Joints and Articulations
advertisement

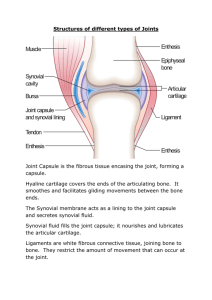
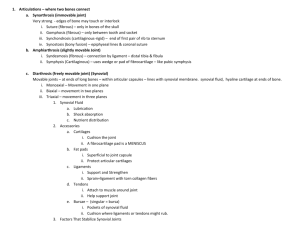
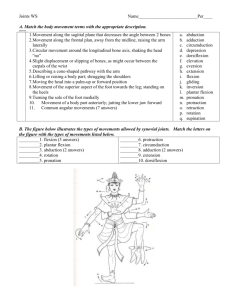
Articulations and Joints Muse lecture #6 10/19/11 Joints Chapter 9 Joint Classifications Fibrous Joints Cartilaginous Joints Synovial Joints Types of Movements at Synovial Joints Types of Synovial Joints Factors Affecting Contact and Range of Motion at Synovial Joints Selected Joints of the Body Aging and Joints Arthroplasty Muse Lecture #6 An Introduction to Articulations Articulations Body movement occurs at joints (articulations) where two bones connect Joint Structure Determines direction and distance of movement (range of motion) Joint strength decreases as mobility increases Classification of Joints Two methods of classification Functional classification is based on range of motion of the joint Structural classification relies on the anatomical organization of the joint Classification of Joints Functional Classifications Party on Arth! Synarthrosis (immovable joint) No movement Fibrous or cartilaginous connections May fuse over time Amphiarthrosis (slightly movable joint) Little movement Fibrous or cartilaginous connections Diarthrosis (freely movable joint) More movement Also called synovial joints Subdivided by type of motion Classification of Joints Classification of Joints Classification of Joints Structural Classifications Bony Fibrous Cartilaginous Synovial (capsulated) Classification of Joints Classification of Joints Functional Classifications Synarthroses (immovable joints) Are very strong Edges of bones may touch or interlock Four types of synarthrotic joints: – suture – gomphosis – synchondrosis – synostosis Classification of Joints Synarthrotic Joints Suture Bones interlocked Are bound by dense fibrous connective tissue Are found only in skull Gomphosis Fibrous connection (periodontal ligament) Binds teeth to sockets Yah can’t chomp without the gomph Joints (Fibrous Joints) Sutures Occur only between bones of the skull Syndesmoses Permits slight movement Interosseous membrane Between the tibia and fibula in the leg Gomphoses Immovable joint Joint in which a cone-shaped peg fits into a socket Articulations of the teeth with the sockets of the maxillae and mandible (b) Syndesmosis Joint held together by a ligament. Fibrous tissue can vary in length, but is longer than in sutures. Fibula Tibia Ligament Figure 8.1b Joints (Fibrous Joints) Lack a synovial cavity The articulating bones are held very closely together by dense irregular connective tissue Fibrous joints permit little or no movement Three types of fibrous joints Sutures Syndesmoses Gomphoses Classification of Joints Synarthrotic Joints Synchondrosis Is a rigid cartilaginous bridge between two bones: – epiphyseal cartilage of long bones – between vertebrosternal ribs and sternum Synostosis Fused bones, immovable: – metopic suture of skull – epiphyseal lines of long bones Classification of Joints Functional Classifications Amphiarthroses More movable than synarthrosis Stronger than freely movable joint Two types of amphiarthroses – syndesmosis: » bones connected by ligaments – symphysis: » bones separated by fibrous cartilage Classification of Joints Functional Classifications Synovial joints (diarthroses) Also called movable joints At ends of long bones Within articular capsules Lined with synovial membrane Synovial Joints Components of Synovial Joints Articular cartilages Pad articulating surfaces within articular capsules: – prevent bones from touching Smooth surfaces lubricated by synovial fluid: – reduce friction Ligament Joint cavity (contains synovial fluid) Articular (hyaline) cartilage Fibrous capsule Synovial membrane Articular capsule Periosteum Figure 8.3 Synovial Joints Components of Synovial Joints Synovial fluid Contains slippery proteoglycans secreted by fibroblasts Functions of synovial fluid: – lubrication – nutrient distribution – shock absorption Synovial Joints Components of Synovial Joints Accessory structures Cartilages: – cushion the joint: » Fibrous cartilage pad called a meniscus (articular disc) Fat pads: – superficial to the joint capsule – protect articular cartilages Ligaments: – support, strengthen joints – sprain: ligaments with torn collagen fibers Synovial Joints Components of Synovial Joints Accessory structures Tendons: – attach to muscles around joint – help support joint Bursae: – pockets of synovial fluid – cushion areas where tendons or ligaments rub Coracoacromial ligament Subacromial bursa Cavity in bursa containing synovial fluid Humerus resting