Oral Histology and Embrylogy
advertisement

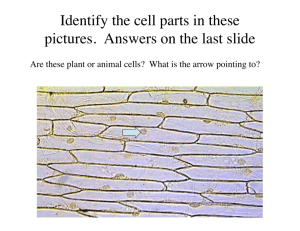
DH227 Board Review Oral Histology & Embryology LISA MAYO, RDH, BSDH CONCORDE CAREER COLLEGE General Embryology 23 chromosomes in each germ cell (haploid) 46 chromosomes after fertilization (diploid) Zygote: mitotic divisions 1. Morula 2. Blastocele 3. Blastocyst 3 periods of development 1. Period of ovum (1st week) 2. Embryonic Period (2-8 weeks): most congenital malformations occur 3. Fetal Period (3-9mo) Gen Embryology Facial & Oral structures dependent on grp of neural crest cells derived from ectoderm as neural tube develops Facial skeleton: Meckel’s cartilage Neck skeleton: hyoid bone Connective tissue components Tooth development Gen Embryology Neural crest cells migrate into each brachial arches and surrounds existing mesoderm 1. 2. 3. 4. Cartilage rod: 1st brachial arch Muscular component: 2nd, facial muscles Vasculature component Nerve component: 1st, trigeminal nerve Internal brachial arches – corresponding pharyngeal pouches that give rise to 1. 2. 3. 4. External auditory meatus Pharyngotympanic tube Palatine tonsils Parathyroid glands 5 Brachial Arches Five Pharyngeal (Branchial) arches develop below the oral pit Each pharyngeal arch is associated with a specific Cranial Nerve 1st Pharyngeal Arch: Mandibular 2nd Pharyngeal Arch: Hyoid 3rd, 4th, and 5th Pharyngeal Arches are located respectively below the other two arches and are separated down the middle by the pericardial cavity (heart). Developing Pharyngeal Arches 3½ Weeks Pharyngeal (Branchial) Arches The cores of these arches will differentiate into the blood vessels, muscles, nerves, cartilages, and bones that will form the human face Mandibular Arch: (1st Pharyngeal Arch) Gives rise to the Maxillary Process which forms the cheeks Eventually forms the: Mandible Muscles of Mastication Innervated by V Cranial Nerve (Trigeminal Nerve) Hyoid: 2nd Pharyngeal Arch) Forms the: Facial muscles Vessels Hyoid bone Innervated by the VII Cranial Nerve (Facial Nerve) 3rd and 4th Pharyngeal Arches Become the constrictor muscles of the throat Innervated by other Cranial Nerves of the muscles of the neck Question Which of the following tissues derive from ectoderm? a. b. c. d. Bone Nervous tissue Dentin and pulp Chewing muscles Answer Which of the following tissues derive from ectoderm? a. b. c. d. Bone Nervous tissue Dentin and pulp Chewing muscles NBQ The first brachial arch gives rise to the mandible, and it innervated by the trigeminal nerve a. b. c. d. Both statement are TRUE Both statements are FALSE The first statement is TRUE, the second statement is FALSE The first statement is FALSE, the second statement is TRUE NBQ The first brachial arch gives rise to the mandible, and it innervated by the trigeminal nerve a. b. c. d. Both statement are TRUE Both statements are FALSE The first statement is TRUE, the second statement is FALSE The first statement is FALSE, the second statement is TRUE NBQ With the exception of the ____, the oral and nasal cavities develop from the first brachial arch and the frontal process a. b. c. d. e. Lower lip Lower border of the cheeks Anterior portion of the hard palate Base of tongue Base of the nasal septum NBQ With the exception of the ____, the oral and nasal cavities develop from the first brachial arch and the frontal process a. b. c. d. e. Lower lip Lower border of the cheeks Anterior portion of the hard palate Base of tongue Base of the nasal septum Pharyngeal Grooves and Pharyngeal Pouches Development of Pharyngeal Arches Each arch is separated Internally by Pharyngeal pouches Externally by Branchial clefts/grooves Gill-like slits (pharyngeal arches) smooth to form Neck Disappearing “Gills” Tissues of the 2nd and 5th pharyngeal arches grow over the other arch grooves and make contact with each other Pharyngeal Grooves & Pharyngeal Pouches The 1st Pharyngeal Groove (covered by ectoderm) deepens to form the external auditory canal. The 1st Pharyngeal pouch forms into the middle ear and Eustachian tube. The membrane at the deepest part of this tube becomes the tympanic membrane. Pharyngeal Grooves & Pharyngeal Pouches 2’nd Pharyngeal Pouch Becomes Palatine Tonsils 3’rd Pharyngeal Pouch Becomes Parathyroid Glands Thymus 4’th Pharyngeal Pouch Becomes Ultimobranchial Body Prenatal Development Pre-implantation: 1-7 days Embryonic: 2-8 weeks Fetal: 9-38+ weeks Major developmental malformation occur in the embryonic period NBQ The olfactory (nasal) pits appear on the lateral sides of these a. b. c. d. e. Maxillary process Olfactory process Mandibular process Frontal process Globular process NBQ The olfactory (nasal) pits appear on the lateral sides of these a. b. c. d. e. Maxillary process Olfactory process Mandibular process Frontal process Globular process Prenatal Development 3 primitive tissue precursors form 1. Ectoderm: Form outer covering of body. Lining of oral cavity. epithelium, salivary glands, nervous system, ameloblasts (enamel) 2. Endoderm: Epithelial linings of internal organs: GI tract, resp system, urinary tract 3. Mesoderm: connective tissues of skeletal, vascular, muscle, dermis, dental pulp, periodontal attachment, cementum, dentin Derivatives of Ectoderm, Mesoderm, and Endoderm layers Ectoderm The embryo is covered by a single layer of ectodermal cells which differentiate into multiple layers Epidermal and dermal cells develop and differentiate into hair, teeth, nails and mammary, sebaceous, and salivary glands Mesoderm Medial somites in the mesoderm form the skeleton that will surround the neural tube. Intermediate mesoderm forms the striated/voluntary muscle of the body. Lateral mesoderm forms the dermis of the epithelium of the body and the GI tract. All peristaltic musculature is derived from mesoderm. Endoderm The endoderm forms into the gastrointestinal tract, which elongates and develops “outpouchings” that form the pharyngeal pouches, lung buds, liver, gall bladder, pancreas, and urinary bladder. Ectoderm forms Neural Crest Neural crest cells form the sensory system of the dorsal root ganglia of the cranial and spinal nerves Neural Tube Development: Week 3 - 9 Closing of Neural Tube (3rd week of development) Head and Neck Development Folding of the embryo at 3-4 weeks forms a space (stomodeum) limited by a temporary barrier (oropharyngeal membrane). It will become the oral cavity Pouches form called brachial arches FIRST MANDIBULAR ARCH: forms mandible, muscles of mastication, nerve and blood supplies, Merkel’s cartilage which is the precursor of the mandible SECOND ARCH (HYOID): forms facial muscles and vessels, hyoid bone Head & Neck Development Face forms week 4-7 w/ formation of stomodeum Tooth enamel forms from ectoderm lining the stomodeum Upper Lip: complete within 6-8 weeks: Fusion of the median nasal process and RT/LF maxillary processes Palate forms week 5-12 Failure of components to fuse during these periods results in cleft lip, palate or both. Unilateral or bilateral Fusion of globular process with the LF/RT palatal shelves Separates the stomodeum into an upper (nasal) and lower (oral) cavity Tongue forms weeks 4-8 Body from tuberculum impar and lateral tissues, and base from copula form and fuse at the sulcus terminalis Post 1/3 and hyoid bone develops from the 2nd and 3rd brachial arches Know the nerve and blood supplies for the tongue, other oral soft tissues, facial skeleton, teeth NBQ The buccopharyngeal membrane at what week in development? a. b. c. d. 2 weeks 3 weeks 4 weeks 6 weeks NBQ The buccopharyngeal membrane at what week in development? a. b. c. d. 2 weeks 3 weeks 4 weeks 6 weeks NBQ A cleft lip occurs when maxillary process fails to fuse with the a. b. c. d. e. Palatine process Globular process Lateral nasal process Mandibular process Opposing maxillary process NBQ A cleft lip occurs when maxillary process fails to fuse with the a. b. c. d. e. Palatine process Globular process Lateral nasal process Mandibular process Opposing maxillary process NBQ Palatal closure occurs during which week in embryonic development? a. b. c. d. 2 4 8-12 16 NBQ Palatal closure occurs during which week in embryonic development? a. b. c. d. 2 4 8-12 16 Head & Neck Most structures of oral cavity develop from 2 embryonic processes Frontal