Mechanical Ventilation
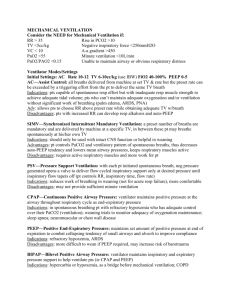
advertisement

Chapter 17 Mechanical Ventilators (plus transition to extrauterine life) Heads Paradoxical Reflex • Mediated by rapidly adapting pulmonary stretch receptors (RARs) in the lungs, with properties quite distinct from those of the slowly adapting receptors (SARs) responsible for the Breuer-Hering inflation reflex. • Called Paradoxical since it has the ability to supersede the Hering reflex which normally limits large volume inspirations. • Thought to be responsible for a babies first breath What is the primary factor that initiates breathing in a newborn infant? • The fetus lives in a relatively hypoxic environment, with a pO2 of approximately 35. • This relative hypoxia is normal for the fetus and causes the pulmonary blood vessels to constrict. • This raises pulmonary blood pressure quite high, higher than the fetus's systemic blood pressure. • So, with each heart beat, most of the cardiac output follows the path of least resistance and flows to the fetus's body. Very little flows to the fetal lungs, due to the relatively high pulmonary blood pressure. This works out just fine in utero where the fetus isn't responsible for oxygenating it's own blood, but not so well after delivery when the placenta is no longer available to provide oxygen. What is the primary factor that initiates breathing in a newborn infant? • At the moment of birth, when the baby takes it's first breath, the pO2 within the baby's bloodstream begins to rise, causing the pulmonary blood vessels to begin to relax, lowering pulmonary blood pressure. • With subsequent breaths, the pO2 continues to rise, causing pulmonary vasodilation, which drops the pulmonary blood pressure lower than the systemic blood pressure (as it should be in adult circulation), and a greater portion of cardiac output begins to flow to the baby's lungs with each heartbeat, allowing the baby to sufficiently oxygenate its own blood. What is the primary factor that initiates breathing in a newborn infant? • As the pO2 begins to rise, the fetal shunts begin to close (functionally), including the patent foramen ovale, the patent ductus arteriosus and the ductus venosus. This changes the pattern of blood flow thru the baby's heart and body to an adult pattern. If these shunts fail to close (functionally) at birth, or structurally within a few days-weeks of birth, then the baby may experience problems such as decreased oxygenation, murmur, CHF, poor feeding, poor weight gain, etc. • If the baby is deprived of oxygen at birth, due to complications such as birth asphyxia, meconium aspiration or pneumonia, these changes may not occur, and the baby may develop a lifethreatening condition called persistent pulmonary hypertension of the newborn (PPHN). What is the primary factor that initiates breathing in a newborn infant? • Perfusing its body by breathing independently instead of utilizing placental oxygen is the first challenge of a newborn. At birth, the baby's lungs are filled with fetal lung fluid (which is not amniotic fluid) and are not inflated. • The newborn is expelled from the birth canal, its central nervous system reacts to the sudden change in temperature and environment. • This triggers it to take the first breath, within about 10 seconds after delivery • With the first breaths, there is a fall in pulmonary vascular resistance, and an increase in the surface area available for gas exchange. Over the next 30 seconds the pulmonary blood flow increases and is oxygenated as it flows through the alveoli of the lungs. What is the primary factor that initiates breathing in a newborn infant? • Oxygenated blood now reaches the left atrium and ventricle, and through the descending aorta reaches the umbilical arteries. • Oxygenated blood now stimulates constriction of the umbilical arteries resulting in a reduction in placental blood flow. • As the pulmonary circulation increases there is an equivalent reduction in the placental blood flow which normally ceases completely after about three minutes. • These two changes result in a rapid redirection of blood flow into the pulmonary vascular bed, from