Physiology (cont.)
advertisement
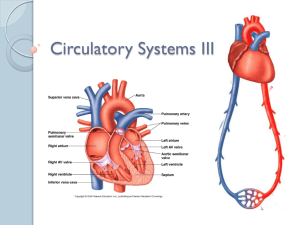
Chapter 9: Cardiac Muscle; The Heart As A Pump and Function of the Heart Valves Guyton and Hall, Textbook of Medical Physiology, 12th edition Physiology of Cardiac Muscle • Physiologic Anatomy a. b. c. d. Muscle fibers arranged in a latticework Striated and Involuntary Actin and myosin, typical myofibrils Sliding filament mechanism Fig. 9.1 Structure of the heart and blood flow through it. Physiology (cont.) • Cardiac Muscle as a Synctium-cardiac muscle fibers are made up of many individual cells connected in series and in parallel (intercalated discs) Fig. 9.2 Synctium Physiology (cont.) a. Composed of two synctiums: atrial and ventricular b. Disks allow the action potential to travel easily from cell to cell • Action Potentials in Cardiac Muscle a. What causes the long action potential and plateau? b. The AP is caused by the opening of two channel types 1. The same fast Na+ channels as in skeletal muscle 2. Slow Ca++ channels (slower to open and close) 3. Longer period of depolarization leads to plateau Fig. 9.3 Rhythmic AP+s from Purkinje fibers and a ventricular muscle. Physiology (cont.) c. Permeability for K+ decreases about 5-fold d. Prevents an early return to depolarized state • Velocity of Signal Conduction • Refractory Period of Cardiac Muscle a. Refractory to restimulation during the AP b. Ventricle; 0.25-0.30 sec. which is the duration of the plateau c. There is an additional relative refractory period Fig. 9.4 Force of ventricular heart muscle contraction, showing the duration of the refractory period and relative refractory period, plus the effect of premature contraction. Note that there is no summation as occurs in skeletal muscle. Physiology (cont.) • Excitation-Contraction Coupling Fig. 9.5 • Excitation-Contraction Coupling (cont.) a. Calcium enters from extracellular fluid b. Triggers calcium release from SR c. At the end of the plateau, calcium flow stops and calcium is reabsorbed by the SR Cardiac Cycle • Cardiac Cycle-events from the beginning of one heartbeat to the beginning of the next a. Cycle is initiated by the spontaneous generation of an AP by the sinus node b. Delay of 0.1 sec from the atria to the ventricle which allows the atria to contract before the ventricles • Diastole-relaxation • Systole-contraction Fig. 9.6 Events of the cardiac cycle Cardiac Cycle (cont.) • Effect of Heart Rate on the Duration of the CycleAs heart rate increases, the duration of the cycle decreases • Relationship of the ECG to the Cycle-electrical voltages generated by the heart a. P wave-spread of depolarization through the atria followed by atrial contraction b. QRS waves-electrical depolarization of the ventricles c. T wave-repolarization of the ventricles Cardiac Cycle (cont.) • Function of the Atria as a Primer Pump-about 80% of the blood flows directly through the atria to the ventricles; atrial contraction adds another 20% so it functions as a primer pump • Pressure Changes in the Atria-in Figure 9.6 there are three minor pressure elevations a. a wave-caused by atrial contraction b. c wave-occurs when the ventricles begin to contract c. v wave-occurs at the end of ventricular contraction Cardiac Cycle (cont.) • Function of the Ventricles as Pumps-period of of rapid filling; lasts about the first third of diastole; a small amount fills during the second third and the atrial contraction fills the last third Emptying of the Ventricles During Systole • Period of Isovolumic Contraction a. Ventricular pressure rises as contraction begins b. Initially the pressure is not sufficient to open the semilunar valves c. Therefore, contraction is occurring but no emptying • Period of Ejection a. Pressure >80 mm Hg pushes the semilunar valves open b. Period of rapid ejection-first third (70%) c. Period of slow ejection-second 2/3 (30%) • Period of Isovolumic Relaxation a. At the end of systole, ventricles relax quickly b. Blood in the arteries push back and close the semilunar valves c. Ventricles continue to relax but volume does not change • End Diastolic Volume-during diastole, volume