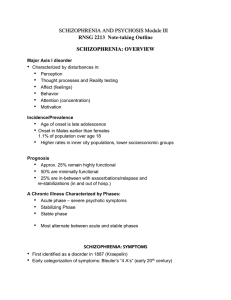
Schizophrenia Because schizophrenia is a disorder of thoughts, perceptions, and behavior, it is sometimes not recognized as an illness by the person experiencing the symptoms The natural progression of schizophrenia is usually described as a chronic illness that deteriorates over time and with an eventual plateau in the symptoms. o Only for older adults with schizophrenia has it been suggested that improvement might occur. Prodromal period (stage of early changes that are a precursor to the disorder) may begin in early childhood. o More than half of patients report the following prodromal symptoms: tension and nervousness, lack of interest in eating, difficulty concentrating, disturbed sleep, decreased enjoyment and loss of interest, restlessness, forgetfulness, depression, social withdrawal from friends, feeling laughed at, more thinking about religion, feeling bad for no reason, feeling too excited, and hearing voices or seeing things After the initial diagnosis of schizophrenia and initiation of treatment, stabilization of symptoms becomes the focus. o Symptoms become less acute but may still be present. The ultimate goal is recovery. Medication generally diminishes the symptoms and allows the person to work toward recovery. o However, no medication will cure schizophrenia. o As with any chronic illness, following a therapeutic regime, maintaining a healthy lifestyle, managing the stresses of life, and developing meaningful interpersonal relationships are important parts of the recovery. o Relapses can occur at any time during treatment and recovery. They are very detrimental to the successful management of this disorder. Relapse is not inevitable; however, it occurs with sufficient regularity to be a major concern in the treatment of schizophrenia We define positive symptoms as hallucinations and delusions and negative symptoms as diminished emotional expression and avolition (lack of interest or motivation in goaldirected behavior, such as getting dressed, going to work or to school). Positive symptoms can be thought of as excessive or distorted thoughts and perceptions that occur within the individual but are not experienced by others. o Hallucinations and delusions are positive symptoms of schizophrenia. o An easy way to remember the difference between hallucinations and delusions is that hallucinations involve one or more of the five senses. o Delusions involve only thoughts. Command hallucinations range from innocuous (eat all of your dinner) to very serious (hurt someone or jump in front of a bus) o If a patient has command hallucinations, it is important for the safety of the person and others to know what the voices are telling the patient to do Various types of delusions include the following: o Grandiose: the belief that one has exceptional powers, wealth, skill, influence, or destiny o Nihilistic: the belief that one is dead or a calamity is impending o Persecutory: the belief that one is being watched, ridiculed, harmed, or plotted against o Somatic: beliefs about abnormalities in bodily functions or structures Auditory hallucinations are more common than visual ones. Delusions are different from strongly held beliefs. Delusions do not change even though strong evidence contradicts the belief. The person continues to hold the belief despite contradictory evidence o Bizarre delusions are those beliefs that are impossible, illogical, and not derived from ordinary life experiences. o Bizarre delusions often include delusions of control (that some outside force controls thoughts and actions), o thought broadcasting (that others can read or hear one’s thoughts), o thought insertion (that someone has placed thoughts into one’s mind), o thought withdrawal (that someone is removing thoughts from one’s mind). Nonbizarre delusions generally have themes of jealousy and persecution and are derived from plausible life experiences The term “negative symptoms” is used to describe emotions and behaviors that should be present but are diminished in persons with schizophrenia. o Negative symptoms are not as dramatic as positive symptoms, but they can interfere greatly with the patient’s ability to function day to day. o Because expressing emotion is difficult for them, people with schizophrenia laugh, cry, and get angry less often. Their affect is flat; they show little or no emotion when personal loss occurs. Anhedonia prevents the person with schizophrenia from enjoying activities. People with schizophrenia may have limited speech and difficulty saying anything new or carrying on a conversation Negative symptoms reflect a lessening or loss of normal functions, such as restriction or flattening in the range and intensity of emotion (diminished emotional expression), reduced fluency and productivity of thought and speech (alogia), withdrawal and inability to initiate and persist in goal-directed activity (avolition), and inability to experience pleasure (anhedonia), affect( expression of emotion), apathy (indifference), asociality (lack of relationships) Neurocognitive impairment exists in people with schizophrenia and may be independent of positive and negative symptoms. o Neurocognition includes memory (short and long term); vigilance or sustained attention; verbal fluency or the ability to generate new words; and executive functioning, which includes volition, planning, purposeful action, and selfmonitoring behavior Disorganized symptoms of schizophrenia are findings that make it difficult for the person to understand and respond to the ordinary sights and sounds of daily living. o These include confused speech and thinking, and disorganized behavior. The following are examples of