process Forehead, frontal bone Median nasal process: center and tip nose, nasal septum, globular process (philtrum, premaxillary palate) Lateral nasal process: sides of nose, infraorbital area 1st brachial arch Maxillary process: lateral palatine processes (palatal shelves), upper parts of cheek, sides of upper lip Mand process: lower jaw, lower parts of the face and lower lip, ant 2/3 of tongue Salivary Glands Major and minor, serous and mucous components, major from 1st brachial arch PAROTID: Stenson’s duct, serous saliva, most common site for tumors SUBMANDIBULAR: Wharton’s duct, serous mucous SUBLINGUAL: anterior floor of mouth, mucous, several ducts along sublingual folds Question The embryological origin of the face is largely from the a. b. c. d. Second brachial arch Second and third brachial arches Frontal process and first brachial arch Frontal process and second brachial arch Answer The embryological origin of the face is largely from the a. b. c. d. Second brachial arch Second and third brachial arches Frontal process and first brachial arch Frontal process and second brachial arch Tongue Development Pharyngeal Arches: 1st forms the anterior (moveable) 2nd , 3rd forms the immovable base The tongue is innervated by the V, VII, IX, X, and XII Cranial nerves for various functions. Tissues of the Tongue 3 Parts: Tuberculum impar (central) Both lateral lingual swellings (sides) As they grow, a U-shaped sulcus forms around the anterior of the tongue to separate it from the jaw tissues This allows free movement of the anterior tongue The 3 parts fuse completely to form the tongue body Tongue formation: 1st Pharyngeal Arch Tongue Development The body and the base of the tongue are separated by the terminal sulcus Behind the terminal sulcus the lingual tonsil develops from the base on the dorsal side Waldeyer’s Ring: (ring of tonsils in pharynx) Lingual tonsil Palatine tonsils Pharyngeal tonsils Body and Base of the Tongue Lateral lingual swellings and tuberculum impar have completely merged and fused to form the body and base of the tongue. Question What is the origin of “Rests of Malassez”? Junctional epithelium Reduced enamel epithelium Hertwig’s epithelial root sheath Cementoblasts in the PDL Answer What is the origin of “Rests of Malassez”? Junctional epithelium Reduced enamel epithelium Hertwig’s epithelial root sheath Cementoblasts in the PDL Question Rests of Malassez are composed of Calcified PDL Calcifications n the dental pulp Groups of epithelial cells attached t the enamel Groups of epithelial cells in the PDL Answer Rests of Malassez are composed of Calcified PDL Calcifications n the dental pulp Groups of epithelial cells attached t the enamel Groups of epithelial cells in the PDL Question Which structure marks the embryonic origin of the thyroid gland? a. b. c. d. Tonsillar pillar Stenson’s duct Foramen ovale Foramen cecum Answer Which structure marks the embryonic origin of the thyroid gland? a. b. c. d. Tonsillar pillar Stenson’s duct Foramen ovale Foramen cecum NBQ What anatomic feature separates the root and the body of the tongue? a. b. c. d. e. The lingual frenum The fungifofrm papillae The median groove The third brachial arch The circumvallate papillae NBQ What anatomic feature separates the root and the body of the tongue? a. b. c. d. e. The lingual frenum The fungifofrm papillae The median groove The third brachial arch The circumvallate papillae NBQ Remnants of Hertwig’s epithelial root sheath sound in the PDL of a functional tooth are called: a. b. c. d. e. Enamel pearls Denticles Rests of Malassez Cementicles Intermediate plexus NBQ Remnants of Hertwig’s epithelial root sheath sound in the PDL of a functional tooth are called: a. b. c. d. e. Enamel pearls Denticles Rests of Malassez Cementicles Intermediate plexus HISTOLOGY Histology Cells parts reviewed during A&P lecture Tissues Epithelium Connective Tissue Muscle Nervous Tissue Histology: Epithelium Tissues Simple and stratified (layered) Named by cell shape Avascular Basement membrane separates from underlying connective tissue Review locations of different types Stratified squamous epithelium