approximately 4% to 100% of cardiac output What is the primary factor that initiates breathing in a newborn infant? • The increase in pulmonary venous return results in left atrial pressure being slightly higher than right atrial pressure, which closes the foramen ovale. • The flow pattern changes results in a drop in blood flow across the ductus arteriosus and the higher blood oxygen content of blood within the aorta stimulates the constriction and ultimately the closure of this fetal circulatory shunt. • All of these cardiovascular system changes result in the adaptation from fetal circulation patterns to an adult circulation pattern. During this transition, some types of congenital heart disease that were not symptomatic in utero during fetal circulation will present with cyanosis or respiratory signs. What is the primary factor that initiates breathing in a newborn infant? • Following birth, the expression and re-uptake of surfactant, which begins to be produced by the fetus at 20 weeks gestation, is accelerated. • Expression of surfactant into the alveoli is necessary to prevent alveolar closure (atelectasis). At this point, rhythmic breathing movements also commence. If there are any problems with breathing, management can include stimulation, bag and mask ventilation, intubation and ventilation. • Cardiorespiratory monitoring is essential to keeping track of potential problems. Pharmacological therapy such as caffeine can also be given to treat apnea in premature newborns. A positive airway pressure should be maintained, and neonatal sepsis must be ruled out What is the primary factor that initiates breathing in a newborn infant? • Potential neonatal respiratory problems include apnea, transient tachypnea of the newborn (TTNB), respiratory distress syndrome (RDS), meconium aspiration syndrome (MAS), airway obstruction, PPHN and pneumonia/Sepsis. • PPHN can be a result of idiopathic means or as a result of persistent pulmonary vascular resistance. The treatment involves treatment of the underlying cause, surfactant delivery, PPV, Nitric Oxide, HFV, ECMO, Prostglandins, steroids and Oxygen Energy metabolism • Energy metabolism in the fetus must be converted from a continuous placental supply of glucose to intermittent feeding. • While the fetus is dependent on maternal glucose as the main source of energy, it can use lactate, free-fatty acids, and ketone bodies under some conditions. • Plasma glucose is maintained by glycogenolysis • Glycogen synthesis in the liver and muscle begins in the late second trimester of pregnancy, and storage is completed in the third trimester Energy metabolism • Glycogen stores are maximal at term, but even then, the fetus only has enough glycogen available to meet energy needs for 8–10 hours, which can be depleted even more quickly if demand is high. Newborns will then rely on gluconeogenesis for energy, which requires integration, and is normal at 2–4 days of life. • Fat stores are the largest storage source of energy. At 27 weeks gestation, only 1% of a fetus' body weight is fat. At 40 weeks, that number increases to 16%. • Inadequate available glucose substrate can lead to hypoglycemia, fetal growth restriction, preterm delivery, or other problems. Similarly, excess substrate can lead to problems, such as infant of a diabetic mother (IDM), hypothermia or neonatal sepsis. Energy metabolism • Anticipating potential problems is the key to managing most neonatal problems of energy metabolism. For example, early feeding in the delivery room or as soon as possible may prevent hypoglycemia. • If the blood glucose is still low, then an intravenous (IV) bolus of glucose may be delivered, with continuous infusion if necessary. Rarely, steroids or glucagon may have to be employed. Temperature Regulation • Newborns come from a warm environment to the cold and fluctuating temperatures of this world. • They are naked, wet, and have a large surface area to mass ratio, with variable amounts of insulation, limited metabolic reserves, and a decreased ability to shiver. • Physiologic mechanisms for preserving core temperature include vasoconstriction (decrease blood flow to the skin), maintaining the