Dyspepsia: Definition, Causes, Pathophysiology & Treatment
advertisement

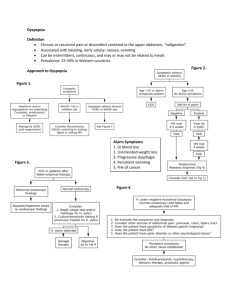
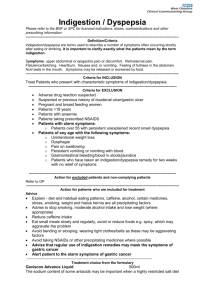
DYSPEPSIA DYSPEPSIA Dr Rakesh 1st year Gastroenterology Resident Definition Un-investigated Dyspepsia Organic Causes of Dyspepsia Functional Dyspepsia Pathophysiology of FD Approach to Un-investigated Dyspepsia Treatment DEFINITION • Dyspepsia is derived from the Greek words δυς- (dys-) and πέψη (pepse) means “difficult digestion.” • The Rome III Consensus Committee, which defined dyspepsia as the presence of symptoms that are considered to originate from the gastroduodenal region • Only 4 symptoms are now considered to be specifically of gastroduodenal origin: 1. Postprandial fullness 2. Early satiation 3. Epigastric pain 4. Epigastric burning Uninvestigated dyspepsia • The term uninvestigated dyspepsia refers to dyspeptic symptoms in persons in whom no diagnostic investigations have yet been performed and a specific diagnosis that explains the dyspeptic symptoms has not been determined ORGANIC CAUSES OF DYSPEPSIA Functional Dyspepsia Functional dyspepsia • Also known as non ulcer dyspepsia • No organic abnormality is identified by routine clinical evaluation • Commonest cause of dyspepsia in Western countries ROME IV criteria • Includes 1 or more of the following: 1. Bothersome postprandial fullness 2. Early satiation 3. Epigastric pain 4. Epigastric burning • For past 3 months with onset at least 6 months before diagnosis • No evidence of structural disease (including at upper endoscopy) that is likely to explain the symptoms • ROME III consensus proposed Functional dyspepsia be used as an umbrella term that includes: 1. Postprandial distress syndrome (PDS) characterized by meal related dyspeptic symptoms, postprandial fullness, and early satiation 2. Epigastric pain syndrome (EPS) characterized by mealunrelated dyspeptic symptoms, epigastric pain, and epigastric burning • ROME IV Committee: • When epigastric pain occurs postprandially in patients with early satiation or postprandial fullness, the patient is still categorized as having the PDS DYSPEPSIA Symptom complex • The dyspepsia symptom complex is broader than the four cardinal symptoms and it includes multiple symptoms such as – – – – – – – – Epigastric pain Early satiation Fullness, Epigastric burning Upper abdominal bloating Belching, Loss of appetite, Nausea and Vomiting. Epidemiology • • • • 10% to 45% F>M More common in smokers and NSAID users. When heartburn is excluded, the frequency of uninvestigated dyspepsia in the general population ranges from 5% to 15% • Quality of life is significantly affected by dyspepsia, especially FD. Pathophysiology Delayed Gastric emptying Impaired Gastric Accommodation Miscellaneous Functional Dyspepsia Hypersensitivity to gastric distention Altered Duodenal Sensitivity Low grade Mucosal inflammation Impaired Gastric Accommodation • Motor Function of proximal and distal stomach • Impaired accommodation • Antral distention Hypersensitivity to Gastric Distension • Visceral hypersensitivity, defined as abnormally enhanced perception of visceral stimuli, is considered one of the major pathophysiologic mechanisms • The level at which visceral hypersensitivity is generated is unclear: – Evidence for involvement of tension-sensitive mechanoreceptors – Alterations at the level of visceral afferent nerves or of the central nervous system. Low grade Mucosal Inflammation in Duodenum • Presence of increased duodenal mucosal mast cell and eosinophil counts and these findings are most clearly associated with symptoms of early satiation. • The inflammatory cell infiltrate (eosinophils and mast cells) in the duodenum has been correlated with: 1. Increased mucosal permeability 2. Altered expression of tight junction proteins 3. Impaired activity and integrity of neurons in the submucous plexus Altered Duodenal Sensitivity to Lipids or Acids • Perfusion of the duodenum with nutrient lipids, enhances the perception of gastric distention through a mechanism that requires lipid digestion and subsequent release of CCK • Duodenal infusion of hydrochloric acid induces nausea in patients with FD but not in healthy subjects, suggesting duodenal hypersensitivity to acid. Delayed Gastric Emptying • Delayed gastric emptying of solids are more likely to report postprandial fullness, nausea, and vomiting Miscellaneous 1. Rapid gastric emptying that was correlated with the intensity of postprandial Symptoms. 