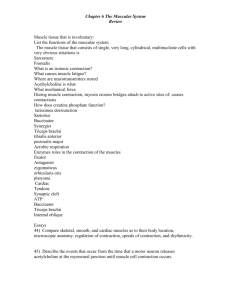
Physiology Ch. 9 p101-112 [4-25
advertisement

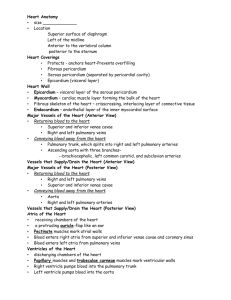
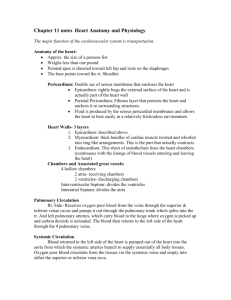
Physiology Ch. 9 p101-112 Cardiac Muscle; the Heart as a Pump and Function of the Heart Valves Physiology of Cardiac Muscle – atrial muscle, ventricular muscle, and excitatory/conductive muscle fibers exist: atrial and ventricular are able to contract same way as skeletal muscle except that contraction is longer -excitatory/conductive fibers don’t contract but rather exhibit rhythmic electric discharge -cardiac muscle is striated like skeletal muscle and has myofibrils with actin and myosin filaments Cardiac Muscle as a Syncytium – intercalated discs are cell membranes that separate individual cardiac muscle cells from each other, but are fused with one another through gap junctions that allow ions to move freely through intracellular fluid along longitudinal axis of muscle fibers so potentials travel easy -thus, cardiac muscle is a syncytium of interconnected cells that all become excited by action potential -atrial syncytium composes walls of atria, and ventricular syncytium composes walls of ventricles Action Potentials in Cardiac Muscle – action potentials average 105mV, raising potential from -85mV to +20mV during each beat. After initial spike, membrane remains depolarized for 0.2s showing plateau followed by repolarization -plateau causes ventricular contraction to last 15x as long in cardiac muscle than skeletal muscle -Skeletal muscle has fast sodium channels that allow rapid contraction -Cardiac muscle has 2 channels that cause action potential 1. Fast Sodium Channels 2. Calcium-sodium channels – slower to open and remain open for several tenths of a second when large amounts of Ca and Na ions flow inside to cause plateau in action potential a. Calcium also activates muscle contraction process -another reason that accounts for prolonged action potential is that permeability to K+ ions decreases fivefold after an action potential which does NOT occur in skeletal muscle, and causes plateau to prevent early return of resting membrane potential -results from excess Ca influx through Ca/Na channels Velocity of Cardiac Conduction – along atrial and ventricular muscle fibers, conduction is 0.3-0.5m/s -velocity in purkinje fibers is 4m/s which allows rapid conduction to different parts of the heart -cardiac muscle is refractory toward new stimulation during action potential -normal refractory period is 0.25-0.3s at plateau phase -There is an additional refractory period of 0.05s after action potential where it is difficult to excite, but can still happen to form an early, premature contraction -refractory period of atria shorter than that of ventricles Excitation-Contraction Coupling – Function of Ca ions and transverse Tubules – excitation-contraction refers to mechanism by which action potential causes myofibrils of muscle to contract -when action potential (AP) passes over cardiac muscle membrane, it spreads to interior of muscle fiber along transverse T tubules, which in turn act on membranes of longitudinal sarcoplasmic tubules to release Ca ions into muscle sarcoplasm for sarcoplasmic reticulum. -Ca diffuses into myofibrils and causes sliding of actin/myosin along one another for contraction -Another difference in cardiac muscle is that in addition to Ca ions released into sarcoplasm for sarcoplasmic reticulum, Ca ions also diffuse from T tubules at the time of action potential, which opens voltage-dependent calcium channels in membrane of T tubules. -Ca entering cell activates Ca Release Channels (Ryanodine Receptor Channels) in the sarcoplasmic reticulum membrane, which interact with troponin to initiate cross-bridge formation and contraction -Without Ca from T tubules, strength of cardiac muscle contraction would be reduced because sarcoplasmic reticulum of cardiac muscle is not as developed as skeletal muscle -T tubules 5x as wide in cardiac muscle as skeletal muscle, contain mucopolysaccharides -strength of cardiac contraction depends on concentration of Ca ions in extracellular fluids -quantity of Ca in T tubules depends on extracellular fluid Ca concentration -Skeletal muscle hardly affected by extracellular fluid Ca because it is only dependent of that inside -at the end of plateau phase, influx of Ca into muscle is cut off, and are rapidly pumped out of fibers into both sarcoplasmic reticulum and T tubule through a calcium-ATPase pump and a sodium-calcium exchanger Duration of Contraction – cardiac muscle contracts few ms after action potential begins and continues until few ms after AP ends. About 0.2s in atria and 0.3s in ventricular muscle Cardiac Cycle – events that occur from beginning of one heartbeat to the beginning of the next -initiated by action potential in the sinus node atria AV node/bundle ventricles -there is a delay in AV node allowing atria to conduct 0.1s before ventricle, thus atria act as primer pumps for ventricles, and ventricles provide major source of power for blood movement Diastole and Systole – cardiac cycle consists of period of relaxation (diastole) when heart fills with blood followed by a period of contraction called systole -total duration of cardiac cycle including systole and diastole is reciprocal of heart rate -if HR is 72 bpm, duration of cardiac cycle is 1/72 beats/min Effect of HR on Cardiac Cycle – hen HR increases, duration of each cardiac cycle decreases, including systole and diastole -duration of action potential and systole decrease, but not as much as diastole -systole comprises 0.4 of entire cardiac cycle, and at 3x normal rate, systole is 0.65 of total cardiac cycle meaning heart does not remain relaxed long enough to allow complete filling of chambers before the next contraction Relationship of ECG to Cardiac Cycle – P wave is caused by spread of depolarization through atria followed by atrial contraction right after P wave. -about 0.16s after P wave, QRS waves appear for ventricular depolarization which initiate contraction of ventricles and causes ventricular pressure to rise. QRS complex slightly before ventricular systole -ventricular T wave on ECG is repolarization of ventricles which occurs slightly before the end of ventricular contraction Function of Atria as Primer Pumps – blood flows continually from great veins into atria, and 80% of blood flows directly through atria into ventricles even before atria contract -atrial contraction causes additional 20% to fill ventricles, but extra 20% is not needed because heart can pump 400% more blood than is required -if atria fail to function, difference is unlikely to be noticed unless person exercises Pressure Changes in the Atria – a,c, and v waves in the atrial pressure curve -the a wave is caused by atrial contraction; R atrial pressure is 5mmHg and L atrial pressure is 7mmHg -the c wave is when ventricles begin to contract and causes slight backflow into atria -the v wave is at the end of ventricular contraction resulting from slow flow of blood into atria from veins while AV valves are closed during ventricular contraction Filling of the Ventricles During Diastole – ventricular systole causes blood to accumulate in R and L atria because of closed AV valves, and when systole is over and ventricular pressures fall, the increased pressures that developed in atria push AV valves open and allow blood to flow into ventricules, this is called period of rapid filling of ventricles -rapid filling lasts for first third of diastole, middle third a small amount of blood flows into ventricles, and the last third the atria contract to give additional thrust of 20% of rest of blood Emptying of Ventricles During Systole – first is the period of isovolumic (isometric) contraction. -after ventricular contraction begins, pressure in ventricles rises causing AV valves to close, and in another 0.02s, pressure rises enough to open semilunar (aortic and pulmonary) valves open against pressures of aorta and pulmonary artery -during this period, contraction is occurring but there is no emptying (isovolumic/isometric contraction) meaning tension is increasing in muscle but no shortening of muscle occurs Period of Ejection of Ventricle – when L ventricular pressure >80mmHg and R vent pressure > 8mmHg, ventricular pressures push semilunar valves open and 70% of blood pours out during first 1/3 of ejection and remaining 30% during last 2/3rds -1st 1/3 is called period of rapid ejection, last 2/3 is called period of slow ejection Period of Isovolumic/isometric Relaxation – at the end of systole, ventricular relaxation begins to allow both R and L intraventricular pressures to decrease rapidly, causing blood in great arteries to push blood back towards ventricles, which snaps aortic and pulmonary valves closed, and afterwards ventricular muscle still relaxes without changing volume, called isovolumic or isometric relaxation, once pressures decrease back to normal, AV valves open back up again to begin new cycle End-diastolic Volume, End Systolic Volume, and Stroke Output Volume 1. End-diastolic volume – normal filling of ventricles increases volume of each ventricle to 110120mL during diastole 2. Stroke Volume Output – as ventricles empty during systole, volume decreases to 70mL 3. End Systolic Volume – the amount of blood remaining in each ventricle (40-50mL) 4. Ejection Fraction – fraction of end-diastolic volume that is ejected Function of the Valves 1. Atrioventricular Valves – AV valves are the tricuspid and mitral valves, and they prevent backflow of blood from ventricles to atria during systole, require almost no backflow to cause closure 2. Semilunar Valves – are aortic and pulmonary valves that prevent backflow from aorta and pulmonary arteries during diastole, and open passively when pressure gradient moves blood backward Function of Papillary Muscles – papillary muscles attach to AV muscles by chordae tendinae, and contract when ventricular walls contract but do NOT help valves close. -they prevent the vanes of valves from bulging too far backward toward atria during ventricular contraction, abnormality of which can cause leakage back into atria Aortic and Pulmonary Valves – aortic and pulmonary artery semilunar valves are different from AV