fetal position (decrease the surface area exposed to the environment), jittery large muscle activity (generate muscular heat), and "non-shivering thermogenesis". Temperature Regulation • "non-shivering thermogenesis "occurs in "brown fat“ which is specialized adipose tissue with a high concentration of mitochondria designed to rapidly oxidize fatty acids in order to generate metabolic heat. • The newborn capacity to maintain these mechanisms is limited, especially in premature infants. As such, it is not surprising that some newborns may have problems regulating their temperature. As early as the 1880s, infant incubators were used to help newborns maintain warmth, with humidified incubators being used as early as the 1930s. Temperature Regulation • Basic techniques for keeping newborns warm include keeping them dry, wrapping them in blankets, giving them hats and clothing, or increasing the ambient temperature. More advanced techniques include incubators (at 36.5°C), humidity, heat shields, thermal blankets, double-walled incubators, and radiant warmers while the use of skin-to-skin "kangaroo mother care" interventions for low birth-weight infants have started to spread world-wide after its use as a solution in developing countries.[ Mechanical Ventilation • http://www.youtube.com/watch?v=dVqurKOJuD8 • http://www.youtube.com/watch?v=9gq34tkskkE • http://www.youtube.com/watch?v=EhQxO8pVy0A •Support devices •HFNC / NC •Transport •Servo 1 •Baby log •Neo Puff •HFV Jet •Avea •HFOV RT Equipment in NICU • Nasal Cannula (0.25-2L), typically set below 1L, always with a blender and a bubble humidifier. Used for oxygenation issues only, or A’s and B’s, weaning off of PPV • Oxyhood: set 7-12 L, with a heated humidifier, blender, temperature probe and O2 analyzer. Used when high FIO2 required/pneumos for Nitrogen washout • HFNC: used when higher flows are required up to 8L, given with heated humidifier/circuit and special cannula. Always use with a blender; may be used when weaning from CPAP/vent • NCPAP: used for persistent grunting/retractions where surfatant is not required. PEEP set from 2-6, given through prongs/mask, through a stand alone machine or through the ventilator RT Equipment in NICU • Nasal SIMV: Used through a SiPAP machine or ventilator, essentially the same as SIMV-PC except given through the nose • Mask CPAP/PPV through a flow inflating bag, may also give through a T-piece/NeoPuff for short term relief • Invasive mechanical ventilation: Through a ETT, typically set in SIMV mode in PC, or a volume targeted mode, rates set between 15-30, Pressures are set anywhere from 10-25, FIO2 kept as low as possible, IT anywhere from 0.2-0.8 seconds • HFV: given as Jet ventilation or HFOV • Nitric Oxide: typically given in tandem with HFV • ECMO: again given in tandem with HFV or mechanical ventilation Other equipment: HHN (although far less common in NICU), CPT via mini massager, ABG/CBG supplies, suction equipment, airway supplies) RT Equipment • NOTE: • All oxygen delivering equipment in the NICU and PICU setting will utilize a humidifier. High flow devices will use a heated humidifier • The use of a blender is also common with most equipment as is a oxygen analyzer • Use of aerosols are uncommon due to the noise factor; except for HHN • Suction pressures are lower, and flows and FIO2 levels are lower, as are PEEP levels Introduction • The primary objective of Mechanical Ventilation is to support breathing until patient respiratory efforts are sufficient. • First mechanical ventilation for a neonate in 1959. • One of the most important breakthroughs in the history of neonatal care. • Mortality from RDS decreased markedly after MV. • New Morbidity developed, CLD (BPD) Indications • Apnea (prolonged or repetitive unresponsive apnea associated with bradycardia or cyanosis). • Respiratory failure in newborns: PaO2 < 50 mmHg on FIO2 ≥ 0.6 PaCO2 > 60 - 65 mmHg (> 55 in infants < 1500 gm) pH < 7.20 • Impending ventilatory failure (worsening oxygenation and/or respiratory distress [↑ RR > 60 infants; > 40 children], retractions, grunting, nasal flaring even when ABG values are within acceptable ranges) (anticipation of