Bursa rolls and lessens friction. Humerus head rolls medially as arm abducts. Humerus moving (b) Enlargement of (a), showing how a bursa eliminates friction where a ligament (or other structure) would rub against a bone Figure 8.4b Synovial Joints Factors That Stabilize Synovial Joints Prevent injury by limiting range of motion Collagen fibers (joint capsule, ligaments) Articulating surfaces and menisci Other bones, muscles, or fat pads Tendons of articulating bones Synovial Joints [INSERT FIG. 9.1a] Figure 9–1a The Structure of a Synovial Joint. Synovial Joints Figure 9–1b The Structure of a Synovial Joint. Synovial Joints Injuries Dislocation (luxation) Articulating surfaces forced out of position Damages articular cartilage, ligaments, joint capsule Subluxation A partial dislocation Movements Types of Dynamic Motion Linear motion (gliding) Angular motion Rotation Planes (Axes) of Dynamic Motion Monaxial (1 axis) Biaxial (2 axes) Triaxial (3 axes) Movements Figure 9–2 A Simple Model of Articular Motion. Movements Figure 9–2 A Simple Model of Articular Motion. Movements Types of Movements at Synovial Joints Terms describe Plane or direction of motion Relationship between structures Movements Types of Movements at Synovial Joints Linear motion Also called gliding Two surfaces slide past each other: – between carpal or tarsal bones Movements Angular Motion Flexion Angular motion Anterior–posterior plane Reduces angle between elements Extension Angular motion Anterior–posterior plane Increases angle between elements Movements Angular Motion Hyperextension Angular motion Extension past anatomical position Angular Movements Movements Figure 9–3a Angular Movements. Movements Angular Motion Abduction Think kidnapping Angular motion Frontal plane Moves away from longitudinal axis Adduction Think adding Angular motion Frontal plane Moves toward longitudinal axis Movements Figure 9–3 Angular Movements. Movements Figure 9–3 Angular Movements. Movements Angular Motion Circumduction Circular motion without rotation Angular motion Movements Figure 9–3 Angular Movements. Movements Types of Movement at Synovial Joints Rotation Direction of rotation from anatomical position Relative to longitudinal axis of body Left or right rotation Medial rotation (inward rotation): – rotates toward axis Lateral rotation (outward rotation): – rotates away from axis Movements Figure 9–4a Rotational Movements. Movements Types of Movements at Synovial Joints Rotation Pronation: – rotates forearm, radius over ulna Supination: – forearm in anatomical position Movements Figure 9–4b Rotational Movements. Movements Types of Movements at Synovial Joints Special movements Inversion: – twists sole of foot medially Eversion: – twists sole of foot laterally Dorsiflexion: – flexion at ankle (lifting toes) Plantar flexion: Plant your feet – extension at ankle (pointing toes) Movements Special Movements at Synovial Joints Opposition Thumb movement toward fingers or palm (grasping) Protraction Moves anteriorly In the horizontal plane (pushing forward) Retraction Opposite of protraction Moving anteriorly (pulling back) Movements Special Movements at Synovial Joints Elevation Moves in superior direction (up) Depression Moves in inferior direction (down) Lateral flexion Bends vertebral column from side to side Movements Figure 9–5 Special Movements. Movements Figure 9–5 Special Movements. Movements Classification of Synovial Joints by Shape Gliding Hinge Pivot Ellipsoid Saddle Ball-and-socket A Functional Classification of Synovial Joints Movements Gliding Joints Flattened or slightly curved faces Limited motion (nonaxial) Hinge Joints Angular motion in a single plane (monaxial) Pivot Joints Rotation only (monaxial) Movements Figure 9–6 Movements at Synovial Joints. Movements Ellipsoid Joints Oval articular face within a depression Motion in two planes (biaxial) Saddle Joints Two concave, straddled (biaxial) Ball-and-Socket Joints Round articular face in a depression (triaxial) Movements Figure 9–6 Movements at Synovial Joints. Movements A joint cannot be both mobile and strong The greater the mobility, the weaker the joint Mobile joints are supported by muscles and ligaments, not bone-to-bone connections Intervertebral Articulations Intervertebral Articulations C2 to L5 spinal vertebrae articulate At inferior and superior articular processes (gliding joints) Between adjacent vertebral bodies (symphyseal joints) Intervertebral Articulations Intervertebral Articulations C2 to L5 spinal vertebrae articulate Intervertebral discs: – pads of fibrous cartilage – separate