Cell injury, adaptation and cell death - V4US-33rd
advertisement
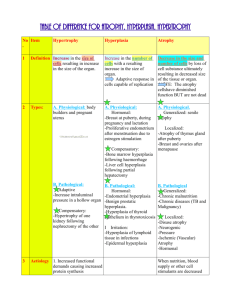
Normal cell (Homeostasis) Stress Increased demand injurious stimulus Cell injury cell death Adaptation Inability to adapt Increase in tissue or organ size due to increase in the number of component cells It takes place if the cellular population is capable of synthesizing DNA, thus permitting mitotic division Occurs in tissues with labile and stable cells Two types of hyperplasia 1. Physiological hyperplasia Hormonal – eg: proliferation of glandular epithelium of breast at puberty and pregnancy Compensatory hyperplasia – eg: following resection of part of liver, hyperplasia of connective tissue cells in wound healing 2. Pathological hyperplasia Hormonal – endometrial hyperplasia, adrenal hyperplasia, thyroid hyperplasia, bone marrow hyperplasia, lymph node hyperplasia, benign prostatic hyperplasia Growth factors – skin wart – papilloma virus and transcription factors Mechanisms of physiological hyperplasia Increased local production of growth factors Increased levels of growth factor receptors on the responding cells Activation of intracellular signaling pathways Increase in tissue or organ size due to increase in the size of the cell Cell size increased due to increased synthesis of structural proteins and organels Usually occurs in tissues with permanent cells. Hypertrophy may be physiological or pathological and caused either by 1. Increased functional demand or 2. Specific hormonal stimulation Eg. 1. Uterus in pregnancy – oestrogenic stimulation causing hyperplasia of endometrium, smooth muscle hypertrophy 2. Body builders – hypertrophy of skeletal muscle 3. Cardiomegaly – hypertension/aortic valve disease 4. Post myocardial infarct enlargement of residual viable cardiac myocytes hypertrophy Mechanisms of hypertrophy Signal transduction pathways -- induction of genes -- synthesis of numerous cellular protiens Trigger factors Mechanical triggers eg. Strech Trophic triggers eg. Polypeptide growth factor Hyperplasia is induced by known stimuli It stops when the stimulus which provoked it, is removed Decrease in tissue size due to decrease in size of a sufficient number of cells, secondary to protein degradation Cell metabolism and function are reduced to a level at which survival is possible Two types of atrophy 1. Physiologic atrophy – During early development some embryonic structures undergo atrophy, Uterus after parturition 2. Pathologic atrophy – Local or generalized 1. Decreased work load –immobilisation of a limb after fracture 2. Loss of innervation 3. Decreased blood supply 4. Loss of endocrine stimulation – in menopause 5. Lack of nutrients 6. Ageing Proteolytic pathways of protein degradation are activated Lysosomes containing proteases are activated Replacement of one type of mature (specialised) tissue by another type of mature (specialised) tissue, not normally found at that site. Can occur in epithelium and connective tissue. Occurs as an adaptive response to a stimulus Although new mature cell type is better able to withstand the adverse conditions (adaptive advantage) , protective mechanisms, like mucus secretion and ciliary clearance can be lost eg resp tract of smokers Structurally normal is potentially reversible 1. 2. Squamous metaplasia – Excretory ducts of salivary glands, pancreas, bile ducts, cervix -Ciliated epithelium of resp tract of smokers -Respiratory tract in Vitamin A deficiency Glandular metaplasia – Intestinal or gastric metaplasia of oesophagus in chronic gastric reflux Osseous Usually metaplasia of fibrous scars no adverse effects but rarely some functional defects Mechanisms of metaplasia No change in phenotype of a differentiated cell type. Result of reprogramming of stem cells which exist in normal tissue, or of undifferentiated mesenchymal cells in connective tissue