Dyspepsia and Dysphagia
advertisement

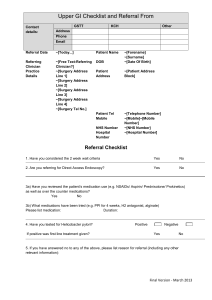
Dyspepsia and Dysphagia Dyspepsia • Common symptom • Extensive differential diagnosis • 25% of the population each year (majority don’t seek treatment) • Original definition: disordered digestion of food • Symptoms of “indigestion,” bloating, early satiety, nausea, vomiting Dyspepsia International committee definition (Rome III criteria): • Postprandial fullness • Early satiation • Epigastric pain or burning Dyspepsia—Differential Dx • Most common: functional dyspepsia (60%) • • • • NSAID induced dyspepsia Peptic ulcers GERD Neoplasm (<2%) Dyspepsia Dyspepsia Dyspepsia: Alarm Symptoms • • • • • • • • • • Unintended weight loss Persistent vomiting Progressive dysphagia Odynophagia Anemia Hematemesis Palpable mass Family hx GI cancer Previous gastric surgery Jaundice GERD • Symptoms or mucosal damage produced by abnormal reflux of gastric contents into the esophagus • Some degree of reflux physiologic • Excessive reflux of gastric juice • Impaired esophageal clearance of the refluxate • Symptoms: retrosternal burning (postprandial), regurgitation, dysphagia, chest pain, water brash, globus, odynophagia, nausea, cough GERD: Mild-Mod Sx • • • • • • • • Mild sx: lifestyle/diet modification, OTC H2 Head of bed elevation: 6-8 inches Avoid chocolate/mint/EtOH/fatty food Avoid food triggers Avoid lying supine after meals Obesity—increased risk—weight loss Promotion of salivation: gum, lozenges Smoking cessation GERD: Severe • Step up or Step down approach In ascending order of potency • OTC antacids and/or H2 blockers • Prescription H2 blockers (bid) • Intermittent (2 weeks) use of PPI • Omeprazole 20 mg daily or equivalent • Omeprazole 20 mg bid or equivalent GERD therapeutic regimens • H2 blockers (six week is adequate trial) • PPI more effective than H2 • No studies showing one PPI more effective than others • Prokinetic agents: high side effect profile • H.pylori and GERD: complex Proton Pump Inhibitors • Stomach parietal cells secrete HCl in response to histamine, acetylcholine, gastrin • H-K-ATPase (proton pump) final pathway by which acid secreted • Most potent inhibition of gastric acid available • Administer before first meal of the day (highest H-K-ATPase) • Should not be given concomitantly (at the same time of day) with H2 blocker Proton Pump Inhibitors • Inhibits only activated enzyme • Once daily dosing inhibits maximum acid output by 66% after five days • Occasional use does not reliably provide adequate acid inhibition (in contrast to H2 blocker) • Max acid secretion may not restored for 24-48 hours after discontinuing • BID dosing of PPI for first 2-3 days may be helpful in achieving more rapid acid inhibition • Rebound gastric secretion with discontinuation, consider taper if on high dose or on for > 6 mos • Chronic atrophic gastritis PPI and clopidogrel • FDA 2009 Concomitant should be avoided due to decreased clopidogrel activity • Only large scale randomized trial (2010) of omeprazole vs placebo in clopidogrel users showed no significant difference in CV events along with a significant reduction in GI events • Postulated mechanism is competitive inhibition of clopidogrel metabolism • Take home: if patient truly requires PPI then continue, but if patient has been on PPI with questionable indication consider d/c GERD: Maintenance Rx • Treat acute GERD for at least 8 weeks • Consider maintenance therapy if recurrent symptoms in < 3 months GERD: Maintenance Rx Potential risks • Increased CAP • Increased enteric infections (c.diff) • Decreased Vit B12 absorption • Increased bone fracture risk due to decreased calcium absorption and osteoclast inhibition (dose dependent and therapy dependent) • Hypomagnesemia (check if on PPI for > one year or on dig/diuretics) Peptic Ulcer Disease Pain in epigastrium (2/3) Burning, gnawing, hungerlike Vague, cramping Pattern: symptomatic periods x several weeks followed by symptoms