PUD & GORD
advertisement

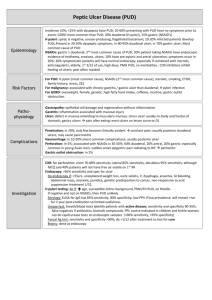
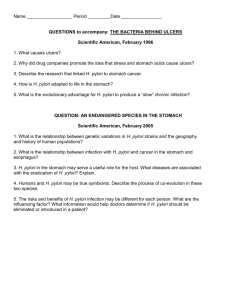
PUD & GORD Nik Sanyal Overview How common is it + what are the risk factors? What are the symptoms and signs? Investigations Management Possible exam questions Cases Epidemiology Dyspepsia occurs in 40% of the population annually and leads to a primary care consultation in 5% and endoscopy in 1%. Of those who undergo endoscopy: About 40% have functional or non-ulcer dyspepsia. 40% have gastro-oesophageal reflux disease (GORD). 13% have ulcer disease. 2% have gastric cancer. 1% have oesophageal cancer Aetiology H. pylori. NSAIDs. Smoking. Alcohol. Steroids. Stress Symptoms and Signs Nonspecific and diagnosis is unreliable on history alone Epigastric pain, usually postprandial - it may sometimes be relieved by food. Nausea. Burping , bloating, distension and intolerance of fatty food - the last is also associated with gallstones. Symptoms & Signs Heartburn sometimes (more typically associated with GORD). May cause pain radiating to the back. Signs may include tenderness or succussion splash (I wouldn’t mention it cos I wouldn’t confidently if it splashed in my face, but you might) Perforation = sudden onset pain + peritonitis, absent bowel sounds, shock Symptoms of GORD Retrosternal discomfort, acid brash regurgitation of acid or bile. Water brash - this is excessive salivation. Odynophagia (pain on swallowing) may be due to severe oesophagitis or stricture. chronic cough, and asthmatic symptoms like wheezing and shortness of breath. Graded A-D based on degree of mucosal breaks Barrett’s Oesophagus This is premalignant ectopic gastric mucosa with a change (metaplasia) from squamous to glandular. Patients with chronic GORD are at increased risk of developing the changes of Barrett's oesophagus. The risk increases with longer duration and increased frequency of gastrooesophageal symptoms. Worrying signs Age >55 + new onset dyspepsia Chronic GI bleed Dysphagia Weight loss Persistent vomiting Epigastric mass Iron deficiency anaemia Differentials Gallstones Chronic pancreatitis Cardiac e.g. MI, angina, pericarditis IBS Hepatitis Malignancy AAA Gastric vs Duodenal Ulcer DU>GU 80% DU = h.pylori, 70% of GU Duodenal ulcer — "Classic" symptoms of a duodenal ulcer include burning, gnawing, aching, or hunger-like pain. Eating improves sx but then they return 2-3hrs after. Gastric ulcer — Symptoms of a gastric ulcer typically include pain on eating. Symptoms are sometimes not relieved by eating or taking antacids. DU more likely to perforate Investigations Bedside: ECG to rule out MI Bloods: FBC to check for anaemia, raised WCC, amylase for pancreatitis, LFTs for gallstones Imaging: erect CXR – free air, AXR – constipation, cancer Special tests: stool test for H.pylori (stop PPIs 1 wk before Urea breath test – radiolabel urea + look for C13 on exhaled CO2 as H.pylori have urease. IgG can confirm h.pylori but stays +ve for weeks Management Conservative: weight loss, drink less coffee, don’t eat just before bed, reduce alcohol, stop smoking Medical: If NSAID related then >90% heal with 8 wks of H2R antagonists e.g ranitidine 150mg BD Eradication therapy: omeprazole 20mg (BD), amoxicillin 1g + clarithromycin 500mg BD or metronidazole 400mg + clarithromycin 250mg BD – antibx for 7d, PPI for 3-4 wks Surgical: Omental patches for perforation Complications Perforation can cause acute abdomen Haematemesis and malaena Duodenal scarring leading to pyloric stenosis Prognosis Prognosis is excellent if the underlying cause such as H. pylori infection or drugs can be addressed. Eradication of H. pylori decreases the ulcer recurrence rate from 60-90% to 10-20%. This is still higher than previously reported and this is thought to be due to an increase in NSAIDrelated ulcers. Those with successful eradication of GU ulcer should be scoped for GI cancer. Exam questions How does H. pylori cause ulcers? How does smoking cause ulcers? Why do NSAIDs cause ulcers? If ulcers/symptoms persist despite h.pylori eradication therapy what condition might you consider? Explain to the patient an OGD Consent for one H pylori causes depletion of somatostatin from the D cells. Somatostatin normally is released when pH is low to prevent acid release by reducing histamine + gastrin. This is because the ammonia the h.pylori releases makes the D cells think the pH is higher than it is. Smoking delays healing as well as opposing prostaglandin synthesis NSAIDs block prostaglandin production which are protective May consider zollinger-ellison: excessive production of gastrin by a tumour, stimulating hyperplasia of the gastric acid-secreting cells and producing a continual high acid output, even between meals and overnight Risks – bleeding, infection, perforation, sore throat, complications of sedation. THANKS Good luck