schizophrenia - Austin Community College
advertisement

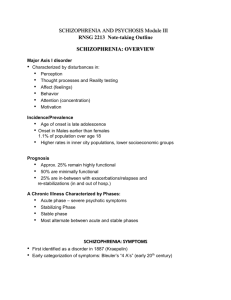
SCHIZOPHRENIA AND PSYCHOSIS Module III RNSG 2213 Note-taking Outline SCHIZOPHRENIA: OVERVIEW Major Axis I disorder • Characterized by disturbances in: • Perception • Thought processes and Reality testing • Affect (feelings) • Behavior • Attention (concentration) • Motivation Incidence/Prevalence • Age of onset is late adolescence • Onset in Males earlier than females 1.1% of population over age 18 • Higher rates in inner city populations, lower socioeconomic groups Prognosis • Approx. 25% remain highly functional • 50% are minimally functional • 25% are in-between with exacerbations/relapses and re-stabilizations (in and out of hosp.) A Chronic Illness Characterized by Phases: • Acute phase – severe psychotic symptoms • Stabilizing Phase • Stable phase • Most alternate between acute and stable phases SCHIZOPHRENIA: SYMPTOMS • • First identified as a disorder in 1887 (Kraepelin) Early categorization of symptoms: Bleuler’s “4 A’s” (early 20th century) CLASSIFICATION OF SYMPTOMS Positive Symptoms Negative (deficit) Symptoms Cognitive Symptoms POSITIVE Symptoms of Schizophrenia Agitation/aggression Altered Perceptions • Delusions • Hallucinations • Illusions Disordered thinking AEB Disordered Speech such as: loose associations, word salad, echolalia Disordered Movements, such as: restlessness, repetitive movements (echopraxia), immobility (catatonia) disorganized movement e.g. wandering NEGATIVE Symptoms of Schizophrenia • • • • • Flat affect Constricted, concrete thinking Poverty of speech (alogia), flat speech Social withdrawal; lack of pleasure in activities (anhedonia) Deep apathy COGNITIVE Symptoms of Schizophrenia Problems with: • ability to pay attention and understand • making decisions (ambivalence) • planning and carrying out activities Antipsychotic Agents and Symptoms • • The “Typical” (older class) of antipsychotics primarily address POSITIVE symptoms • Can make negative symptoms Worse The “Atypical” (newer classes) of antipsychotics address both POSITIVE AND NEGATIVE symptoms SYMPTOMS: DSM CRITERIA A. At least 2: B. C. D. E. Delusions, Hallucinations, Disorganized speech, Catatonia/ Disorganized behavior, Negative symptoms Social-occupational dysfunction Continuous s/sx. > 6 months No schizoaffective diagnosis Not caused by substance abuse or medical disorder DSM Criteria: Schizophrenia Subtypes • • • • • Paranoid – persecutory and/or grandiose delusions Disorganized – speech & affect & behavior are disturbed Catatonic – Absent, excessive &/or peculiar movements. Mutism. Undifferentiated – Does not meet criteria for other subtypes Residual – Has some disturbed thinking or behavior but does not meet other criteria OTHER PSYCHOTIC DISORDERS Schizophreniform Disorder- Has shown Schizophrenia symptoms 1-6 months Schizoaffective Disorder-Has symptoms of Schizophrenia + a Mood Disorder Psychotic Disorder NOS- Has psychotic symptoms but doesn’t fit criteria for other disorders listed. ETIOLOGY Multifactorial-no single cause Multiple theories for etiology (see next content) Current research: Is it a single disorder? BIOLOGICAL THEORIES 1) The Dopamine Hypothesis Too much dopamine binds with too many limbic receptors and causes positive 2) Disturbed ratio of serotonin:dopamine BIOLOGICAL THEORY: CHANGES IN BRAIN STRUCTURE AND FUNCTION Alterations found in some Schizophrenics using Diagnostic Imaging: • PET Scan: glucose metabolism in frontal/temporal lobes; in basal ganglia • MRI: Enlargement of ventricles • BEAM Scan: Abnormal wave patterns indicting absence of ability to “calm” the brain • Evoked Potential Topography: Illogical thought patterning in frontal lobe • • GENETIC THEORY Inherited predisposition to schizophrenia Risk Factors: Two parents with schizophrenia = 35% Identical twins = 50% DEVELOPMENTAL AND ENVIRONMENTAL THEORIES Prenatal infections Exposure to toxins Parental neglect or rejection Greater % of pts. come from lower socio-economic class Issues in Schizophrenia Noncompliance and relapse are common Have poorer ability to cope with stress Increased rates of depression, suicide Increased