Ventilator Weaning - Society of Trauma Nurses
advertisement

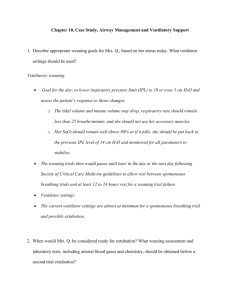
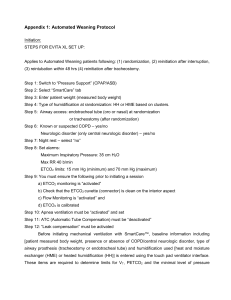
Revised 12-06-07 SICU VENTILATOR WEANING PROTOCOL Purpose: To facilitate a respiratory therapist-initiated ventilator weaning procedure in order to minimize the duration of mechanical ventilation. The following protocol is to be construed as a clinical guideline only. It is not intended to establish policy or a medical standard of care for discontinuation of mechanical ventilation nor is it intended to replace the medical judgment of the treating physician. 1. Daily Assessment of Readiness to Wean from Ventilator: Every morning, each patient should be assessed by the Respiratory Therapist (RT) and RN for the following criteria to determine whether or not they are ready for a Spontaneous Breathing Trial (SBT): a. Resolution or stabilization of the underlying disease process that contributed to the need for mechanical ventilation b. Not receiving continuous sedation or neuromuscular blocking drugs and no residual effects from prior neuromuscular blockade c. Exhibiting spontaneous respiratory efforts d. Cough/gag present or patient has tracheostomy e. Intracranial pressure </= 20 cm H2O and not requiring frequent interventions to be controlled f. No signs or symptoms of hemodynamic instability, unstable dysrhythmia, or myocardial ischemia g. FiO2 </= 0.50, PEEP </= 5 cm H2O, SaO2 >/= 90%, PaO2:FiO2 ratio >200 h. Minute ventilation </= 12-15 L/min i. Serum pH 7.3 to 7.5 j. A request to avoid weaning has not been made by a physician. If all of the criteria are not met, then the patient should continue on their current ventilator settings and be reassessed the next morning. 2. Calculation of Rapid Shallow Breathing Index (RSBI): If a patient meets the above criteria, the RT should ask the patient’s physician if it would be appropriate to proceed with a “weaning trial”. If the answer is “yes”, then a type-in order should be entered in TDS under the respiratory section that states, “Initiate ventilator weaning protocol now.” If the order is initiated by the physician, they should contact the RT on duty to let them know that a “weaning protocol” order has been entered in the computer. Once the order is entered, it will be noted on the bedside ventilator flowsheet by the RT and will remain in effect until either the patient is extubated or a physician cancels it. Once the order has been entered in the computer, a RSBI should be calculated by placing the patient on CPAP of 5 cm H2O with Pressure Support (PS) = 5 cm H2O. After one minute, the spontaneous respiratory rate and tidal volume are measured and the RSBI is calculated (RSBI = f/Vt). If the RSBI is > 105 (80 for elderly/debilitated patients), then the patient should return to their previous, non-fatiguing ventilator settings and be reassessed 6-8 hours later (not more than 2 times/day). If the RSBI is < 105 (80 for elderly/debilitated patients), then a SBT should commence. The results of the RSBI should be recorded each morning on the top of the ventilator flow sheet at the patient’s bedside. 3. Spontaneous Breathing Trial (SBT): A SBT consists of a 30-90 minute trial of spontaneous breathing with CPAP = 5 cm H2O, PS = 5 cm H2O, and FiO2 = to current settings (</= 0.5) (Note: prior to initiating a SBT, the RT and RN should review a patient’s physiologic status and planned treatments to determine if the patient is appropriate for a SBT). If the patient meets any of the following criteria, the trial should be terminated and the patient returned to their previous, non-fatiguing ventilator settings and a SBT can be repeated 6-8 hours later (not to more than 2 times/day): a. Respiratory rate > 30 for 5 minutes or more b. SaO2/SpO2 < 90% for 30 seconds or more c. Heart rate > 140 bpm or sustained increase or decrease of 20% from baseline d. New onset hypertension (SBP >180 mmHg) or hypotension (SBP <90 mmHg) e. Sustained increase in anxiety, diaphoresis, or other signs of respiratory distress f. Cardiac instability or dysrhythmia g. pH </= 7.32 h. ICP > 20 cm H2O i. RSBI > 105 (80 for elderly/debilitated patients) If the patient successfully completes the SBT, they should be considered for extubation (see #4). 4. Assessment of Readiness for Extubation: If the patient successfully completes a SBT, then the following criteria should be assessed to determine readiness for extubation: a. Does not require suctioning more than every 2 hours b. Anticipated adequate spontaneous cough and ability to protect airway c. Endotracheal tube cuff leak AUDIBLE when cuff deflated (after suctioning oropharynx) and patient either spontaneously breathing on Pressure Support 0-10 cm H2O or receiving a set tidal volume </= 10 cc/kg. If cuff leak not present, consult attending of primary service for permission to either initiate a 24-hour course of Decadron (10 mg IV q 6 hours), consult ENT service for direct laryngoscopy, or extubate patient in the presence of Anesthesia due to a potentially difficult airway. d. No known history of upper airway obstruction, edema, or stridor within previous 48 hours. e. Negative Inspiratory Force (NIF) < -20 cm H2O (if patient is following commands) f. Spontaneous tidal volume >5 cc/kg g. Vital Capacity > 10 cc/kg h. Minute Ventilation < 12 L/min i. Stomach is empty and not distended If these criteria are met, the SICU resident (pager 506-5503) should be contacted for a potential order for extubation. If the patient is not extubated, then they should return to their previous, non-fatiguing ventilator settings and be reassessed 6-8 hours later. The results of the SBT and the weaning parameters should be entered at the top of the bedside ventilator flowsheet.