worsening lung pathology) Indications • There are no well defined criteria for when to initiate MV in infants and children. Many clinical factors come into play and must be individualized for each patient's problem. Early intubation and MV is recommended in many situations: • Congenital anomalies affecting ventilatory function (diaphragmatic hernia) • Infants with low Apgar scores and responding poorly to resuscitation efforts • Infants with severe sepsis or compromised pulmonary blood flow (PPHN) • Premature babies < 1000 gm • Progressive atelectatic disease Indications • Scheduled surgical procedure • Any acute or chronic cardiopulmonary insufficiency • May be due to problem with lung, cardiovascular system, CNS, or various metabolic disorders Clinical signs: • Repeated A-B spells Indications • The oxygenation index is a calculation used to assess FIO2/Pressure requirements to achieve a PaO2 • A lower oxygenation index is better - this can be inferred by the equation itself. As the oxygenation of a person improves, they will be able to achieve a higher PaO2 at a lower FiO2. This would be reflected on the formula as a decrease in the numerator or an increase in the denominator - thus lowering the OI. Typically an OI threshold is set for when a neonate should be placed on ECMO, for example >40,>30 HFV Blood Gas Scoring System For Assisted Ventilation * A score of 3 or more indicates the need for CPAP or IMV. Ambient O2 failure → CPAP CPAP failure (10 cm H2O & FIO2 1.0) → IMV ** May indicate the need for CPAP or IMV by itself, if cyanotic heart disease not present. Contraindications • < 23 weeks gestation (?) or birth weight of less than 400 g (ref: NRP) • Congenital anomalies incompatible with survival (anacephaly, lethal genetic disorders) • Severe prolonged code with no reasonable chance of survival • NOTE: Parental involvement in the decision not to treat is vital. • Untreated/unvented pneumothorax (a contraindication for all PPV in all age populations) Neonatal Physiology Affecting Ventilation • Compliant chest wall and weak cartilaginous support of airways (excessive inspiratory efforts will collapse upper airway and lungs, increasing Raw and decreasing Vt) • Horizontal ribs and flatness of diaphragm reduce potential lung expansion and Vt • Peripheral Raw is 4x > than older children and adults • Distal airway growth lags behind proximal airway growth leading to increased peripheral Raw • Possible R-L shunting (PDA and/or foramen ovale) (L-R shunt through PDA increases the risk of pulmonary edema) Neonatal Physiology Affecting Ventilation • Increased risk of atelectasis and airway closure due to paucity of collateral ventilation between alveoli • Surfactant deficiency (↓ CL, ↓, FRC; may grunt and/or shorten Te to maintain FRC) • Postnatal clearance of lung liquid and ↑ pulmonary interstitial fluid • High metabolic rate • ↓ Muscle mass, ↓ oxidative capacity, ↓ Type 1 (slow twitch) muscle fiber Time Constant: An index of how rapidly the lungs can empty. • Time constant = Compliance X Resistance • In BPD time constant is long because of increased resistance. • In RDS time constant is short because of low compliance. • Normal = 0.12-0.15 sec Time Constant • • • • • • Inspiratory time must be 3-5 X time constant One time conststant = time for alveoli to discharge 63% of its volume through the airway. Two time constant = 84% of the volume leaves Three time constant = 95% of volume leaves. In RDS: require a longer I time because the lung will empty rapidly but require more time to fill. • In CLD: decrease vent rate, which allows to lengthen the I time and E time. Relationship to FRC Neonatal Ventilation • Time Cycled and Pressure Limited Ventilation with SIMV (most common type of conventional ventilation in the NICU) • Inspiration is stopped when the selected inspiratory time has been reached • PIP is the maximum amount of pressure exerted on the patient’s airway during the inspiration • Initial values = 16-20 cmH20 of PIP • Good chest rise and Good breath sounds Neonatal Ventilation Volume Controlled Ventilators: A preset volume of gas is delivered to the system after which inspiration is terminated. • When this gas