lines oral cavity Histology: Connective Tissues Collagen fibers Loose and dense Calcified and non-calcified Cartilage: hyaline remodels into bone Elastic is flexible Fibrous lines boney surfaces Bone: form skeletal system Blasts: build Clasts: consume Cytes: just hang around different hard CT Histology: Muscle Tissues Skeletal (voluntary) Smooth(GI and blood vessels) Cardiac (heart muscle) Histology: Nervous Tissues Ectodermal origin Central: brain and spinal cord Peripheral components Afferent (sensory) signals to CNS Efferent (motor) signals from CNS to muscle and glands Somatic system carries signals to voluntary muscles Autonomic system carries signals from CNS to involuntary muscles and glands Sympathetic: causes activity, fight-or-flight Parasympathetic: maintain status quo, decrease activity Tooth Development Begins 7th weeks of embryonic life with 20 primary teeth Continue development until late teens Enamel forms from ectoderm lining the sotmoduem Dentin/pulp form from ectomesenchyme (derived from embryonic ectoderm adjacent to the underlying mesenchymal tissue Each tooth is product of 2 tissues 1. 2. Mesenchymal: derived from neural crest cells Epithelium: oral epithelium derived from ectoderm NBQ What type of primitive tissue gives rise to the enamel of a tooth? a. b. c. d. Ectoderm Mesoderm Endoderm None of the above NBQ What type of primitive tissue gives rise to the enamel of a tooth? a. b. c. d. Ectoderm Mesoderm Endoderm None of the above NBQ The embryonic origin of all connective tissue is d. Mesenchyme Endoderm Fascia Ectoderm e. Epithelium a. b. c. NBQ The embryonic origin of all connective tissue is d. Mesenchyme Endoderm Fascia Ectoderm e. Epithelium a. b. c. NBQ Rathke’s pouch if the embryonic origin of the a. b. c. d. e. Thyroid gland Palate Globular process Pituitary gland Nasal septum NBQ Rathke’s pouch if the embryonic origin of the a. b. c. d. e. Thyroid gland Palate Globular process Pituitary gland Nasal septum Tooth Development: 2 Events Morphodifferentiation Shaping of teeth Stages: Bud, Cap, Bell, Apposition Cytodifferentiation Epithelial Outer Inner Stratum Stellate reticulum Mesenchymal Dental sac: alveolar bone, PDL, Cementum Dental papilla: odontoblasts Pulp Tooth Development Initiation (Bud) stage 1. Dental lamina (ectodermal thickening) grows into the underlying mesenchymal (conncective) tissue at 20 places to form the primary teetj 2. Proliferation (Cap) Stage Enamel organ develops from the dental lamina, and will produce enamel Dental papilla arises and produces pulp/dentin The dental sac surrounds the developing tooth, and becomes cementum, the PDL and alveolar bone Tooth Development 3. Differentiation (Bell) Stage Enamel 1) 2) 3) 4) organ develops 4 distinct layers Outer enamel epithelium Stellate reticulum Stratum intermedium Inner enamel epithelium: becomes enamel. IEE becomes amelobasts which produce enamel, odontoblasts from the dental papillae produce dentin Tooth Development Tooth structure is produced layer by layer (appositional growth) Tooth matrix is initially soft, then mineralizes (hydroxyapatite is crystalized calcium phosphate) Root formation begins after the crown if complete, and ends 14yrs after eruption Enamel organ layers condense to form the reduced enamel epithelium Hertwig’s epithelial root sheath (HERS), which develops from the internal and external enamel epithelium, helps determine outline of the root and dissolves Remnants of HERS (knows as rests of Malassez) have the potential to form cysts Remnants of the dental lamina are known as Rests of Serres Teeth: Enamel 96% mineralized (hydroxyapatite) Composed of enamel rods perpendicular to surface Ectodermal origin from inner enamel epithelium Secreted by ameloblasts after dentin formation begins Inner and outer enamel epithelial areas combine to form the Reduced Enamel Epithelium as enamel formation is completed Hertwig’s root sheath forms REE combines with surface epithelium at eruption and cervical area becomes junctional epithelium Ameloblasts have disappeared as formative cells appear Teeth: Dentin 70% mineralized Composed of dentinal tubules extending