confused speech and thinking patterns: o Echolalia—repetition of another’s words that is parrot-like and inappropriate o Circumstantiality—extremely detailed and lengthy discourse about a topic o Loose associations—absence of the normal connectedness of thoughts, ideas, and topics; sudden shifts without apparent relationship to preceding topics o Tangentiality—the topic of conversation is changed to an entirely different topic that is a logical progression but causes a permanent detour from the original focus o Flight of ideas—the topic of conversation changes repeatedly and rapidly, generally after just one sentence or phrase o Word salad—stringing together words that are not connected in any way o Neologisms—words that are made up that have no common meaning and are not recognizable o Paranoia—suspiciousness and guardedness that are unrealistic and often accompanied by grandiosity o Referential thinking—a belief that neutral stimuli have special meaning to the individual, such as a television commentator who is speaking directly to the individual o Autistic thinking—restricts thinking to the literal and immediate so that the individual has private rules of logic and reasoning that make no sense to anyone else o Concrete thinking—lack of abstraction in thinking; inability to understand punch lines, metaphors, and analogies o Verbigeration—purposeless repetition of words or phrases o Metonymic speech—use of words with similar meanings interchangeably o Clang association—repetition of words or phrases that are similar in sound but in no other way, for example, “right, light, sight, might” o Stilted language—overly and inappropriately artificial formal language o Pressured speech—speaking as if the words are being forced out Disorganized behavior (which may manifest as very slow, rhythmic, or ritualistic movement) coupled with disorganized speech make it difficult for the person to partake in daily activities. o Aggression—behaviors or attitudes that reflect rage, hostility, and the potential for physical or verbal destructiveness (usually comes about if the person believes someone is going to do him or her harm) o Agitation—inability to sit still or attend to others, accompanied by heightened emotions and tension o Catatonia—psychomotor disturbances such as stupor, mutism, posturing, or repetitive behavior o Catatonic excitement—a hyperactivity characterized by purposeless activity and abnormal movements, such as grimacing and posturing o Echopraxia—involuntary imitation of another person’s movements and gestures o Regressed behavior—behaving in a manner of a less mature life stage; childlike and immature behavior o Stereotypy—repetitive purposeless movements that are idiosyncratic to the individual and to some degree outside of the individual’s control o Hypervigilance—sustained attention to external stimuli as if expecting something important or frightening to happen o Waxy flexibility—posture held in an odd or unusual fixed position for extended periods of time People with schizophrenia tend to cluster in the lowest social classes in industrialized countries and urban communities. o The symptoms of the illness are so pervasive that it is difficult for these individuals to maintain any type of gainful employment. Homelessness is a problem for people with severe mental illness Dopamine has a role in the pathogenesis of schizophrenia, but it is more complicated than previously thought. Dopamine activity is related to other disorders, cortical functioning, and stress Mood and Affect o Affective lability—abrupt, dramatic, unprovoked changes in type of emotions expressed o Ambivalence—the presence and expression of two opposing feelings, leading to inaction o Apathy—little emotional expression; diminished interest and desire Both content and speech patterns should be assessed by the nurse. o Speech content may include obvious obsessions or delusions, loose associations, or flight of ideas. o In some instances, as already noted, patients make up their own words (neologisms). o The nurse should note any difficulty in articulating words (dysarthria) or difficulty in swallowing (dysphagia) as indicators of medication-related side effects. Some persons with schizophrenia develop disturbed fluid and electrolyte balance. o Nurses should observe for polydipsia (frequently drinking an excessive amount of fluids) or frequent incontinence. o These individuals are obsessed with drinking water and compulsively consume fluids. o Nursing interventions include teaching and assisting the patient to develop selfmonitoring skills. Fluid intake and weight gain should be monitored to control fluid intake and reduce the likelihood of developing water intoxication. Antipsychotic medications are the treatment of choice for patients with psychosis. Antipsychotic drugs are used because they have the general effect of blocking dopamine transmission leading to a decrease in psychotic symptoms The prescription of first-generation antipsychotics (e.g., haloperidol, chlorpromazine) decreased dramatically with the introduction of second-generation antipsychotics. o However, it is important that medication choice be individualized based on each patient’s experience and preference as well as the side effect profiles of selected drugs rather than to limit drug selection to one type or class of antipsychotic medication Nursing interventions during the initial acute phase of schizophrenia include prompt, safe, and informed administration of antipsychotic medications. Generally, it takes about 1 to 2 weeks for antipsychotic drugs to effect a change in symptoms. During the stabilization period, the selected drug should be given an adequate trial, generally 6 to 12 