vertebral bodies – anulus fibrosus: » tough outer layer » attaches disc to vertebrae – nucleus pulposus: » elastic, gelatinous core » absorbs shocks Intervertebral Articulations Figure 9–7 Intervertebral Articulations. Intervertebral Articulations Vertebral Joints Also called symphyseal joints As vertebral column moves Nucleus pulposus shifts Disc shape conforms to motion Intervertebral Ligaments Bind vertebrae together Stabilize the vertebral column Intervertebral Articulations Six Intervertebral Ligaments Anterior longitudinal ligament Connects anterior bodies Posterior longitudinal ligament Connects posterior bodies Ligamentum flavum Connects laminae Intervertebral Articulations Six Intervertebral Ligaments Interspinous ligament Connects spinous processes Supraspinous ligament Connects tips of spinous processes (C7 to sacrum) Ligamentum nuchae Continues supraspinous ligament (C7 to skull) Intervertebral Articulations Damage to Intervertebral Discs Slipped disc Bulge in anulus fibrosus Invades vertebral canal Herniated disc Nucleus pulposus breaks through anulus fibrosus Presses on spinal cord or nerves Intervertebral Articulations Figure 9–8a Damage to the Intervertebral Discs. Intervertebral Articulations Figure 9–8b Damage to the Intervertebral Discs. Intervertebral Articulations Movements of the Vertebral Column Flexion Bends anteriorly Extension Bends posteriorly Lateral flexion Bends laterally Rotation Turning Articulations of the Axial Skeleton Articulations of the Axial Skeleton Articulations of the Axial Skeleton Joints (Selected Joints of the Body) Temporomandibular Joint Combined hinge and planar joint formed by the mandible and the temporal bone Only movable joint between skull bones Only the mandible moves Superior view Outline of the mandibular fossa Lateral excursion: lateral (side-to-side) movements of the mandible Figure 8.13c Mandibular fossa Articular tubercle Zygomatic process Infratemporal fossa External acoustic meatus Lateral ligament Articular capsule Ramus of mandible (a) Location of the joint in the skull Figure 8.13a Articular disc Mandibular fossa Articular tubercle Superior joint cavity Articular capsule Synovial membranes Mandibular condyle Ramus of mandible Inferior joint cavity (b) Enlargement of a sagittal section through the joint Figure 8.13b The Shoulder Joint Also called the glenohumeral joint Allows more motion than any other joint Is the least stable Supported by skeletal muscles, tendons, ligaments Ball-and-socket diarthrosis Between head of humerus and glenoid cavity of scapula The Shoulder Joint Socket of the Shoulder Joint Glenoid labrum Deepens socket of glenoid cavity Fibrous cartilage lining Extends past the bone Processes of the Shoulder Joint Acromion (clavicle) and coracoid process (scapula) Project laterally, superior to the humerus Help stabilize the joint The Shoulder Joint Shoulder Ligaments Glenohumeral Coracohumeral Coraco-acromial Coracoclavicular Acromioclavicular Shoulder Separation Dislocation of the shoulder joint The Shoulder Joint Shoulder Muscles (also called rotator cuff) Supraspinatus Infraspinatus Subscapularis Teres minor Shoulder Bursae Subacromial Subcoracoid Subdeltoid Subscapular The Shoulder Joint Figure 9–9a The Shoulder Joint. The Shoulder Joint Figure 9–9b The Shoulder Joint. The Elbow Joint A stable hinge joint With articulations involving humerus, radius, and ulna The Elbow Joint Articulations of the Elbow Humero-ulnar joint Largest articulation Trochlea of humerus and trochlear notch of ulna Limited movement Humeroradial joint: Smaller articulation Capitulum of humerus and head of radius The Elbow Joint Figure 9–10a The Elbow Joint. The Elbow Joint Supporting Structures of the Elbow Biceps brachii muscle Attached to radial tuberosity Controls elbow motion Elbow Ligaments Radial collateral Annular Ulnar collateral The Elbow Joint Figure 9–10b The Elbow Joint. The Hip Joint Also called coxal joint Strong ball-and-socket diarthrosis Wide range of motion The Hip Joint Structures of the Hip Joint Head of femur fits into it Socket of acetabulum Which is extended by fibrocartilaginous acetabular labrum Ligaments of the Hip Joint Iliofemoral Pubofemoral Ischiofemoral Transverse acetabular Ligamentum teres The Hip Joint Figure 9–11a The Hip Joint. The Hip Joint Figure 9–11b The Hip Joint. The Hip Joint Figure 9–11c The Hip Joint. The Knee Joint A complicated hinge joint Transfers weight from femur to tibia Articulations of the knee joint Two femur–tibia articulations At medial and lateral condyles One between patella and patellar surface of femur The