sedation. 4) Adequate oxygenation on 40% FiO2 with CPAP (or PEEP) = 4. 5) The availability of someone who can reintubate the patient, if necessary. 6) Equipment available to reintubate the patient, if necessary. Extubation failure decreasing tidal volume indexed to body weight of a spontaneous breath increasing FiO2 increasing MAP increasing oxygenation index increasing fraction of total minute ventilation provided by the ventilator increasing peak ventilatory inspiratory pressure decreasing mean inspiratory flow Weaning Protocol 1. 2. 3. 4. 5. Is patient is a candidate for weaning? i) PaO2 > 60mmHg ii) FiO2 <0.5 iii) PEEP < 8 cm H2O Screen for readiness—RSB Trial i) SBT for one minute to calculate RSBI Ensure intact airway reflexes i) Coughing during suctioning Patient can now be subject to SBTs i) PS, CPAP, or T-piece ii) Up to 120 minutes SBT can be terminated if patient: i) Successfully tolerates the SBT from 30-120 minutes ii) Shows s/sx of failure RSBI First described by Yang and Tobin in 1991 Rapid Shallow Breathing Index (RSBI) is the ratio of respiratory frequency to tidal volume (f/VT) A patient who has a RR of 25 breaths/min and a VT of 250 mL/breath has an RSBI of (25 breaths/min)/(.25 L) = 100 breaths/min/L. Patients who cannot tolerate independent breathing tend to breathe rapidly (high frequency) and shallowly (low tidal volume), they generally have a high RSBI. RSBI, the respiratory frequency (f) and tidal volume (VT) were measured using a hand-held spirometer attached to the endotracheal tube while a patient breathed room air for one minute without any ventilator assistance Causes of increased RSBI : narrow endotracheal tube, female gender, sepsis, fever, supine position, anxiety, suctioning, and chronic restrictive lung disease. Failure of Weaning Indicators of deterioration are: 1. 2. 3. 4. 5. respiratory rate >35/mt. falling tidal volume <5ml/kg PaO2 <55mm Hg; Rising PaCO2 fall in blood pressure tachycardia, cardiac arrythmias, sweating increased sympathetic activity 6. altered mental status - restlessness, anxiety, confusion Dependence/Failure to Wean • Additional Features – Cardiovascular Function – Ischemia – Heart Failure – Metabolic Derangements – – – – Hypophosphatemia Hypocalcemia Hypomagnesemia Hypothyroidism (severe) – Nutrition – Poor—protein catabolism – Overfeeding—excess CO2 – Deconditioning Predictions of the outcome of weaning Variables used to predict weaning success: Gas exchange • PaO2 of > 60 mmHg with FiO2 of < 0.35 • A-a PaO2 gradient of < 350 mmHg • PaO2/FiO2 ratio of > 200 Initiate Weaning • When there is: 1. Adequate Oxygenation A) PaO2/FiO2 >150-200 B) Vent Settings: PEEP <8 and FiO2 <0.5 2. 3. 4. 5. pH >7.25 Hemodynamic stablility Ability to Initiate an Inspiratory Effort Sedation (esp. with resp-depressing drugs) has itself been weaned Conclusion Type of patient Tidal Volume RR PEEP FIO2 Ins. Flow I:E Normal 10 cc/kg 10 to 12 0 to 5 100%. 60 l/min 1:2. ARDS 6 cc/kg 10 to 12 5 to 15 100%. 60 l/min 1:2. COPD 6 cc/kg 10 to 12 5 to 10 100%. 100 to 120 1:3 to 1:4 Trauma 10 cc/kg 10 to 12 0. 100%. 60 l/min 1:2. Pediatric 8-10 cc/kg Varies age 3 to 5 100%. 60 l/min 1:2. Note Note PH>7.2 PCO2 <80 mmhg Trigger to consider Trigger to consider