has been delivered by the piston inspiration is terminated. • Tidal Volume • 4-6 ml/kg in low–birth-weight preemies • 5-8 ml/kg in term infants • 7-10 ml in pediatrics and adolescent patients • Volume losses by leaks from tubing system around the endotracheal tube. • Not common, unless using Volume targeted modes, such as with the Baby Log by Drager. Neonatal Ventilation • Peep = Positive pressure maintained in the patient’s airway during expiration; typically set between 3-5 cmH2O in most babies due to low FRC. Rarely do you go above 6 or below 3. • Prevents collapsed alveoli • Increases FRC • Improves compliance • Improves oxygenation • Decreases intrapulmonary shunting • Allows for lower PIPs to be used Mechanical Ventilation: Modes • All modes are available to the neonate • Time cycled IMV (with pressure limiting) • Newer neonatal vents may allow volume cycled IMV • Newer neonatal ventilators can do A/C volume cycle or pressure control Initial Setting on neonatal vent • Time cycled – Pressure Limited ventilator • PIP set 15 – 20 cm H20 • Achieve VT range of 4-6 ml/kg • Peep set 3 – 5 cm H2O (assess MAP, CXR 8-9 ribs expanded) • Rate set 20 – 40 bpm • Flow set 6 – 8 lpm • I time set .3 - .5 seconds for LBW and .5 - .8 seconds for larger infants • Keep alarms tight/set in SIMV mode, may use PSV 3-5 Settings • PIP – good chest excursion, good lung aeration • Vt in pressure control = PIP – PEEP • Vt in pressure control changes with change in compliance and resistance • PIP set – change only with changes in compliance and resistance in 2 cm increments Inspiratory Time Positive End Expiratory Pressure Managing Ventilator Settings Inspiratory Trigger Mechanism •Time –Controlled Mechanical Ventilation – NO patient interaction •Pressure –Ventilator senses a drop in pressure with patient effort •Flow –Ventilator senses a drop in flow with patient effort •Chest impedance / Abdominal movement –Ventilator senses respiratory/diaphragm or abdominal muscle movement •Diaphragmatic activity •NAVA- Neurally adjusted ventilatory assist •http://www.youtube.com/watch?v=fq2cna71G_o Target Values: MAP Mean Airway Pressure • Average pressure exerted on the airways from the start of one inspiration until the next • Is affected by IT, PIP, Rate, and PEEP • Baro/Volutrauma seen with values above 12 cmH2O • It is the most powerful influence on oxygenation! CPAP vs PEEP • Same distending alveolar pressure • PEEP is used in conjunction with ventilator rate • CPAP is used in spontaneously breathing patient, typically with use of nasal prongs or mask, not common with ETT in place, although PSV can be used along with CPAP Methods of administering CPAP • Endotracheal Tube • Patent airway, airway clearance • Disadvantage: plugging, malacia, infection • Nasal Prongs • Decrease infection, no malacia • Disadv. = plugging,pressure necrosis, gastric distention • Nasopharyngeal • Pressure necrosis, infection • Face Mask • Temporary measure prior to intubation or for apnea episode CPAP Indications: • Refractory Hypoxemia • PaO2 < 50 on an FIO2 of 60% or > • Many hospitals use 50% as the upper limit before changing to CPAP • Transitional therapy between simple O2 therapy and mechanical ventilation • Usually in the early stages of a disease or when recovery starts • Any disease that causes increased elastic resistance and alveolar instability CPAP: EFFECTS • Increased FRC , ie, back towards normal • Decreased shunt • Adequate PaO2 at minimal FIO2 • W.O.B. ? • By increasing FRC, CPAP should decrease the W.O.B. • However, it requires active exhalation which increases W.O.B. • To go on CPAP an infant needs to be breathing spontaneously and to have normal (or slightly lowered) PaCO2 CPAP: Administration Techniques • Mostly flow resistors • To change CPAP level, change either flow rate or the amount of resistance • May be administered via mask, nasal cannula, hood, or ET tube • An orogastric tube may be needed if using a mask, cannula, or hood •SiPAP machine •Bubble CPAP CPAP: Management Technique • Start at current FIO2 or slightly > • Start at 4-5 cmH2O • Titrate level in 1-2 cmH2O increments until PaO2 is acceptable • Watch pulse oximeter or TCM as well • Maximal level is usually 10-12 cmH2O Weaning: • Get FIO2 to 50% or < • Decrease CPAP in 1-2 cmH2O increments • Monitor for stability in vital signs, ABGs, and pulse oximeter • If on ET tube, extubate when CPAP is 2 cmH2O Delivery Systems (cont.) Delivery Systems (cont.) Delivery Systems (cont.) Delivery Systems (cont.) Delivery Systems (cont.) Delivery Systems (cont.) CPAP Hazard, breakdown of septum Common method • High flow nasal cannula: Although you are not setting a PEEP level, you are setting a flow rate up to 8L at max. The flow will create a expiratory resistance thus creating a small peep level. • Most HFNC start around 2-6 L, it is always heated to body temperature at 100% RH, using a heated humidifier; used as an alternative to CPAP or as a weaning tool from CPAP ET - CPAP in Pediatrics Pre and Post operatively to support structures • • • • • • Subglottic stenosis Cleft palate Laryngeal papillomas Neck tumors Tonsillitis epiglottitis Indications for NCPAP AARC Clinical Guidelines • Increased WOB with retractions, flaring, grunting and cyanosis • Inadequate ABG’s • Presence of poor expansion on CXR • Presence of conditions responsive to CPAP • RDS, Pulmonary edema, atelectasis, apnea, tracheal malacia, TTN Contraindications to NCPAP Guidelines • Upper airway abnormalities • TEF, choanal atresia (REQUIRE ETT) • Severe cardiovascular instability and impending arrest • Unstable respiratory drive • Ventilatory failure • NEC Hazards of NCPAP • • • • • • • • • • Hemodynamic compromise Pulmonary Baro/Volutrauma Gastric insufflation Air leaks Ventilation Perfusion Mismatch CO2 retention and increased WOB Increase in PVR due to impedence of blood flow Nasal irritation with septal distortion Pressure necrosis Nasal mucosal damage due to inadequate humidification Physiologic Deadspace • Physiologic = anatomic + alveolar • Anatomic = Gas that fills the airways and never participates in gas exchange • Alveolar = gas that goes to unperfused alveoli and thus never participates in gas exchange • Nl physiologic Vd in neonate = 2cc/kg Flow rate • Flow rate used determines the type of wave pattern • Goal is to set flow to allow maximum diffusion time without causing turbulent flow • Diffusion time is the length of time that the gas is in contact with the alveoli Flow Rate Target Values: ABGs • pH: 7.25 – 7.45 • PaCO2: 35-55 mmhg • Increased chances of intracranial bleed if above 55 mmhg • PaO2: 50 – 70 mmhg • Capillary is 35 – 50 mmhg • May allow permissive hypercapnia for severe prematurity to prevent VILI (BPD, PIE) • Capillary Blood gas ranges differ dramatically with pH 7.25-7.35 • CO2 45-60 • Trend ABG values using TCOM or ETCO2 and oxygenation using a pulse ox SpO2 Strategies to Prevent Non-Permissive Hypercapnia • Define optimum PaCO2 levels • Level to at which you will intervene • Level to at which you will wean • Ventilate at optimal FRC • Continuous monitoring of tidal volume • Use least pressure for maximal tidal volume • Facilitate spontaneous breathing • Consider “dual wean” of driving pressures • Consider pseudo-adaptive strategies Adjusting Ventilator Parameters • To change PaCO2 ONLY, change rate • To increase PaCO2 only, decrease rate • To decrease PaCO2 only, increase rate • To Change PaO2 ONLY, change FIO2, PEEP, or IT • FIO2 is changed in 1- 5 % increments • PEEP is changed in 1 – 2 cmH2O increments • To change both PaCO2 and PaO2 at the same time, but in opposite directions, change PIP • Increase PIP, PaO2 increases, PaCO2 decreases • Decrease PIP, PaO2 decreases, PaCO2 increases Adjusting Ventilator Parameters Peak Inspiratory Pressure (PIP): • Changes in PIP affect both PaO2& PaCO2by altering the MAP. • Increase in PIP:Increase in PaO2 • Decrease in PaCO2 • A high PIP should be used cautiously because it may increase the risk of volutrauma = air leak and BPD • Common mistake “large babies need higher PIP” requirement is strongly determined by compliance Adjusting Ventilator Parameters Rate: Change in rate alter alveolar minute ventilation • High rate low TV is strongly preferred • Rate change alone with constant I:E ratio do not alter MAP • Any change in inspiratory time that accompany change in