weeks, before considering a change in the drug prescription. For maximum absorption, ziprasidone and lurasidone should be given with food. Ziprasidone should be taken with a high-fat meal of 500 calories. For lurasidone, 350 calories should be eaten when administering this Observe frequently for early signs of tardive dyskinesia. Use caution with individuals who have cardiovascular disease; risperidone can cause electrocardiographic changes Orthostatic hypotension is a common side effect of antipsychotic drugs. Primarily an antiadrenergic effect, decreased blood pressure may be generalized or orthostatic. Factors that have been shown to promote recovery include: o Adjustment, coping, and reappraisal o Responding to the illness o Social support, close relationships, and belonging Factors that have a negative impact on the process of recovery include: (1) negative interactions and isolation, (2) internal barriers, and (3) uncertainty and hopelessness SAD, a complex and persistent psychiatric illness, is one of the schizophrenia spectrum disorders. SAD is characterized by periods of intense symptom exacerbation alternating with periods of adequate psychosocial functioning. o When psychosis and mood disturbance occur at the same time, a diagnosis of SAD is made o Patients with SAD are more likely to exhibit persistent psychosis than are patients with a mood disorder. Delusional disorder is another schizophrenia spectrum disorder that is characterized by stable and well-systematized delusions that occur in the absence of other psychiatric disorders. The essential features of schizophreniform disorder are identical to those of schizophrenia, with the exception of the duration of the illness, which can be less than 6 months. o Symptoms must be present for at least 1 month to be classified as a schizophreniform disorder Dystonic reactions are also believed to result from the imbalance of dopamine and acetylcholine, with the latter dominant. o This side effect, which develops rapidly and dramatically, can be very frightening for patients as their muscles tense and their body contorts. o The experience often starts with oculogyric crisis, in which the muscles that control eye movements tense and pull the eyeball so that the patient is looking toward the ceiling. o This may be followed rapidly by torticollis, in which the neck muscles pull the head to the side, or retrocollis, in which the head is pulled back, or oropharyngeal dysphagia, o The immediate treatment is to administer benztropine 1 to 2 mg, or diphenhydramine (Benadryl), 25 to 50 mg, intramuscularly or intravenously. This is followed by daily administration of anticholinergic drugs and, possibly, by a decrease in dosage antipsychotic medication Akathisia appears to be caused by the same biologic mechanism as other extrapyramidal side effects. o Patients are restless and report they feel driven to keep moving. They are extremely uncomfortable. o Frequently, this response is misinterpreted as anxiety or increased psychotic symptoms, so that the patient may inappropriately be given increased dosages of an antipsychotic drug, which only perpetuates the side effect. Tardive dyskinesia, tardive dystonia, and tardive akathisia are less likely but still possible to appear in individuals taking second-generation, rather than first-generation, antipsychotics Hyperprolactinemia can occur. When dopamine is blocked in the tuberoinfundibular tract, it can no longer repress prolactin, the neurohormone that regulates lactation and mammary function o Gynecomastia, Galactorrhea (i.e., lactation) may also occur. Menstrual irregularities and sexual dysfunction are possible. Sedation is another possible side effect of antipsychotic medication and a frequent reason that patients discontinue medications. Weight gain is related to antipsychotic agents, especially olanzapine and clozapine. Patients may gain as much as 20 or 30 lb within 1 year. New-onset DM should be assessed in patients taking antipsychotic drugs. o An association has been found between new-onset DM and the administration of second-generation antipsychotic agents, especially after weight gain. o Patients should be monitored for clinical symptoms of diabetes. o Fasting blood glucose tests and hemoglobin A1C monitoring are commonly ordered for these individuals. DRESS. Symptoms include skin eruption, hematologic abnormalities (e.g., eosinophilia, atypical lymphocytosis), lymphadenopathy, and internal organ involvement (e.g., liver, kidney, lung) An anticholinergic crisis is a potentially life-threatening medical emergency caused by an overdose of or sensitivity to drugs with anticholinergic properties. o This syndrome (also called anticholinergic delirium) may result from an accidental or intentional overdose of anticholinergic drugs, including atropine, scopolamine, or belladonna alkaloids, which are present in numerous prescription drugs and OTC medicines. o characterized by fever; parched mouth; burning thirst; hot dry skin; decreased salivation; decreased bronchial and nasal secretions; widely dilated eyes (bright light becomes painful); decreased ability to accommodate visually; increased heart rate; constipation; difficulty urinating; and hypertension or hypotension. o is important for the nurse to be alert for signs and symptoms of anticholinergic crisis, especially in elderly and pediatric patients, who are much more sensitive to the anticholinergic effects of drugs, and in patients who are receiving multiple medications with anticholinergic effects. In brief psychotic disorder, the length of the episode is at least 1 day but less than 1 month. The onset is sudden and includes at least one of the positive symptoms of schizophrenia.