valves -high pressure in arteries at the end of systole cause semilunar valves to snap closed -due to smaller openings velocity of blood ejection is greater than through AV valves -due to pressure and velocity of blood, these valves subject to greater mechanical abrasion -semilunar valves are NOT supported by chordae tendinae Aortic Pressure Curve – left ventricular contraction causes pressure in ventricle to increase and allow aortic valve to open, after which pressure in ventricle rises much less rapidly because blood flows out -entry of blood into arteries causes walls to stretch and pressure to increase to 120mmHg -at the end of systole after L ventricle stops ejecting blood and aortic valve closes, elastic walls of arteries maintain high pressure in arteries even during diastole -an incisura occurs in the aortic pressure curve when aortic valve closes caused by short period of backflow of blood immediately before closure of valve followed by cessation of backflow -After aortic valve closed, pressure in aorta decreases slowly throughout diastolebecause blood stored in elastic arteries flows continually through peripheral vessels back toward veins -Pressure curves in R ventricle and pulmonary artery are similar to aorta but 1/6 as great Relationship of Heart Sounds to Pumping – when valves close, vanes of valves vibrate due to sudden pressure changes to give off a sound that travels through chest -when ventricles contract, you first hear sound of AV valve closure, known as first heart sound -when aortic and pulmonary valves close at the end of systole, you hear a rigid snap due to rapid closure, which is the second heart sound Work output of Heart – stroke work output is amount of energy that heart converts to work during each heartbeat while pumping blood into arteries -minute work output is the total amount of energy converted to work in 1min, = to stroke output times HR/minute -Work output is in 2 forms: -major proportion is used to move blood from low-pressure veins to high-pressure arteries, called volume-pressure work or external work -minor proportion of energy is used to accelerate blood to its velocity of ejection through aortic and pulmonary valves, called kinetic energy of blood flow Graphical Analysis of Ventricular Pumping – diastolic pressure curve is determined by filling the heart with progressively greater volumes of blood and then measuring diastolic pressure immediately before ventricular contraction, which is end-diastolic pressure -systolic pressure curve is determined by recording systolic pressure during ventricular contraction at each volume of filling -during ventricular contraction, systolic pressure increases even at low ventricular volumes and reaches a max ventricular volume at 150-170mL -as volume increases further, systolic pressure actually decreases because actin/myosin filaments of muscle fibers are pulled apart far enough that strength of each contraction is less Volume-pressure diagram during cardiac cycle – four phases in filling left ventricle: 1. Period of Filling – this phase begins at ventricular volume of 50mL and diastolic pressure of 23mmHg. Amount of blood remaining in ventricle after previous heartbeat is called end-systolic volume 2. Period of Isovolumic Contraction – during isovolumic contraction, volume of ventricle does not change because valves are closed, but pressure inside ventricles increases to equal aortic pressure 3. Period of ejection – during ejection, systolic pressure rises even higher due to more ventricular contraction and volume decreases because aortic valve has opened up and blood flows out 4. Period of Isovolumic Relaxation – at the end of ejection period, aortic valve closes and ventricular pressure falls back to diastolic pressure without change in volume -when heart pumps large quantities of blood, area of work diagram becomes much larger and extends to the right because ventricle fills with more blood during diastole Concepts of Preload and Afterload – Preload is the tension of cardiac muscle when it begins to contract, and afterload is the load against which muscle exerts its contractile force -preload is usually considered to be the end-diastolic pressure when ventricle has been filled -Afterload of ventricle is pressure in aorta leading from ventricle (described by phase 3 of curve) Chemical Energy Required for Cardiac Contraction: O2 Utilization of Heart – heart muscle uses chemical energy to provide work of contraction, most of which comes from fatty acid metabolism and some from lactate and glucose -since fatty acids require oxidation for metabolism, rate of O2 consumption can measure chemical energy liberated while heart performs work -external work – O2 consumption and chemical energy expended during contraction -potential energy – additional work that could be accomplished by contraction of ventricle if the ventricle should empty all of its blood -O2 consumption has been shown to be proportional to the tension in heart muscle during contraction multiplied by the duration of time of contraction, which is called the tension-time index -since tension is high when systolic pressure