from DEJ to pulp chamber Mesodermal origin and formed by odontoblasts (precedes enamel formation initially) Odontoblasts remain viable and capable of forming dentin after tooth formation is completed Primary dentition forms before completion of the root apex Secondary dentin forms after apex is completed Tertiary (reparative) dentin forms in response to injury or some irritations Teeth: Dentin Peritubular dentin forms tubule walls Intertubular dentin forms between tubules Outerdentinal layer nearest DEJ formed 1st and is called mantle dentin Cicrumpulpal dentin forms inner dentinal layer nearest pulp chamber Tubules narrow with age NBQ The layer of dentin found adjacent to the pulp in young teeth is called a. b. c. d. e. Tome’s granular layer Predentin Interglobular dentin Dead tracts Sclerotic dentin NBQ The layer of dentin found adjacent to the pulp in young teeth is called a. b. c. d. e. Tome’s granular layer Predentin Interglobular dentin Dead tracts Sclerotic dentin The last visible layer in Nonkeratinized stratified squamous epithelium is the a. b. c. d. Basal cell layer Prickle cell layer Granular layer Corneum layer The last visible layer in Nonkeratinized stratified squamous epithelium is the a. b. c. d. Basal cell layer Prickle cell layer Granular layer Corneum layer NBQ Dentin is the product of a. b. c. d. e. Dental lamina Dental organ Dental papilla Dental cuticle Dental sac NBQ Dentin is the product of a. b. c. d. e. Dental lamina Dental organ Dental papilla Dental cuticle Dental sac Teeth: Cementum Cementicles Calcified ovoid or round nodule found in the PDL May be found in grps or near the surface of the cementum More prevalent along the root in an aging person May be found at the site of trauma Teeth: Cementum Mature Cementum: 3 grps fibers 1. 2. 3. Grp I: collagen fibers produced by cementoblasts, parallel to long axis of root Grp II: fibers from cells of dental sac, form fibers PDL Grp III (external): coarser than internal, Sharpey’s fibers Teeth: Pulp Vascular tissue within pulp chamber Contains connective tissue, nerves, blood vessels, odontoblasts at periphery Nerves only respond with pain to stimulation Derived from dental papilla Pulp & Dentin Comparisons Closely related developmentally and functionally Pulp = loose, non-calcified ct, vascular Dentin=calcified ct, avascular Development Odontobasts = form dentin Dental papilla = form pulp Bone: Alveolar Formed during development & eruption of teeth Located in boney crypts of jaw bone Same histology as other bones in body Anatomy Each tooth in own alveolus (socket), inner cortical plate, spongiosa Each socket has 3 parts: Outer cortical plate Alveolar bone proper: part of bone facing root of tooth, follows outline of roots, sometimes called cribiform plate/lamina dura Question The cells that produce enamel derive from the a. b. c. d. Stellate recticulum Junctional epithelium Inner enamel epithelium Outer enamel epithelium Answer The cells that produce enamel derive from the a. b. c. d. Stellate recticulum Junctional epithelium Inner enamel epithelium Outer enamel epithelium Question Which of the following is a likely reaction to destruction of a focal area of odontoblasts by injury? a. b. c. d. New odontoblasts will differentiate from epithelial rests of Malassez New odontoblasts will form by division of vital odontoblasts adjacent to the zone of injury New odontoblasts will form by differentiation from cells in the cell rich layer of the pulp None of the above Answer Which of the following is a likely reaction to destruction of a focal area of odontoblasts by injury? a. b. c. d. New odontoblasts will differentiate from epithelial rests of Malassez New odontoblasts will form by division of vital odontoblasts adjacent to the zone of injury New odontoblasts will form by differentiation from cells in the cell rich layer of the pulp None of the above PDL Specialized form of ct Derived from dental sac Made of fiber bundles 1. 2. Gingival: dentogingival, dentoperiosteal, transeptal, circumfrential Principal: alveolar crest, horizontal, oblique, apical, interradicular Fast turnover rate Fibrous Matrix Fibers are collagen & oxytalan with few elastic fibers assoc with blood vessels Sharepy’s Fibers: terminal portion of PDL that is embedded in bone PDL Rich blood supply 2 types nerves 1. 