ABNORMAL PSYCHOLOGY SIXTH EDITION
advertisement
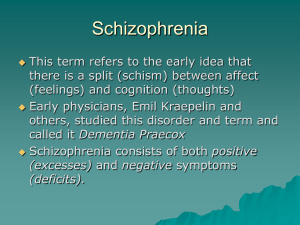
Schizophrenic Disorders Symptoms Diagnosis Causes Treatment and Management OVERVIEW Psychosis - A state of being profoundly out of touch with reality Most common symptoms: changes in the way a person thinks, feels, and relates to other people and the outside environment. Involves disruptions of mental functions No single symptom or specific set of symptoms is characteristic of patients. OVERVIEW Devastating disorder for both the patients & families. Among mental disorders, the second leading cause of disease burden. OVERVIEW Onset typically occurs during adolescence or early adulthood. The period of risk is considered to be between 15 and 35. The problems of most patients can be divided into three phases of variable and unpredictable duration: prodromal phase (developing) active phase (psychotic symptoms) residual phase (no longer psychotic but still showing signs of schizophrenia) What Schizophrenia Isn’t… Debunking myths - Not “split personality” Not inherently violent or homicidal SYMPTOMS Positive Symptoms--Type I Hallucinations ○ Perceptual disturbances ○ Can occur in any of the senses ○ Persistent over time SYMPTOMS Delusional Beliefs ○ FALSE Idiosyncratic beliefs that are rigidly held in spite of their preposterous nature. Subtypes: - Grandeur Persecution Reference Nihilistic - Capgras’ syndrome - Cotard’s syndrome SYMPTOMS Disorganization Thinking Disturbances ○ Involves disorganized speech – say things that do not make sense. Word salad Loose associations or derailment Perserveration Symptoms • Disorganized speech or thought • Neologisms • Clang associations • Echolalia SYMPTOMS Disorganization Bizarre Behavior ○ Catatonia Stuporous state – reduced responsiveness. Echopraxia Disheveled Childlike Behavior ○ Inappropriate affect SYMPTOMS Negative Symptoms--Type II Lack of initiative, social withdrawal, deficits in emotional responding. ○ Affective flattening, Blunted affect ○ Anhedonia – inability to experience pleasure. ○ Apathy - Socially withdrawn Both a symptom and coping strategy ○ Avolition – lack of will, motivation ○ Alogia – impoverished thinking, poverty of speech. Classifying Schizophrenia: The DSM-IV-TR Criteria Two or more of the following: Delusions Hallucinations Disorganized speech Grossly disorganized or catatonic behavior Negative symptoms Social/occupational dysfunction and decline Six month duration of symptoms TABLE 13-1 Diagnosis Criteria for Schizophrenia A. Characteristic Symptoms: Two (or more) of the following, each present for a significant portion of time during a 1-month period (or less if successfully treated): 1. Delusions 2. Hallucinations 3. Disorganized speech (such as frequent derailment or incoherence) 4. Grossly disorganized or catatonic behavior 5. Negative symptoms, such as affective flattening, alogia, or avolition B. Social/Occupational Dysfunction: For a significant portion of the time since the onset of the disturbance, one or more major areas of functioning such as work, interpersonal relations, or self-care is markedly below the level achieved prior to the onset. C. Duration: Continuous signs of the disturbance persist for at least six months. This six-month period must include at least one month of symptoms that meet Criterion A (active phase symptoms), and may include periods of prodromal or residual symptoms. During these prodromal or residual periods, the signs of the disturbance may be manifested by only negative symptoms or two or more symptoms listed in Criterion A present in an attenuated form (such as odd beliefs, unusual perceptual experiences). DIAGNOSIS Subtypes Schizophrenia is a heterogeneous disorder with many different clinical manifestations and levels of severity. ○ Paranoid Type ○ Disorganized Type ○ Catatonic Type ○ Undifferentiated Type ○ Residual Type DIAGNOSIS Related Psychotic Disorders Brief psychotic disorder = symptoms < 1 month Schizophreniform disorder = symptoms for 1-6 months “Schizophrenic spectrum” also includes: Schizoaffective disorder Delusional disorder Shared delusional disorder Paranoid and schizotypal personality disorders FREQUENCY Gender Differences ♂: 30 to 40% more likely to develop schizophrenia than ♀. Differences between ♂ and ♀ onset, symptoms, and course of the disorder. CAUSES TWIN STUDIES ADOPTION STUDIES The average concordance rate for MZ twins is 48%, whereas the comparable figure for DZ twins is 17%. Suggests strong genetic factors. Also compelling evidence for the importance of environment. Genain quadruplets Genetic factors play role in development of the disorder (Heston). CAUSES PREGANANCY AND BIRTH COMPLICATIONS More likely than the general population to have been exposed to various problems during their mother’s pregnancy and to have suffered birth injuries. Dietary factors VIRAL INFECTIONS Somewhat more likely to have been born during the winter/spring when viral infections are more prominent. Disorder seems to affect many different regions of the brain. Enlarged lateral ventricles Differences (decreased size) in parts of the limbic system. FIGURE 13-3 CAUSES Biological Components: Immediate Causes Brain function abnormalities: hypofrontality, neurotransmission, dopamine hypothesis Brain structure abnormalities Neuropsychological/neurophysiological abnormalities: impaired cognition, sensory gating, visual tracking CAUSES The dopamine hypothesis Interactions of multiple neurotransmitters Focuses on the function of dopamine in the limbic area of the brain. Hypothesis grew out of attempts to understand how antipsychotic drugs improve the adjustment of schizophrenic patients. Current research focuses many neurotransmitters: Serotonin GABA Glutamate CAUSES Psychological Factors Expressed Emotion ○ The family environment does have a significant impact on the course (as opposed to the etiology) of schizophrenia. ○ Patients who relapsed seemed to react negatively to some feature of their close relationship with their family. ○ See Figure 13.5 TREATMENT Antipsychotic Medication Have a relatively specific effect- reduce psychotic symptoms Positive symptoms respond better than negative symptoms. A substantial minority of patients, perhaps 25% do not improve on classical antipsychotic drugs. See Figure 13.7 relapse rate TREATMENT Antipsychotic Medication Motor Side Effects ○ Extrapyramidal symptoms ○ Tardive dyskinesia TREATMENT Antipsychotic Medication Second-Generation Antipsychotics ○ Atypical antipsychotics ○ Work on both serotonin and dopamine ○ Impact both positive and negative symptoms