2. Abnormalities in the control of gastric myoelectrical activity. 3. Small bowel motor alterations, most commonly hypermotility with burst activity and an increased proportion of duodenal retrograde contractions. Pathogenic Factors 1. Genetic susceptibility 2. Infection 3. Psychological factors • Genetic Predisposition – Polymorphisms of the G-protein beta polypeptide 3 (GNB3) gene have been associated with the risk of functional dyspepsia • Hp Infection – Statistically significant beneficial effect of eradication of Hp therapy on symptoms in patients with FD – Kyoto consensus which defines Hp-associated dyspepsia as dyspepsia in an Hp-infected person with the absence of an alternative cause of dyspepsia on endoscopy and sustained control of symptoms after eradication of Hp • Post Infectious FD: – More likely to report symptoms of early satiation, weight loss, nausea, and vomiting – Significantly higher frequency of impaired accommodation of the proximal stomach, which was attributed to dysfunction at the level of gastric nitrergic neurons. – More prominent mucosal inflammation in the duodenum • Psychosocial factors – The most common psychiatric comorbidities in patients with FD are 1. Anxiety 2. Depressive or somatoform disorders 3. Recent or remote history of physical or sexual abuse. • The presence of psychosocial comorbidities is associated with greater symptom severity in patients with FD, and this association may be mediated in part by visceral hypersensitivity. APPROACH TO UNINVESTIGATED DYSPEPSIA History Symptoms Systemic illness Stress H/o Gi Infections Drugs Diet Additional Investigations • Testing for celiac disease and Giardia infection is useful for patients with refractory symptoms, especially when accompanied by weight loss. • In patients with severe pain or weight loss, US or CT can rule out pancreaticobiliary disease and screen for stenosis of large abdominal arteries. • In case of severe postprandial fullness, and refractory nausea and vomiting, a gastric emptying study using scintigraphy or a breath test can be considered. • In cases of refractory intermittent epigastric pain or burning, esophageal pH with impedance monitoring is useful for diagnosing atypical manifestations of GERD. • Psychological or psychiatric assessment is recommended for patients with long-standing refractory or debilitating symptoms. Management Strategies Endoscopy and Directed Treatment • Advantages of endoscopy: 1. Detection of organic causes of dyspepsia 2. Gastric mucosal biopsies facilitate diagnosis of Hp infection 3. Detect gastric cancer at an early curable stage Endoscopy vs Noninvasive management • Available data, do not support early endoscopy as a costeffective initial management strategy for all patients with uncomplicated dyspepsia. • Most relevant practice guidelines advocate early endoscopy: 1. In patients younger than age 45 who have a family history of gastric cancer 2. Emigrated from a country with a high rate of gastric cancer 3. Have undergone partial gastrectomy • In a young dyspeptic patient (<age 45 y) without alarm features, initial endoscopy cannot be recommended because the yield is low Test And Treat Hp Infection • Several consensus panels and guidelines have advocated noninvasive testing for Hp in young patients (<45 to 60 years of age) with uncomplicated dyspepsia • In a population with a high prevalence (>20%) of Hp infection, the test-and-treat approach remains attractive because patients with PUD will be cured. • The test-and-treat strategy as an initial approach to uninvestigated dyspepsia is most likely to be beneficial in areas where the Hp infection rate is high. Empirical Antisecretory Drug Therapy • In populations in which the prevalence of Hp infection is low, empirical antisecretory therapy (a PPI for 1 to 2 months) appears to be the preferred option • Disadvantages of empirical PPI therapy: 1. Rapid symptomatic relapse after therapy is discontinued 2. Potential for rebound gastric hypersecretion, so many patients require long-term PPI therapy Treatment of FD 1. General measures 2. Pharmacological Treatment 3. Psychological Intervention Lifestyle Modifications • Reassurance and education is of primary importance in patients with FD. • Advising patients to eat more frequent, smaller meals seems logical. • Because the presence of lipids in the duodenum enhances gastric sensitivity, avoiding meals with a high fat content may be advisable. • Discourage consumption of spicy foods containing capsaicin and other irritants. • Coffee may aggravate symptoms in some cases and should be avoided. • Cessation of smoking and consumption of alcohol. • Avoidance of aspirin and other NSAIDs is commonly recommended and seems sensible, although not of established value. Pharmacological Treatment 1. 