Knee Joint Menisci of the Knee Medial and lateral menisci Fibrous cartilage pads At femur–tibia articulations Cushion and stabilize joint Give lateral support Locking knees Standing with legs straight: – “locks” knees by jamming lateral meniscus between tibia and femur The Knee Joint Seven Ligaments of the Knee Joint Patellar ligament (anterior) Two popliteal ligaments (posterior) Anterior and posterior cruciate ligaments (inside joint capsule) Tibial collateral ligament (medial) Fibular collateral ligament (lateral) The Knee Joint Figure 9–12a The Knee Joint. The Knee Joint Figure 9–12b The Knee Joint. The Knee Joint Figure 9–12c The Knee Joint. The Knee Joint Figure 9–12d The Knee Joint. Torn meniscus Figure 8.14 The Knee Joint The Knee Joint Aging Rheumatism A pain and stiffness of skeletal and muscular systems Arthritis All forms of rheumatism that damage articular cartilages of synovial joints Osteoarthritis Caused by wear and tear of joint surfaces, or genetic factors affecting collagen formation Generally in people over age 60 Developmental Aspects of Joints By embryonic week 8, synovial joints resemble adult joints A joint’s size, shape, and flexibility are modified by use Advancing years take their toll on joints: Ligaments and tendons shorten and weaken Intervertebral discs become more likely to herniate Most people in their 70s have some degree of OA Exercise that coaxes joints through their full range of motion is key to postponing joint problems Aging Rheumatoid Arthritis An inflammatory condition Caused by infection, allergy, or autoimmune disease Involves the immune system Gouty Arthritis Occurs when crystals (uric acid or calcium salts) Form within synovial fluid Due to metabolic disorders Rheumatoid Arthritis RA begins with synovitis of the affected joint Inflammatory blood cells migrate to the joint, release inflammatory chemicals Inflamed synovial membrane thickens into a pannus Pannus erodes cartilage, scar tissue forms, articulating bone ends connect (ankylosis) Figure 8.15 Gouty Arthritis Deposition of uric acid crystals in joints and soft tissues, followed by inflammation More common in men Typically affects the joint at the base of the great toe In untreated gouty arthritis, the bone ends fuse and immobilize the joint Treatment: drugs, plenty of water, avoidance of alcohol Aging Joint Immobilization Reduces flow of synovial fluid Can cause arthritis symptoms Treated by continuous passive motion (therapy) Bones and Aging Bone mass decreases Bones weaken Increases risk of hip fracture, hip dislocation, or pelvic fracture Joints (Arthroplasty) Arthroplasty Joints may be replaced surgically with artificial joints Most commonly replaced are the hips, knees, and shoulders Hip Replacements Partial hip replacements involve only the femur Total hip replacements involve both the acetabulum and head of the femur Knee Replacements Actually a resurfacing of cartilage and may be partial or total Potential complications of arthroplasty include infection, blood clots, loosening or dislocation of the replacement components, and nerve injury Joints (Arthroplasty) Joints (Arthroplasty) Osteoarthritis (OA) Common, irreversible, degenerative (“wear-and-tear”) arthritis 85% of all Americans develop OA, more women than men Probably related to the normal aging process Osteoarthritis (OA) More cartilage is destroyed than replaced in badly aligned or overworked joints Exposed bone ends thicken, enlarge, form bone spurs, and restrict movement Treatment: moderate activity, mild pain relievers, capsaicin creams, glucosamine and chondroitin sulfate Lyme Disease Caused by bacteria transmitted by the bites of ticks Symptoms: skin rash, flu-like symptoms, and foggy thinking May lead to joint pain and arthritis Treatment: antibiotics Integration with Other Systems Bone Recycling Living bones maintain equilibrium between Bone building (osteoblasts) And breakdown (osteoclasts) Factors Affecting Bone Strength Age Physical stress Hormone levels Calcium and phosphorus uptake and excretion Genetic and environmental factors Integration with Other Systems Bones Support Body Systems The skeletal system Supports and protects other systems Stores fat, calcium, and phosphorus Manufactures cells for immune system Disorders in other body systems can cause Bone tumors Osteoporosis Arthritis Rickets (vitamin D deficiency) Integration with Other Systems Figure 9–13 Functional Relationships between the Skeletal System and Other Systems. Integration with Other Systems Figure 9–13 Functional Relationships between the Skeletal System and Other Systems.