2. Autonomic Afferent sensory 2 types nerve endings 1. 2. Free, un-myelinated Encapsulated Width varies Wider in younger adults than older Greater near cervical/apical areas Greatest movements occur apical/cervical Related to amt of function Oral Mucosa Composed of stratified squamous epithelial layer and a ct lamina propria, separated by a basement membrane It includes the masticatory, lining, and specialized mucosal tissues Masticatory mucosal tissue is keratinized and protects the gingiva and hard palate. The keratinization of the attached gingiva ends at the free gingival margin Lining mucosa is not keratinized and includes the alveolar, vestibular and buccal mucosa, floor of the mouth Specialized mucosa refers to the papillae of the tongue NBQ In the oral cavity, one way in which lining mucosa differs from masticatory mucosa is that c. Lining mucosa contains more muscle fibers Masticatory mucosa contains glands Lining mucosa has no submucosa d. Lining mucosa is not keratinized a. b. NBQ In the oral cavity, one way in which lining mucosa differs from masticatory mucosa is that c. Lining mucosa contains more muscle fibers Masticatory mucosa contains glands Lining mucosa has no submucosa d. Lining mucosa is not keratinized a. b. Anatomy of Gingiva Stratified squamous epithelium with a basement membrane between the epithelium and connective tissue Stratum corneum outside layer Keratinized=no nuclei, tough Attached Gingiva Non-Keratinized=have nuclei, more flexible, lining mucosa Sulcular & Junctional Epithelium Anatomy of Gingiva No blood vessels Nutrients from connective tissue vasculature Desmosomes connect epithelial cells to each other Hemidesmosomes connect epithelial cells to connective tissue Gingival Fibers: 9 groups based on orientation, insertions, structures, involved Gingival connective tissue Lots collagen matrix Few cells: fibroblasts, macrophages, lymphocytes, neutrophils 3 Gingival Epithelium Areas Oral Epithelium Outer surface of free and attached gingiva from gingival margin to mucogingival junction Keratinized or partially keratinized Orthokeratinized= thicker granular layer Rete pegs connect to connective tissue inside 2. Sulcular Epithelium Lining of gingival sulcus Nonkeratinized=allows for crevicular fluid in and out No Rete pegs, just smooth interface 1. 3 Gingival Epithelium Areas 3. Junctional Epithelium Seals and protects Forms base of sulcus and attaches to tooth surface 0.75-1.35mm long Nonkeratinized Attached by hemidesmosomes to enamel or an implant surface in health, dentin or cementum in disease Oral Epithelium Melanocytes Langerhans cells Merkle cells Inflammatory cells Stratified squamous (3 types) 1. Orthokeratinized a. b. 2. Nonkeratinized a. 3. Less common Cell layers: Basal (deepest), Prickle, Granular, Keratinized outer layer Cell layers: Basal, prickle, nonker. outer layer Parakeratinized: between #1&2 a. Cell layers: Basal, prickle, keratinized outer layers Oral Epithelium Connective Tissues: Lamina Propria Layers: Papillary & Reticular Submucosa: between lamina propria & muscles Interface Area between oral epithelium & ct Rete Pegs: epithelial extension into lamina propria Basement Membrane 2 layers: Basal lamina (densa) & Reticular lamina (lucida) Epithelial cells for hemidesmosome attachments to basal lamina Question Where are Von Ebner’s glands located? In submucosa of the pharynx In the submucosa of the cheek Beneath the floor of the mouth Beneath circumvallate papillae in the tongue Answer Where are Von Ebner’s glands located? In submucosa of the pharynx In the submucosa of the cheek Beneath the floor of the mouth Beneath circumvallate papillae in the tongue Question During which time of fetal development will cleft palate form? a. b. c. d. Second trimester Week 1-3 Weeks 6-11 Early in the 3rd trimester Answer During which time of fetal development will cleft palate form? a. b. c. d. Second trimester Week 1-3 Weeks 6-11 Early in the 3rd trimester