period of weeks/months • 2-5 hours after meals or btwn 2300-0200 • • • • H.pylori testing ACG recommendations • Only if clinician plans to offer treatment • Active peptic ulcer disease or past history of documented peptic ulcer (untreated) • “Test and treat” strategy: patients under 55 with uninvestigated dyspepsia with no alarm features H.pylori stool Ag assay • Sens 94%, Spec 86-92% • Can be used to determine eradication after four weeks • False negatives: PPI, bismuth Urea breath testing • Based on hydrolysis of urea by H.pylori to produce CO2 and ammonia • Labeled carbon isotope given by mouth, presence of h.pylori liberates CO2 that can be detected • Sensitivity 88-95%, Spec 95-100% • False negatives: anti-secretory therapy, bismuth, antibiotics (off abx 4 wks, PPI 2 wks) H.pylori serology • ELISA to detect IgG antibodies • Highly sensitive 90-100%, Variable specificity 76-96% • At 18 months 60% of patients cured of infection had undetectable antibody titers Confirmation of Eradication • Recommended by ACG o o o o • • • • An patient with h.pylori associated ulcer Persistent dyspepsia despite treatment H.pylori MALT lymphoma Resection of early gastric cancer UBT or stool Ag testing Antibiotics/bismuth d/c for at least 4 wks PPI discontinued at least one week UTD authors recommend consideration of testing for confirmation of eradication in all patients treated for h.pylori H.pylori treatment • Multiple treatment regimens evaluated in RCT, no optimal therapy identified • Consider efficacy, cost, side effects, ease of administration • Most common is triple therapy with PPI, amoxicillin 1 g bid, and clarithromycin 500 bid for 7-14 days • A meta-analysis suggested that longer duration of treatment (14 vs 7 days) was associated with 5% increase in eradication rates H.pylori treatment • Prevpac: lansoprazole, amoxicillin, clarithromycin • Quadruple therapy consists of PPI, bismuth, two abx (metronidazole, tetracycline) • Pylera/Helidac: bismuth, metronidazole, tetracycline (Helidac ) • LOAD therapy: levofloxacin, omeprazole, nitazoxanide, doxycycline Dyspepsia:Functional Dysphagia: Classification Oropharyngeal dysphagia Esophageal dysphagia Dysphagia: Classification Oropharyngeal dysphagia (transfer dysphagia) • Disease of the upper esophagus and pharynx • Upper esophageal sphincter dysfunction • Patient will complain of food getting stuck immediately upon swallowing. • They will point to cervical region as location of symptoms. Dysphagia: Classification Esophageal dysphagia • Disease in body of the esophagus, lower esophageal sphincter, or cardia • Symptoms occur several seconds after swallowing • Symptoms usually located retrosternal or at the suprasternal notch Dysphagia: What to ask? • Differentiate odynophagia (pain with swallowing) from globus sensation (feeling of a lump in the throat) • Type of food that causes symptoms: solid, liquid or both? • Progressive symptoms or intermittent? • Timeline of symptoms • Other medical problems: DM, scleroderma, AIDS, NM d/o, hx radiation Dysphagia: What to ask? Mechanical • Dysphagia to solids which progress to liquids • Progressive: think cancer or stricture • Intermittent: think lower esophageal ring Motility • Dysphagia to solids AND liquids • May be progressive or intermittent Dysphagia: Testing • Barium swallow: if proximal lesion suspected by history • EGD: for mid and lower esophagus lesions • Esophageal manometry: Diagnosis of motility disorders • Videofluoroscopy: visualization and analysis of swallow. • Nasopharyngeal laryngoscopy: visualization of oropharynx, hypopharynx, larynx, vocal cords Dysphagia: Treatments • • • • • • • Reflux esophagitis: H2, PPI Lower esophageal ring: pneumatic dilation Achalasia: myotomy, pneumatic dilation, botox Peptic stricture: dilation, antireflux Rx Carcinoma: surgery, radiation Spastic motility: Ca Channel blockers, nitrates Functional dysphagia: Ca channel blockers, nitrates, SSRI, anxiolytics, smooth muscle relaxants