ST110 Tissues and Membranes
advertisement

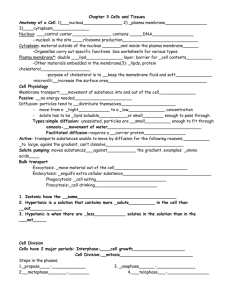
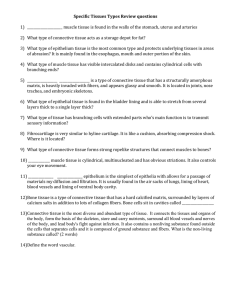
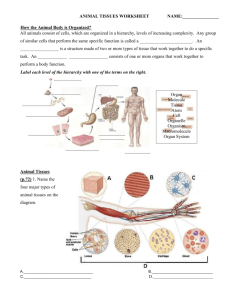
Tissue: group of similar cells that perform a common function Matrix: nonliving intercellular material Histology: The study of the structure, composition and functions of tissues Epithelial Connective Muscle Nervous Types Epithelium is divided into two types: Membranous (covering or lining) epithelium Glandular epithelium Locations Membranous epithelium: covers the body and some of its parts and lines the serous cavities; blood and lymphatic vessels; and respiratory, digestive, and genitourinary tracts Glandular epithelium: secretory units of endocrine and exocrine glands Along with connective are bound together by a basement membrane. Functions include: Protection Skin Excretion and Secretion endocrine glands Mucous glands Kidneys Sweat glands Diffusion Alveolar wall Cleaning Intestinal tract (Ciliated) Absorption Intestinal tract Kidneys Sensation Skin Tongue Generalizations about epithelial tissue Limited amount of matrix material Membranous type attached to a basement membrane Avascular Cells are in closely packed together, with many desmosomes and tight junctions Capable of reproduction Classification of epithelial tissue Membranous (covering or lining) epithelium Classification based on cell shape Squamous Cuboidal Columnar Transitional Pseudostratified columnar Epithelial and Connective tissue are bound together by basement membrane Classification based on layers of cells: Simple epithelium Simple squamous epithelium One-cell layer of flat cells Permeable to many substances Examples: Alveoli of the lungs and lining of blood vessels Simple cuboidal epithelium One-cell layer of cells that are as tall as they are wide Found in many glands and ducts (secretion & absorption) Found in the lining of the heart, blood and lymphatic vessels, body cavities, and alveoli of the lungs. • Classifications based on layers of cells (cont.) Simple columnar epithelium Single layer of tall, column-shaped cells Cells often modified for certain functions such as goblet cells (secretion), cilia (movement), microvilli (absorption) Often lines hollow visceral structures Pseudostratified columnar epithelium Columnar cells of differing heights All cells rest on basement membrane but may not reach the free surface above Cell nuclei at odd and irregular levels Found lining air passages and segments of male reproductive system Motile cilia and mucus are important modifications Hair-like extensions of cells in the respiratory tract and female reproductive system. Classifications based on layers of cells (cont.) Stratified epithelium Keratinized stratified squamous epithelium Nonkeratinized stratified squamous epithelium Multiple layers of flat, squamous cells Cells filled with keratin Covering outer skin on body surface Lining vagina, mouth, and esophagus Free surface is moist Primary function is protection Stratified cuboidal epithelium Two or more rows of cells are typical Basement membrane is indistinct Located in sweat gland ducts and pharynx Found in covering outer skin on body surface. Found in lining of vagina, mouth and esophagus. Classifications based on layers of cells (cont.) Stratified columnar epithelium Multiple layers of columnar cells Only most superficial cells are typical in shape Rare Located in segments of male urethra and near anus Transitional epithelium Located in lining of hollow viscera subjected to stress (e.g., urinary bladder) Often 10 or more layers thick Protects organ walls from tearing Has varying shapes and is capable of stretching (found in urinary bladder) Glandular epithelium Glands are usually composed of simple cuboidal cells Specialized for secretory activity Exocrine glands: discharge secretions into ducts Simple exocrine glands- only has one duct leading to the surface Compound exocrine glands- only has two or more ducts leading to the surface Endocrine glands: “ductless” glands; discharge secretions directly into blood or interstitial fluid Goblet cells- glandular epithelial cells that secrete mucous to lubricate the intestinal wall Structural classification of exocrine glands Multicellular exocrine glands are classified by the shape of their ducts and the complexity of their duct system Shapes include tubular and alveolar Simple exocrine glands: only one duct leads to the surface Compound exocrine glands: have two or more ducts Functional classification of exocrine glands (Figure 5-12) Apocrine glands Holocrine glands Secretory products collect near apex of cell and are secreted by pinching off the distended end Secretion process results in some damage to cell wall and some loss of cytoplasm Mammary glands are good examples Secretion products, when released, cause rupture and death of the cell Sebaceous glands are holocrine Merocrine glands Secrete directly through cell membrane Secretion proceeds with no damage to cell wall and no loss of cytoplasm Most numerous gland type Mast= cell that produces heparin and histamine Has large amounts of intracellular matrix Most varied and abundant tissue in the body Functions, characteristics, and types General function: Support – holds organ together Bind together tissues Mechanical framework (skeleton) General characteristics ECM predominates in most connective tissues and determines its physical characteristics Consists of fluid, gel, or solid matrix, with or without extracellular fibers (collagenous, reticular, and elastic) and