Urinary System- Anatomy and Physiology
advertisement
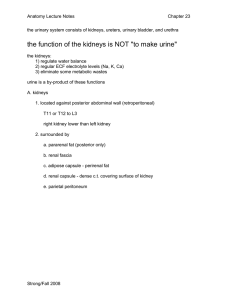
Urinary SystemAnatomy and Physiology Zoe McCarthy 1 Urinary System in Context 2 Urinary System in Context System How does it do it? 3 Functions of the Urinary system • 1. Regulating blood volume and pressure • 2. Regulating plasma concentrations of sodium, potassium, chloride and other ions • 3. Stabilising blood pH • 4. Conserving nutrients • 5. Detoxifying poisons (with the liver) 4 Organisation of the Urinary System • • • • Kidneys Ureters Urinary bladder Urethra 5 Position of the Kidneys CT abdomen with contrast MRI coronal abdomen 6 Protection of the Kidneys • 3 layers of connective tissue: Renal cortex – Inner layer- Renal capsule – Middle layer- Adipose capsule – Outer layer-Renal fascia Retroperitoneal space 7 Surface anatomy of the Kidney • Hilum is located on the medial surface 10 cm 3cm 5.5cm 8 Internal Structure of the Kidney Renal Lobe Renal pyramids Renal papilla Renal Columns 9 Microscopic structure of the Kidney and Urine Production 10 Renal Corpuscle and Filtration 11 Nephron-Tubular System 1. Proximal convoluted tubule 2. Descending loop of Henle 3. Ascending loop of Henle 4. Distal convoluted tubule 5. Collecting duct 12 Summary so far….. Blood enters the kidney through the renal artery at the site of the hilum The PCT is concerned with reabsorption- organic nutrients are reabsorbed and water follows because there is a concentration gradient The remaining filtrate moves into the descending loop of henle. This is lined with thin cells so water moves out A number of other nephrons join up to the cleectig duct which travels through the medulla to the renal papilla wher the filtrate is emptied in the minor calyx 4-5 minor calyces join up to make a major calyx The renal artery divides in to ever smaller arteries and arterioles The filtered substances move into the proximal convoluted tubule Because water has been reabsorbed the concentration of the filtrate is not very high From the DCT the filtrate now passes into the collecting duct. 2-3 major calyces join up to form the renal pelvis Afferent arterioles take blood to the glomerulus to be filtered Once blood is filtered efferent arterioles take blood away from the glomerulus Products which are filtered out: water, mineral salts, amino acids, glucose, hormones, urea, toxins The glomerulus is a network of capillaries which filters the blood The walls of the ascending loop of henle are lined with thicker cells, so water can’t pass in or out. Instead sodium and chloride is pumped out actively In the DCT the volume and composition of the filtrate can be adjusted but this is controlled by hormones The renal pelvis joins the ureter at the hilum Products which do not filter and remain in the blood: Leukocytes, erythrocytes, platelets, plasma proteins The filtrate now enters the distal convoluted tubule- is it now only 20% of what it originally was. The ureter transport the filtrate/urine from the kidney to the bladder 13 The Formation of Urine • 3 processes involved in the formation of urine. – Simple filtration – Selective reabsorbtion • Hormonal control» Parathyroid hormone, calcitonin » Anti diuretic hormone » Aldosterone – Secretion 14 Ureters • Superiorly • Continuous with the renal pelvis • Inferiorly • Pass through the abdominal cavity, behind the peritoneum, infront of the psoas muscle, into the pelvic cavity ehere they enter the posterior wall of the bladder • 25-30 cm in length 15 Ureter- Cross Section • 3 layers of tissue – Outer layer • Fibrous tissue – Middle layer • Muscle – Inner layer • Epithelium 16 Bladder 17 Bladder- structure of • 3 layers – Outer layer • Loose connective tissue – Middle layer • Smooth muscle and elastic fibres – Inner layer • Lined with transitional epithelium 18 Urethra • Extends from the base of the bladder to the outside world. • Anatomical differences mean that male and female urethras are different. – Female: long – Male: long 4cm 14cm 19 Urethra- structure of • Muscle layer • Submucosa layer • Mucosa 20