rate of substance abuse: alcohol, marijuana, nicotine, cocaine Often cannot hold a job INTERVENTIONS/ PSYCHOTHERAPEUTIC MANAGEMENT NURSE-CLIENT RELATIONSHIP • • • • • • Be accepting, consistent and honest Do not argue with or reinforce hallucinations or delusions Reinforce acceptable behaviors Gently encourage withdrawn client Recognize when a client may be suspicious, anxious or fearful, and approach with care Assess for command hallucinations MILIEU MANAGEMENT • • • • • • Set limits on disruptive behavior Assess agitated clients frequently for escalation Assess ability to participate in activities; choose activities at client’s level of ability May need 1:1 rather than group activities at first Decrease environmental stimuli prn Supervise meals, hygiene, grooming OTHER NURSING INTERVENTIONS Importance of patient and family education Referrals, community resources and continuity of care PHARMACOTHERAPY Antipsychotic Agents Traditional or Typical Agents: 1st Generation (beginning 1950’s) Atypical or Second Generation Agents (1990’s) Novel or Third Generation Agents (21st century) TYPICAL ANTIPSYCHOTIC AGENTS Action: Antagonize (block) Dopamine D2 receptors Most effective for Positive (+) symptoms Effects: • Sedation (esp. if combined with other CNS depressants) • • • • Slowing of motor activity Decrease in hallucinations and delusions Emotional quieting Improved cognitive function; decreased confusion High Potency e.g. haloperidol (Haldol), fluphenazine (Prolixin) Moderate Potency e.g. loxapine (Loxitane), perphenazine (Trilafon) Low Potency e.g. chlorpromazine (Thorazine), thioridazine (Mellaril) Atypical (2nd Generation) Agents Actions: Antagonize (block) multiple dopamine D and serotonin 5-HT receptors Most frequently prescribed Useful for both positive and negative symptoms clozapine (Clozaril) -Prototype risperidone (Risperdal) olanzapine (Zyprexa) quetiapine (Seroquel) ziprasidone (Geodon) paliperidone (Invega) Novel (3rd Generation) Agent aripiprazole (Abilify) Action: Partial dopamine antagonist “Balances” dopamine (both increases and decreases it in different limbic areas) Antipsychotics: Side Effects Most Common Side Effects: • Extra-Pyramidal Side Effects (EPSEs)- abnormally increased or decreased motor activity, muscle spasms, twisting, tremors Bradykinesia Akinesia Pseudo-Parkinsonism Akathisia Dystonias Tardive Dyskinesia • Anticholinergic Effects-dry mouth, orthostatic hypotension, urinary retention, blurred vision • Usually resolve over time Other Side Effects Cardiac: Arrythmias (QT interval lengthened) Blood: leukopenia, anemia, agranulocytosis-clozapine/Clozaril Endocrine and Metabolic: weight gain, elevated prolactin levels (typical agents), altered glucose metabolism diabetes Type II Sexual: Impaired libido, performance A Dangerous Side Effect Neuroleptic Malignant Syndrome (NMS) • Potentially lethal • Associated with use of high-potency agents e.g. haloperidol • Onset: within a week after starting meds. • Symptoms: muscular rigidity (“lead pipe”), tremors, autonomic hyperactivity e.g. high body temperature, altered consciousness PHARMACOTHERAPY FOR EXTRAPYRAMIDAL SEs: Antiparkinson Agents benztropine (Cogentin) * diphenhydramine (Benadryl) * trihexyphenidyl (Artane) biperiden (Akineton) amantadine (Symmetrel) • • • Action: Restore balance of dopamine with acetylcholine (ACh) Reduce motor and muscle dysfunctions caused by this imbalance BUT: They also may cause anticholinergic SEs and mental confusion (* can give these IM) EMERGENCY MEDS Goals: reduce agitation rapid sedation Common choice: IM “cocktail” of sedating antipsychotic + antiparkinsonian agent + benzodiazepine NURSING INTERVENTIONS Related to Antipsychotic Medications • Medication education (You cannot teach too often) • Explore side effect issues contributing to poor adherence/compliance • Teach Comfort and Safety measures relating to side effects: • e.g. anticholinergic effects, CNS depression, photosensitivity, thermoregulation problems, etc. • Options for clients with poor adherence: • Prolonged-acting (“depot”) form, give IM Duration: 1 wk - 4 wks • Other forms: oral disintegrating tabs, liquid concentrate, etc.