is high, more O2 is used -more O2 used during normal pressures but abnormal ventricular dilation because heart muscle is more tensed, becomes important in heart failure Efficiency of Cardiac Contraction – most of expended chemical energy is converted to heat, and a smaller amount to work output. Ratio of work output to total chemical energy is the efficiency of heart -maximum efficiency of heart is 20-25%, and in heart failure it is 5-10% Regulation of Heart Pumping – At rest, heart pumps 4-6 liters of blood/minute, and 5x during exercise -volume pumped is regulated by intrinsic cardiac regulation in response to volume changes, and control of heart rate by autonomic nervous system Intrinsic Regulation of Heart Pumping – Frank-Starling Mechanism – amount of blood pumped by heart/min determined entirely by rate of flow into heart from veins called venous return -each peripheral tissue of body controls its own local blood flow and combine into big veins R atrium -intrinsic ability of the heart to adapt to increasing volumes of inflowing blood is called Frank-Starling Mechanism, meaning greater the heart muscle is stretched during filling, the greater is the force of contraction and greater amount of blood pumped into aorta. -Heart pumps all the blood that returns to it by the veins -when extra blood flows into ventricles, cardiac muscle is stretched to greater length. Actin and myosin filaments are brought to a more optimal overlap for force generation, and so heart contracts more forcefully -another factor that increases pumping when volume is increased is that stretch of R atrial wall directly increases HR by 10-20% to increase amount of blood each minute Ventricular Function Curves – help express functional ability of ventricles to pump blood -a type of ventricular function curve is a stroke work output curve, where atrial pressure of each side of heart increases, stroke work output of that side increases until it reaches limit of ventricle’s pumping ability -ventricular volume output curve – represent function of two ventricles of human heart based on data from lower animals, and as R and L atrial pressure increase, ventricular volume also increases -Ventricular function curves are another way of expressing Frank-Starling Mechanism where ventricles fill in response to high atrial pressures and ventricular volume/strength of cardiac muscle contraction increase causing heart to pump increased quantities of blood into arteries Control of heart by Sympathetic and Parasympathetic Nerves –for fiven levels of atrial pressure, amount of blood pumped each minute can be increased to 100% by sympathetics, and decreased to 0 by parasympathetic (vagal) stimulation 1. Sympathetic – can increase HR from 70bpm to 200bpm, and increase force of contraction to 2x to increase volume of blood pumped and increasing ejection pressure a. Sympathetic stimulation increases maximum cardiac output 2-3x b. Inhibition of sympathetic nerves can decrease cardiac pumping because under normal conditions, sympathetic nerves to the heart discharge continuously at a slow rate that maintains pumping at about 30% above that with no sympathetics i. When sympathetics are depressed, HR and strength of contraction decreases 2. Parasympathetic – parasympathetic fibers in the vagal nerves can stop heartbeat for few seconds but then heart escapes and beats at a rate of 20-40bpm as long as this continues a. Vagal fibers are mainly innervating atria and not much to ventricles where power of contraction occurs, which is why parasympathetic stimulation decreases HR but not strength of contraction Effect of Symp or Parasymp stimulation on Cardiac Function Curve – at any given R atrial pressure, cardiac output increases during sympathetic stimulation and decreases during parasympathetic stimulation -these changes result from changes in heart rate AND changes in contractile strength Effect of K+ and Ca+ Ions on Heart Function – excess K+ in extracellular fluids cause heart to be dilated and flaccid and slows HR, and large quantities can block conduction through AV bundle -these result from high K+ in extracellular fluid decreases resting membrane potential in cardiac muscle to partially depolarize the membrane and cause intensity of action potential to decrease to make contraction weaker -Excess calcium ions cause effects opposite to K+, causing heart to go into spastic contraction due to direct ability of Ca ions to initiate cardiac contractile process -deficiency of Ca ions causes cardiac flaccidity similar to high K+ ions Effect of Temperature on Heart – increased body temp during fever increases heart rate sometimes up to double of normal, and decreased temperature causes decreased heart rate, resulting from the fact that heat increases permeability of cardiac muscle membrane to ions that control heart rate -contractile strength of heart increases with increasing temperature like during exercise, but prolonged heat causes weakness Increasing Arterial Pressure Load Does NOT Decrease Cardiac Output – increasing aortic pressure does not decrease cardiac output until mean arterial pressure rises above 160mmHg