2. 3. 4. 5. 6. Hp Eradication Acid Suppressive Drugs Prokinetic agents Agents that enhance gastric accommodation Centrally acting Neuromodulators Other Pharmacological Approaches Hp Eradication • Although H pylori–associated dyspepsia is not technically considered under the umbrella of functional dyspepsia • H pylori infection is identified in approximately 5% of dyspepsia cases. • A meta-analysis found that 9% reduction in the frequency of dyspepsia after Hp eradication, with a NNT 12.5. • A trial evaluating improvement in specific dyspepsia symptoms following H pylori therapy demonstrated improvement in epigastric pain and burning, but not early satiety or postprandial fullness. • Another study suggested that female sex is a risk factor for persistent dyspepsia symptoms despite H pylori eradication Rationale for Acid- suppressive therapy • Overlap of GERD and dyspepsia symptoms – Gastric acid secretion in patients with FD similar to that in controls1 • Acid hypersensitivity – Lowers threshold of mechanosensitive afferents – Increases nausea with duodenal acid infusion • Abnormal clearance from the duodenum – Decreases fasting clearance of exogenous acid – Decreases fasting duodenal motor activity . Acid Suppressive Drugs • Based on meta-analyses of therapeutic outcomes in FD, the efficacy of antacids, sucralfate, and misoprostol has not been demonstrated. • A meta-analysis of 12 randomized placebo-controlled trials that evaluated the efficacy of H2RAs in patients with FD reported a significant benefit over placebo, with a relative risk reduction of 23% and a number needed to treat of 7. • A meta-analysis of 15 placebo-controlled, randomized trials of PPIs for FD also confirmed that this class of agents is superior to placebo, with a number needed to treat of 10 • PPI therapy to be most effective in the group with overlapping reflux, less effective in the group with EPS, and lacking a statistically significant effect in the with PDS Prokinetic Agents • A meta-analysis has suggested that therapy with a prokinetic agent is superior to placebo in patients with FD, with a NNT of 7 • Metoclopramide and domperidone are dopamine receptor agonists with a stimulatory effect on UGI motility. • On the basis of a systematic analysis, the efficacy of prokinetic agents is not thought to be driven by their stimulatory effect on gastric emptying, but rather by effects on accommodation and visceral hypersensitivity. Enhance Gastric Accommodation • Impaired gastric accommodation is the most commonly found motor abnormality in FD. • The first-in-class agent acotiamide is both a presynaptic muscarinic autoreceptor inhibitor and a cholinesterase inhibitor and enhances both gastric emptying and accommodation. Acotiamide • Acotiamide is an oral prokinetic drug , acting as gastric motility modulator • Approved in India for “treatment of bloating after meals, epigastric bloating and early satiety in function dyspepsia” • The drug modulates upper gastrointestinal motility to alleviate abdominal symptoms resulting from hypo motility and delayed gastric emptying by increasing cholinergic activity. Mechanism of Action 1. Inhibition of acetylcholinesterase (AChE) activity in the stomach 2. Inhibition of M2,M1 Muscarinic receptors (Auto Receptors) at presynaptic terminal enhancing Ach release Centrally Acting Neuromodulators • Psychotropic agents like antidepressants, anxiolytics, and antipsychotics are commonly used for the treatment of functional GI disorders that do not respond to initial conventional approaches. • The rationale for their use is their potential to alter painprocessing pathways in the brain and, based on this concept, they are now referred to as centrally acting neuromodulators Other Therapies 1. 2. 3. 4. Bismuth Salts Peppermint Oil Rifaximin Herbal Preparation – Japan and china Psychological Interventions • Psychological interventions such as group support with relaxation training, cognitive behavioral therapy, psychotherapy, and hypnotherapy have been used in patients with FD. • Evidence to confirm the efficacy of psychological interventions in FD is insufficient.