rate will alter MAP Adjusting Ventilator Parameters FIO2:Changes alter Alveolar Oxygen Pressure Flow: Not well studied in infants • Minimal effects on ABG • In general 8-12 LPM • High Flow is needed with short inspiratory time to achieve adequate TV. Adjusting Ventilator Parameters Oxygenation Depends largely on the FIO2 • Oxygenation increase linearly with increase in MAP. • MAP is a measure of the average pressure to which the lungs are exposed. • Generally keep FIO2 lower than 40% if possible Increased I time and Inverse IE Ratios • Used when increasing FIO2 and PEEP is NOT raising PaO2 • Used for increased elastic resistance with short time constant • RDS, atelectasis, bilateral pneumonia • Rate should be no greater than 30 and PIP should be no greater than 30 cmH2O Monitoring During Mechanical Ventilation • Essential aspects of monitoring • Calculation of effective tidal volume • Close observation of the patient (vitals, ETT location, B/S…) • Noninvasive methods of determining oxygenation and ventilation status (SPO2, TCOM, ETCO2…) • Direct measurement of blood gas values (CBG, ABG…) Weaning from Mechanical Ventilation • Initiation • Significant resolution or reversal of the initial pathologic condition (note CXR, labs, vitals…) • Stable condition • Adequate nutrition • Able to breathe spontaneously Weaning from Mechanical Ventilation (cont.) • Initiation • Acceptable ventilator settings (FIO2 less than 40%, Rate low limit 10-15, PIP levels at minimum, PEEP 3-5) • Assessment of ventilatory muscle strength • VC, MIP, RSBI not assessed Weaning • Decrease FIO2 and PEEP (as already described for CPAP) • When rate is down to 10-12, try CPAP • Decrease PIP to 10-20 cmH2O • When stable on CPAP of 2 cmH2O and FIO2 of 40% or less, extubate • Start weaning with the parameter that is most extreme • Monitor for stability of vital signs, TCM values, and pulse oximeter values at all times Advancing Concepts • Automated regulation of the inspired oxygen (closed loop FIO2) • Partial support • Negative pressure ventilation Mechanical Ventilation: Hazards • Problems associated with increased mean ITP • Hemodynamic compromise, pulmonary baro/volutrauma • Mechanical failure • Usually human failure! • BPD, ie, Bronchopulmonary Dysplasia • http://www.youtube.com/watch?v=W0lGTifk3Hs Mechanical Ventilation: Hazards Mechanical Ventilation: Hazards • Pulmonary interstitial emphysema (PIE) is a collection of air outside of the normal air passages in the body and instead is found inside the connective tissue of the peribronchovascular sheaths, interlobular septa, and visceral pleura. • This collection develops as a result of alveolar and terminal bronchiolar rupture. Pulmonary interstitial emphysema is more frequent in premature infants who require mechanical ventilation for severe lung disease. • Causes: • Prematurity • Respiratory distress syndrome (RDS) • Meconium aspiration syndrome (MAS) • Amniotic fluid aspiration • Sepsis, or other infections • Mechanical ventilation HFV Definition: Ventilation at a high rate at least 2 –4 times the natural breathing rate, using a small TV that is less than anatomic dead space: • Types: High Frequency Jet Ventilator (HFJV)Up to 600 breath / min • High Frequency Flow Interrupter (HFFI)Up to 1200 breath / min • High Frequency Oscillatory Ventilator (HFOV)Up to 3000 / min High-Frequency Ventilation HFV Indications When conventional ventilation fails • –reduced compliance • Increased OI • –RDS/ARDS • –airleak/PIE • –meconium aspiration • –BPD • –pneumonia • –atelectases • –lung hypoplasia • –PPHN HFV Introduction • The respiratory insufficiency remains one of the major causes of neonatal mortality. • Intensification of conventional ventilation with higher rates and airway pressures leads to an increased incidence of barotrauma. • Either ECMO or high-frequency oscillatory ventilation might • resolve such desperate situations. • Since HFOV was first described by Lunkenheimer in the early • seventies this method of ventilation has been further developed and is now applied the world over. HFV There are three distinguishing characteristics of • high-frequency oscillatory ventilation: • The frequency range