Schizophrenia, sept 25
advertisement

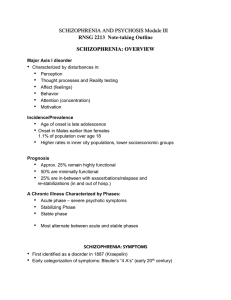
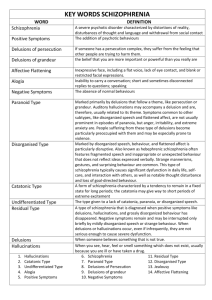
Class Notes Patricia H. Foster, EdD, RN Associate Professor of Nursing Schizophrenia Impact of Schizophrenia Nearly 4 million Americans will develop schizophrenia during their lives About 100,000 schizophrenic patients are in public mental hospitals on any given day Approximately 1 percent of the population In 3 of 4 patients, schizophrenia begins between ages 17 and 25 Estimated 1/3 to 1/2 of homeless in the US have schizophrenia Schizophrenia most chronic & disabling of the major mental illnesses 5 times more common than multiple sclerosis 6 times more common than insulin-dependent diabetes 20% to 50% of patients with schizophrenia attempt suicide; 10% succeed Diagnosis of Schizophrenia Delusions Hallucinations (gustatory is taste) each of the 5 senses can have a hallucination associated w/ it. Disorganized speech Grossly disorganized or catatonic (withdrawn) Negative symptoms (flat affect & lack of energy, apathy, lack of initiative) Bleuler’s Four A’s (a psychiatrist) Affect inappropriate Associations loose Autism focus inward neologisms (made up words) Ambivalence difficulty making decisions Problems in Cognitive Functioning Memory “Is it time for group?” Attention , easily distracted Form & content of speech Decision making concrete; difficulty with multiple stage commands ( clocks without minute or second hands Thought content-delusions & hallucinations Maladaptive movements catatonia, extrapyramidal side effects, grimacing, abnormal eye movements (staring) apraxia-difficulty carrying out a purposeful task (dressing) echopraxia- imitation of movements by others Positive Symptoms delusions & hallucinations (clues) speech-incoherence, word salad, loose associations, tangential, circumstantial, pressured speech or poverty of speech bizarre behavior-catatonia, movement disorders, deterioration of social behavior Negative Symptoms loss of normal functions flat affect alogia-restricted thought & speech apathy, lack of initiative anhedonia (lack of pleasure in anything) attention impairment-inability to focus Predisposing Factors (she thinks the book does a good job of talking about this) Biological-genetic (twin studies) identical twins have 4X the potential of having schizophrenia… there is a genetic predisposition for Neurobiology-prefrontal cortex & limbic cortex not fully developed Dysregulation of neurotransmitters (dopamine) Viral theories-prenatal exposure to influenza virus Psychological: schizophrenogenic mother (blamed it on the mother… she gave mixed messages to the kid)… not much evidence for this communication double-bind Precipitating Stressors biological information processing overload decreased gating ball game unable to differentiate noise from the crowd, team, public address system neighbor’s fireworks & startle response Paranoid Type (p. 492 in book) unfocused anxiety anger, argumentative potential for violence onset usually later in life preoccupation with paranoid delusions frequent auditory hallucinations prognosis better than for some other types Disorganized (hebephrenic… don’t call it this anymore) grimaces, incoherence, loose associations extreme social withdrawal, incoherent flat or grossly inappropriate affect early insidious onset-chronic course chronic without significant remissions Catatonic stupor negativism or mutism rigidity peculiar voluntary movement, posturing waxy flexibility (gumbie… put them in a position & they will stay that way) excessive motor activity echolalia and echopraxia Undifferentiated “wastebasket” prominent delusions hallucinations incoherence grossly disorganized behavior sometimes listed as SCUT (schizophrenia undifferentiated type) Residual when symptoms of illness persist without prominent psychotic symptoms negative symptoms emotional blunting illogical thinking mild loose associations Schizophreniform disorder meets criteria for schizophrenia episode lasts at least 1 month but less than 6 months prognosis based on onset of psychotic sx , confusion at height of psychosis, good premorbid social and occupational functioning, absence of blunted or flat affect Schizoaffective disorder major depressive episode or manic concurrent with sx of schizophrenia, (depression or mania) Delusional disorder nonbizarre delusions lasting at least a month never met criteria for schizophrenia functioning & behavior not markedly affected (woman thought the social worker was the CEO of the hospital & he was going to marry her on Valentine’s day, yet otherwise she was functioning fairly well) Brief psychotic disorder-at least one of the following: delusions, hallucinations disorganized speech disorganized or catatonic behavior Folie a deux shared delusion Antipsychotic Drugs Typical: Thorazine, Mellaril, Serentil, Trilafon, Stelazine, Navane, Loxitane, Moban Haloperidol (Haldol), Fluphenazine (Prolixin) Atypical: side effects might not be quite as bad: problematic side effect is weight gain, then they end up with metabolic syndrome & type 2 diabetes Clozapine (Clozaril) agranulocytosis Risperidone (Risperdal), Olanzapine (Zyprexa) Quetiapine (Seroquel), Ziprasidone (Geodon) Aripiprazole (Abilify) Invega is another one she has recently seen (it is in text book) Antipsychotic Drug Side Effects EPS: akathisia (can’t sit still), dystonia (involuntary muscle movement), oculogyric crisis (eyes roll back in head) Parkinson’s : cogwheel rigidity, fine tremor Tardive Dyskinesia: tongue protrusion, lip smacking Neuroleptic malignant symdrome: fever, tachycardia, muscle rigidity (potentially fatal…. Very dangerous) Agranulocytosis: fever, leucopenia (particularly for clozaril/clozapine) Seizures; photosensitivity; anticholinergic (dry mouth, reduced secretions, blurred vision, constipation… sugarless candy to help that); sedation; wt.gain, hormonal/sexual Drugs to Treat Extrapyramidal symptoms Anticholinergics: Cogentin, Artane Antihistamine: Benadryl Dopamine agonist: Symmetril, Parlodel Benzodiazepines:Valium, Ativan, Klonopin There is a table in ch 21 about the meds to treat eps Drugs to Treat Neuroleptic Malignant Syndrome parlodel Dantrolene Dopamine Tracts (not to memorize & spit back) Nigrostriatal Releases dopamine in basal ganglia (area of brain that controls muscle activity) When blocked causes EPS Tuborinfundibular Projects into anterior pituitary Prevents production of prolactin Dopamine Tracts continued Mesolimbic Releases dopamine into limbic area (important in control of emotions) Excess causes hallucinations, delusions Mesocorticol Releases dopamine into area of cortex which controls cognitive function Deficiency causes negative Sx Be sure to look at the study guides on blackboard for week 5