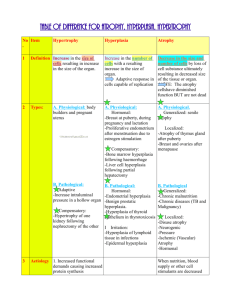
Cellular
Adaptations
Dr. Peter Anderson, UAB Pathology
Cellular Adaptations
Environmental Factors
•
•
•
•
Increased or decreased stimulation
Increased or decreased work
Decreased blood flow
Abnormal materials
Response to Stress
Response to Stress
Normal Cells
Hyperplasia
Atrophy
Metaplasia
Hypertrophy
Dysplasia
Copyright © 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved
Atrophy
• Shrinkage in the size of the cell by loss of
structural components
Atrophy
• Shrinkage in the size of the cell by loss of
structural components
– Decreased work load
– Loss of innervation
– Diminished blood supply
– Inadequate nutrition
– Loss of endocrine stimulation
Disuse Atrophy - Skeletal Muscle
Disuse Atrophy - Skeletal Muscle
Senile Atrophy
Hypertrophy
• Increased size of cells & the organ
Hypertrophy
• Increased size of cells & the organ
• Physiologic
– Hormonal stimulation e.g., uterus during
pregnancy
• Pathologic
– Increased functional demand e.g., Left
Ventricular Hypertrophy (LVH)
- hypertension or valve stenosis
Hypertrophy
Hypertrophy
Hypertrophy
Normal
Hypertrophy
Postpartum Uterus
HYPERTROPHY
Hyperplasia
• Increase in the number of cells in an
organ or tissue
Hyperplasia
• Increase in the number of cells in an
organ or tissue
– Physiologic hyperplasia
• hormonal induced – breast in pregnancy
– Pathologic hyperplasia
• viral induced – papillomaviruses
• excessive hormonal stimulation - prostate
Prostatic Hyperplasia
Prostatic Hyperplasia
Metaplasia
• Reversible change in which one differentiated
cell type is replaced by another cell type.
Ciliated Columnar
Epithelium
Squamous epithelium
Metaplasia
Ciliated Columnar
Epithelium
Stem Cells
Squamous epithelium
Metaplasia
Ciliated Columnar
Epithelium
Stem Cells
Squamous Metaplasia
Basement
Membrane
Squamous
Metaplasia
Squamous Metaplasia
- Bronchus
Kidney Stone
Transitional Epithelium
Squamous Metaplasia
Squamous Metaplasia
Metaplasia Summary
• Reversible change in which one differentiated
cell type (epithelial or mesenchymal) is
replaced by another cell type
Cellular Adaptations
Atrophy
Hypertrophy
Hyperplasia
Metaplasia
Cellular
Accumulations
Intracellular Accumulations
Normal Cellular
Constituents
Abnormal or
Exogenous
•
•
•
•
•
•
•
•
Lipids
Proteins
Glycogen
Carbohydrates
Carbon
Silica
Asbestos
Bacteria
Fatty Change
• Lipid in macrophages
– foam cells - atherosclerosis
• Lipid in parenchyma cells
– alcoholic fatty liver
Fatty Liver
• Too much lipid going in
• Not enough lipid going out
Early Fatty Change - Liver
Fatty Change - Liver
Fatty Change - Liver – Oil Red O Stain
Fatty Change Liver
Normal Liver
Fatty Change Liver
Intracellular Proteins
• Kidney Proximal Tubules
– hyaline droplets
• Plasma Cells
– Russell bodies
• Alcoholic Hyaline
Intracellular Proteins
Alcoholic Hyaline
• Liver cells of alcoholics
• Tangled skeins of cytokeratin intermediate
filaments and other proteins
• Eosinophilic cytoplasmic inclusions
• Called Mallory Alcoholic hyaline
Alcoholic Hyalin
Pigments
• Exogenous pigments
– Carbon (anthracosis)
– Tattooing
– Natural substances
• b carotiene
– Poisons
• lead (pica)
Anthracosis
Pigments
• Endogenous Pigments
– Lipofuscin
– Melanin
– Hemosiderin
Melanin - Malignant Melanoma
Iron Overload
• Hemosiderosis
– Iron overload in phagocytic cells
– No tissue damage
• Hemochromatosis
– Iron overload in parenchymal cells
– Tissue damage
Iron - Hemochromatosis
Iron - Hemochromatosis
Hemochromatosis - Liver and Pancreas
Metastatic Calcification
• Deposition of calcium in normal tissues
due to hypercalcemia
• Interstitial tissues of blood vessels,
kidneys, lungs, and gastric mucosa
Metastatic Calcification
Metastatic Calcification
Dystrophic Calcification
• Deposition of calcium salts in necrotic
tissues
• Intracellular, extracellular, or both
• Heterotopic bone may form with time
Dystrophic Calcification
Dystrophic Calcification
The End
Cellular Adaptations
&
Cellular Accumulations