from 5 to 50 Hz (300 to 3000 bpm) • active inspiration and active expiration • Tidal volumes: about the size of the deadspace volume HFV HFV Oscillators provide active inspiration and active expiration with sinusoidal waveforms: • Piston oscillators move a column of gas rapidly back and forth in the breathing circuit with a piston pump. • Its size determines the stroke volume, which is therefore fairly constant. A bias flow system supplies fresh gas HFV The "flow-interrupters" chop up the gas flow into the patient circuit at a high rate, thus causing pressure oscillations. Their power, however, depends also on the respiratory mechanics of the patient Three parameters determine oscillatory ventilation: • Firstly, there is the mean airway pressure (MAP): around which the pressure oscillates. • Secondly, the oscillatory volume: which results • from the pressure swings and essentially determines the effectiveness of this type of mechanical ventilation. • Thirdly, the oscillatory frequency: the number of cycles per unit of time. HFV • MAP set 3-5 higher than conventional ventilator MAP, adjust with bias flow, increased for lung expansion and oxygnation • AMP (set with power) • The term amplitude has stood for pressure amplitude. • In the end, however, ventilation does not depend on the pressure amplitude but on the oscillatory volume. • as a setting parameter the amplitude is one of the determinants of oscillatory volume. • The oscillatory volume exponentially influences CO2 elimination • During HFV volumes similar to the deadspace • volume (about 2 to 2.5 ml/kg) should be the target. HFV In any HF ventilator, the oscillatory volume depends characteristically on the oscillatory frequency. Normally, lower frequencies permit higher volumes. Even small changes in resistance and/or compliance of the respiratory system, e.g. by secretion in the airways, or through the use of a different breathing circuit or ET tube, can change the oscillatory volume and thus the effectiveness of HFV. Hertz set 10-15 HFV Oscillatory ventilation on its own can be used in the CPAP mode, or with superimposed IMV strokes, usually at a rate of 3 to 5 strokes per minute. • The benefit of the IMV breaths is probably due to the opening of uninflated lung units to achieve further ‘volume recruitment’. • Sometimes very long inspiratory times (15 to 30 s) are suggested for these sustained inflations Bunnell Life Pulse Jet Ventilator Hi-Lo Jet Endotracheal Tube SensorMedics 3100A/3100B HFOV Circuit Considerations • Very low circuit compliance (typically secured to warmer) • Intrinsic timing mechanisms • Control over inspiratory times • Sufficient time for gas egress • Adequately humidify gases • Alarms and fail-safe devices Ventilator Management • Initial management • Proper gas temperature and humidity • Ventilator and circuit position • Initial settings are lower than anticipated • Appropriate primary therapies Clinical Management Strategies • High-volume strategy • Optimize lung inflation • Minimize ventilation-perfusion Sustained Inflations • Applying plateau pressures at levels in excess of expected alveolar opening pressures for periods of 5 to 30 seconds Clinical Management Strategies • Low volume • Allows the lung to slowly deflate or minimizes ongoing air leakage • Provides tolerable ventilation while accepting a higher FIO2 Weaning • Minute ventilation • HFFI and HFOV • Reducing oscillatory amplitude during • HFJV • Decreasing peak pressure and on time • mPaw • Radiographic assessment of lung volume • FIO2 Care of the Patient • Positioning • Endotracheal tube • Suctioning (keep at a minimum during HFV) • Monitoring (assess chest wiggle from clavicles to mid belly) Troubleshooting • Chest wall movement (increase AMP for decreased movement, increase MAP per CXR expansion) • Cardiac output • Pathology • Specific for equipment Drager Babylog 8000 plus •Used at Kaiser, Vol, Guaranteed, essentially PRVC Sechrist IV-200 SAVI Viasys Avea Drager Evita 4/XL Puritan-Bennett 840 •Used at Redlands Maquet Servo i Hamilton-G5 GE Healthcare Engstrom Carestation Puritan-Bennett Companion 2801 Philips Respironics Lifecare PLV102 LTV 900/950/1000 Newport HT- 50