of the ventricles increases to about 110-120 ml • Stroke Volume Output-as ventricles empty during systole, the volume decreases about 70 ml • End Systolic Volume-remaining volume in the ventricle (40-50 ml) • Ejection Fraction-fraction of the end diastolic that is ejected (60%) Function of the Valves • Atrioventricular Valves (tricuspid and mitral) a. Prevent backflow from the ventricles to the atria b. Close and open passively Fig. 9.7 Valves (cont.) • Function of the Papillary Muscles-attach to the AV valves by the chordae tendineae; prevent the valves from bulging back into the atria • Aortic and Pulmonary Artery Valves a. Because of smaller openings the velocity of flow is greater than with the AV valves b. Subject to greater mechanical abrasion than AVs c. No chordae tendineae • Relationship of Heart Sounds to Heart Beating a. First sound is closure of the AV valves b. Second sound is closure of the SL valves c. Lub-Dub • Work Output of the Heart a. Stroke work output-amount of energy the heart converts to work during each heartbeat b. Minute work output-total amount of energy converted to work in one minute c. Volume-pressure work and kinetic energy of blood flow Graphic Analysis of Ventricular Pumping Fig. 9.8 Relationship between left ventricular volume and intraventricular pressure during diastole and systole. Heavy red lines indicate the volume pressure diagram (EW-external work). Volume-Pressure Diagram During the Cardiac Cycle • Phase I: Period of Filling • Phase II: Period of Isovolumic Contraction • Phase III: Period of Ejection • Phase IV: Period of Isovolumic Relaxation Fig. 9.9 • Preload-the degree of tension on cardiac muscle when it begins to contract; usually is the enddiastolic pressure when the ventricle has filled • Afterload-pressure in the aorta leading from the ventricle; Energy Requirements • Oxygen Utilization By the Heart a. 70-90% from the oxidative metabolism of fatty acids b. 10-30% from lactate and glucose • Efficiency of Cardiac Contracton a. Most of the chemical energy is converted to heat b. 20-25% max. efficiency of the normal heart c. As low as 5-10% in heart failure Regulation of Heart Pumping • Intrinsic Regulation of Heart Pumping—Frank-Starling Mechanism-intrinsic ability of the heart to adapt to increasing volumes of inflowing blood a. Within physiologic limits, the heart pumps all the blood that returns to it by way of the veins b. Muscle stretches and brought to optimal degree of overlap for contraction c. Stretch of the right atrial muscle increases the heart rate by 10-20% Ventricular Function Curves : Another Way of Expressing the Frank-Starling Mechanism 9.10 Left and right ventricular function curves Fig. 9.11 Normal right and left ventricular output Control by the ANS • Excitation by the Sympathetic Nerves a. Stimulation can increase heart rate from 70 bpm to 180-200 bpm b. Increases the force of contraction two-fold c. Increases the volume pumped and the ejection pressure d. Inhibition decreases the heart rate and strength of contraction ANS Control (cont.) • Parasympathetic (Vagal) Stimulation a. Strong stimulation will stop the heart for a few seconds; then 20-40 bpm b. Decrease the strength of contraction 20-30% c. Distributed mainly to the atria Fig. 9.12 Cardiac sympathetic and parasympathetic nerves Fig. 9.13 Effect on the cardiac output curve of different degrees of sympathetic and parasympathetic stimulation Effects of Potassium and Calcium Ions on Heart Function • Potassium Ions a. Excess causes the heart to become flaccid and dilated and slows heart rate b. Excess can block conduction through the AV bundle c. Contraction becomes progressively weaker • Calcium Ions a. Excess causes the heart to go to spastic contractions b. Deficiency causes flaccidity c. Regulated within a narrow range so seldom important clinically Effect of Temperature on Heart Function • Effects of Temperature a. Increase body temperature increases heart rate b. Decrease body temp. decreases heart rate c. Contractile strength enhanced by moderate increases in temperature d. Prolonged elevation eventually causes weakness