proteoglycans or other compounds that thicken and hold together the tissue Types Three subgroups: Loose connective Tissue Dense Connective Tissue Specialized Connective Tissue Loose Connective Tissue Areolar Adipose Reticular • Dense Connective Tissue • Fibrous • Elastic • Specialized Connective Tissue • Bone Compact bone Cancellous bone • Cartilage Hyaline Fibrocartilage Elastic • Blood Areolar connective tissue One of the most widely distributed of all tissues Intercellular substance is prominent and consists of collagenous and elastic fibers loosely interwoven and embedded in soft viscous ground substance Several kinds of cells present, notably fibroblasts and macrophages, also mast cells, plasma cells, fat cells, and some white blood cells Function: stretchy, flexible connection Adipose tissue Similar to loose connective tissue but contains mainly fat cells Functions: protection, insulation, support, and food reserve Reticular tissue Forms framework of spleen, lymph nodes, and bone marrow Consists of network of branching reticular fibers with reticular cells overlying them Functions: defense against microorganisms and other injurious substances; reticular meshwork filters out injurious particles and reticular cells phagocytose them Dense Connective Tissue Matrix consists mainly of densely packed fibers and relatively few fibroblast cells Irregular: fibers intertwine irregularly to form a thick mat Regular: bundles of fibers are arranged in regular parallel rows Fibrous(Collagenous): mostly collagenous fibers in ECM Elastic: mostly elastic fibers in ECM Locations: structures that need great tensile strength, such as tendons and ligaments; also dermis and the outer capsule of the kidney and spleen Function: furnishes flexible connections that are strong or stretchy Membranes and Wound Healing Bone Uniquely hard and strong connective tissue type tissue Cells (osteocytes) embedded in a calcified matrix Inorganic component of matrix accounts for 65% of total bone tissue Functions Support Protection Point of attachment for muscles Reservoir for minerals Supports blood-forming tissue Provide movement Compact bone Osteon (Haversian system) Structural unity of bone Spaces for osteocytes called lacunae Matrix present in concentric rings called lamellae Canaliculi are canals that join lacunae with the central Haversian canal (communication passageway) Cell types Osteocyte: mature, inactive bone cell Osteoblast: active bone-forming cell Osteoclast: bone-destroying cell Cancellous bone made up of trabeculae Trabeculae: thin beams of bone Supports red bone marrow Myeloid tissue: a type of reticular tissue Produces blood cells Called spongy bone because of its spongelike appearance Endochondrial ossification- the conversion of cartilage to bone Periosteum- membrane that surrounds bone Cartilage Chondrocyte is the only cell type present Lacunae house cells as in bone Avascular: nutrition of cells depends on diffusion of nutrients through matrix Heals slowly after injury because of slow nutrient transfer to cells Perichondrium is membrane that surrounds cartilage Endochondrial ossification- the conversion of cartilage to bone Types Hyaline Fibrocartilage Appearance is shiny and translucent Most prevalent type of cartilage Located on ends of articulating bones Strongest and most durable type of cartilage Matrix is semirigid and filled with strong white fibers Found in intervertebral disks and pubic symphysis Serves as shock-absorbing material between bones at the knee (menisci) Elastic Contains many fine elastic fibers Provides strength and flexibility Located in external ear and larynx Blood A liquid tissue Contains neither ground substance Composition of whole blood nor fibers Liquid fraction (plasma) is the matrix; 55% of total blood volume Formed elements contribute 45% of total blood volume Red blood cells (erythrocytes) White blood cells (leukocytes) Platelets (thrombocytes) Functions Transportation Regulation of body temperature Regulation of body pH White blood cells destroy bacteria Circulating blood tissue is formed in the red bone marrow by a process called hematopoiesis; the blood-forming tissue is sometimes called hematopoietic tissue Tissues Lymphoid organs that form RBC’s or WBC’s WBC’s Red bone Marrow RBC’s Types Skeletal, or striated voluntary Smooth, also known as nonstriated involuntary or visceral Cardiac, or striated involuntary Microscopic characteristics Skeletal muscle: threadlike cells with many crossstriations and many nuclei per cell Smooth muscle: elongated narrow cells, no crossstriations, one nucleus per cell Cardiac muscle: branching cells with intercalated disks (formed by abutment of plasma membranes of two cells) Works with connective tissue to provide movement Located in walls of hollow organs, bladder, and uterus Functions: rapid regulation and integration of body activities Special characteristics Excitability Conductivity Organs Brain Spinal cord Nerves Cell types Neuron: conducting unit of system. Composed of axon, dendrites, myelin sheath, and cell body (soma) Cell body, or soma Processes Axon (single process): transmits nerve impulse away from the cell body Dendrite (one or more): transmits nerve impulse toward the cell body and axon Neuroglia: special connecting, supporting, coordinating cells that surround neurons Epineurium- the connective membrane that surrounds entire nerve Thin, “sheet like” tissue layers that cover surfaces, line cavities, and divide spaces or organs Four major types: Cutaneous Serous Mucous Synovial (connective tissue) Line body cavities that are not open to the outside of the body Secrete a thin watery fluid called Serous Fluid Lubricates the surface of the membrane and reduces friction between structures Visceral layer: covers the organs within the cavity Parietal layer: the inner linings of those cavities Visceral peritenium- covers the organs within the abdominal cavity Parietal peritoneum- inner lining of the abdominal cavity Pleura: serous membranes in the thoracic cavity Peritoneum: serous membranes in the abdominal cavity Epithelial membranes are most common type Cutaneous membrane (skin) Primary organ of integumentary system One of the most important organs Approximately 16% of body weight Epithelial Tissue Membranes Cont. Mucous membrane (mucosa) Lines and protects organs that open outside the body Found lining ducts and passageways of the respiratory, digestive, and other tracts Lamina propria: fibrous connective tissue underlying mucous epithelium Mucus is made of mostly of water and mucins— proteoglycans that form a double-layer protection against environmental microbes Connective tissue membrane: Synovial membranes line the spaces between bone in joints (classified as connective tissue membrane) Do not contain epithelial components Have smooth and slick membranes that secrete synovial fluid Help reduce friction between opposing surfaces in a movable joint Synovial membranes also line bursae Tissues Epithelial tissues and membranes maintain homeostasis Form membranes that contain and protect the internal fluid environment Absorb nutrients Secrete products that regulate functions involved in homeostasis Connective tissues Hold organs and systems together Form structures that support the body and permit movement Muscle tissues Work with connective tissues to permit movement Nervous tissues Work with glandular epithelial tissue to regulate body function Tissues have a varying capacity to repair themselves; damaged tissue regenerates or is replaced by scar tissue Regeneration: growth of new tissue Scar: dense, fibrous mass; unusually thick scar is a keloid Epithelial and connective tissues have the greatest ability to regenerate Muscle and nervous tissues have limited capacity to regenerate Two types of surgical wounds: Incisional : intentional cut through intact tissue for the purpose of exposing underlying structures Excisional : Removal of tissue Four Classes of surgical wounds: Classified by degree of microbial intrusion Class I (clean) Class II (Clean-contaminated) Class III (Contaminated) Class IV (dirty-infected) Wound classes Class I- Clean occurs when an incision is made Class II- Clean-Contaminated occurs after a primary closure- drain placed minor break in aseptic technique Class III- Contaminated occurs when an open traumatic wound is encountered, aerodigestive tract, biliary, or genitourinary tract was entered with spillage, or major break in aseptic technique. Class IV- Dirty-Infected occurs in open traumatic wounds in which microbial contamination had previously occured Infection rate Class I – 1%-5% Class II - 8%- 11% Class III - 15%- 20% Class IV - 27%- 40% First Intention– Primary Union Second Intention-- Granulation Third Intention– Delayed primary Closure Primary union Ideal Wound heals side to side w/o infection Inflammatory Response aka Lag Phase: 3-5 days Inflammation Swelling Heat Redness Loss of function Scab forms Proliferation Phase: begins around the 3rd or 4th day and lasts for 20 days Collagen fibers provide some tensile strength New capillary network is established (day 5-6) Maturation aka Differentiation Phase: Day 14 – healed Tensile strength increases Wound contraction complete (day 21) Mature scar formed *Cicatrix Granulation Occurs when a wound fails to heal by 1st intention Wound left open to heal from the bottom up Wound closure occurs by contraction Weak (herniation common) and forms a large scar Examples: When wound can not be reapproximated Infected wounds Delayed primary closure Used for dirty wounds Wound is treated by debridment of dead tissue………then left open to heal by second intention (4-6 days) once the wound is infection free, it is closed with suture or staples to finish healing by first intention Dehiscence: partial or total separation of a layer (or layers) of tissue after closure Most frequently between the 5th and 10th Postop day Causes: Abdominal distention Coughing or Vomiting Improper suture Improper suturing technique Dead Space (pg. 55): can occur when subcutaneous tissues are not approximated with suture Evisceration Hemorrhage Adhesions Herniation Fistula Keloid Scaring Sinus Tract We have genetic markers on the surface of our WBC’s Ex. HLA: Human leukocyte antigen An antigen is something that when introduced into the body triggers an immune response. Donor If an immune response occurs (ex. Proliferation of WBC’s) the tissue will likely be rejected DNA WBC’s and Recipient WBC’s are mixed Tissue Typing MHC: major histocompatibility complex Particular genes unique to each individual Permanent section: 10% formalin May remain on sterile field until the end of case Fresh or Frozen section: Sent immediately after removal Pathologist will phone OR with results Surgical Techs Responsibilities Must be able to Identity the specimen Identify the origin Must properly communicate information to circulator Properly identify and explain markers (suture) Specimens should be placed in/on: Sterile specimen cup Sterile Telfa pad Sterile towel Sterile basin *a counted sterile sponge should never be used