Heart Notes
advertisement

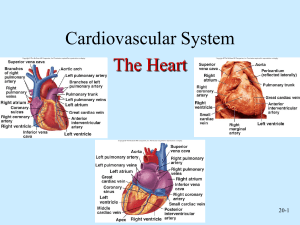
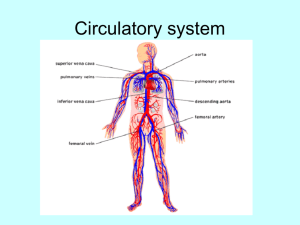
Chapter 11 notes Heart Anatomy and Physiology The major function of the cardiovascular system is transportation. Anatomy of the heart: Approx. the size of a persons fist Weighs less than one pound Pointed apex is directed toward left hip and rests on the diaphragm The base points toward the rt. Shoulder Pericardium: Double sac of serous membrane that encloses the heart Epicardium: tightly hugs the external surface of the heart and is actually part of the heart wall Parietal Pericardium: Fibrous layer that protects the heart and anchors it to surrounding structures. Fluid is produced by the serous pericardial membranes and allows the heart to beat easily in a relatively frictionless environment. Heart Walls- 3 layers 1. Epicardium: described above 2. Myocardium: thick bundles of cardiac muscle twisted and whorled into ring like arrangements. This is the part that actually contracts. 3. Endocardium: This sheet of endothelium lines the heart chambers. (continuous with the linings of blood vessels entering and leaving the heart) Chambers and Associated great vessels: 4 hollow chambers 2 atria- receiving chambers 2 ventricles- discharging chambers Interventricular Septum: divides the ventricles Interatrial Septum: divides the atria Pulmonary Circulation Rt. Side- Receives oxygen poor blood from the veins through the superior & inferior venae cavae and pumps it out through the pulmonary trunk which splits into the rt. And left pulmonary arteries, which carry blood to the lungs where oxygen is picked up and carbon dioxide is unloaded. The blood then returns to the left side of the heart through the 4 pulmonary veins. Systemic Circulation Blood returned to the left side of the heart is pumped out of the heart into the aorta from which the systemic arteries branch to supply essentially all body tissues. Oxygen poor blood circulates from the tissues via the systemic veins and empty into either the superior or inferior vena cava. Left ventricle walls are much thicker than rt., Because it must pump blood over a much longer pathway through the body. Valves 4 valves allow blood to flow in only one direction through the heart chambers. Atrioventricular valves (AV) located between the atrial and ventricular chambers on each side. ( prevent back flow into the atria when the ventricles contract) Left AV- bicuspid or mitral valve Rt. AV- tricuspid valve Semilunar valves: guards the bases of the two large arteries leaving the ventricular chambers Pulmonary semilunar valve Aortic semilunar valve AV valves are open during heart relaxation and closed during ventricle contraction Semilunar valves are closed during heart relaxation and forced open when ventricles contract. Cardiac Circulation: The blood supply that oxygenates and nourishes the heart is provided by the rt. and left coronary arteries. The myocardium is drained by several cardiac veins which empty into an enlarged vessel on the backside of the heart called the coronary sinus, which empties into the rt. atrium. When the heart beats rapidly myocardium may not receive enough blood (blood is only able to flow during relaxation periods) Angina pectoris: chest pain resulting from oxygen deprived myocardium Myocardial infarction: Heart attack- prolonged angina in which the ischemic heart cells die. Physiology of the heart: In one day the heart pushes the body’s supply of approx. 6 quarts of blood through the blood vessels over 1000 times. It actually pumps 6000 quarts in a day. Unlike skeletal muscle, cardiac muscle cells can and do contract spontaneously and independently, even if all nervous connections are severed. Muscle cells in different areas of the heart have different rhythms Ventricular cells- 20-40/minute Arterial-60/minute 2 types of controlling systems: 1. Nerves of the autonomic nervous system act as ‘brakes” and “accelerators” to decrease or increase heart rate depending on which division is activated. 2. Intrinsic conduction system (ICS or nodal system) a. Built into the heart tissue b. Special tissues found nowhere else c. Cross between muscle and nervous tissue d. Causes heart muscle to depolarize in only one direction e. Enforces a contraction rate of approximately 75 beats/min. helping the heart to keep beating as a coordinated unit Sinoatrial Node (SA) Right Atrium- most important part of ICS Atrioventricular (AV) node Junction of the atria and ventricles SA node starts each heartbeat and sets the pace for the whole heart. (Pacemaker) Damage to the AV node can partially or totally release the ventricles from the control of the SA node- ventricles beat at their own rate. This condition is called heart block. Damage to the SA node- placement of artificial pacemaker Ischemia: lack of adequate blood supply to the heart muscle; may cause fibrillation. Fibrillation: Uncoordinated rapid shuddering of the heart muscle, which makes the heart useless. This is a major cause of death from heart attacks in adults. Tachycardia: rapid heart rate (over 100/min) Prolonged tachycardia may lead to fibrillation Bradycardia: slower than normal HR (under 60/min) Systole: heart contraction Diastole: Heart relaxation Cardiac cycle: The events of one complete heart beat, during which both atria and ventricles contract and then relax.(normally 0.8 second) Mid to late diastole Ventricular systole Early diastole Cardiac Output (CO): Amount of blood pumped out by each side of the heart in 1 minute. (product of HR and Stoke volume) Stoke Volume: volume of blood pumped out by a ventricle with each heart beat. Regulation of Stroke Volume: Starling’s law of the heart: critical factor controlling stroke volume is how much the cardiac muscle cells are stretched just before they contract. Anything that increases volume or speed of venous return increases stroke volume and force of contraction. Slow HR allows more time for ventricles to fill Regulation of HREffects on HR- autonomic nervous system, chemicals, hormones and ions Sympathetic nervous system increases heart rate Parasympathetic (vagus nerves) slow and steady the heart Epinephrine: increases heart rate Thyroxine: increases heart rate Heat: increases heart rate Average RHR: Female: 72-80 Male: 64-72 Congestive Heart Failure: Pumping efficiency of heart is depressed so htat circulation is inadequate to meet tissue needs. CHF: usually progressive condition that reflects weakening of the heart by coronary atherosclerosis, persistent high BP, multiple myocardial infarcts. Each side of the heart can fail independently Left side= Pulmonary congestion, causes pulmonary edema, person can suffocate and die. Right side= Peripheral congestion, causes edema in the distal parts of the body With either condition eventually the heart will fail without medical assistance.