Anatomy Lecture Notes Chapter 23
advertisement

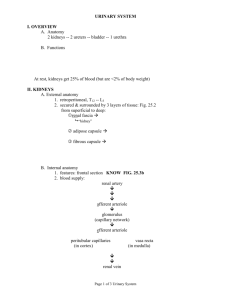
Anatomy Lecture Notes Chapter 23 the urinary system consists of kidneys, ureters, urinary bladder, and urethra the function of the kidneys is NOT "to make urine" the kidneys: 1) regulate water balance 2) regular ECF electrolyte levels (Na, K, Ca) 3) eliminate some metabolic wastes urine is a by-product of these functions A. kidneys 1. located against posterior abdominal wall (retroperitoneal) T11 or T12 to L3 right kidney lower than left kidney 2. surrounded by a. pararenal fat (posterior only) b. renal fascia c. adipose capsule - perirenal fat d. renal capsule - dense c.t. covering surface of kidney e. parietal peritoneum Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 3. layers a. cortex - contains renal corpuscles and extends inwards as renal columns b. medulla - consists of renal pyramids which consist mostly of collecting ducts papilla - apex of renal pyramid; where collecting ducts drain into calyx 4. cavities and associated structures a. renal sinus - space in medial part of kidney; contains renal pelvis b. renal pelvis - expanded superior part of ureter minor calyx collects urine from one renal papilla major calyx formed by junction of 2 or more minor calyces renal pelvis formed by junction of all major calyces Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 5. renal hilum - medial indentation; where ureter leaves kidney 6. blood flow through the kidney - renal fraction = 20% of cardiac output aorta renal artery segmental arteries lobar arteries interlobar arteries arcuate arteries cortical radiate (interlobular) arteries afferent arterioles glomerular capillaries (glomerulus) efferent arteriole peritubular capillaries and vasa recta cortical radiate (interlobular) veins arcuate veins interlobar veins renal vein inferior vena cava Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 7. histology: uriniferous tubule = structural and functional unit of kidney > 1 million per kidney components = nephron + collecting duct nephron = renal corpuscle + 3 tubular sections renal corpuscle = glomerular capsule + glomerular capillaries a. glomerular (Bowman's) capsule parietal layer - simple squamous e. visceral layer - podocytes (branching epithelial cells) pedicels filtration slits function = makes filtrate b. proximal convoluted tubule (PCT) epithelium is modified to have a large surface area: simple cuboidal e. with microvilli folded basal surface function: reabsorbs molecules from filtrate c. loop of the nephron (loop of Henle) descending limb vs ascending limb thick segment (simple cuboidal e.) vs thin segment (simple squamous e.) categories of nephrons: cortical nephrons (85%) - loop barely dips into medulla juxtamedullary nephrons (15%) loop extends deep into medulla; conserve water Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 d. distal convoluted tubule (DCT) epithelium - simple cuboidal e. with sparse microvilli and folded basal surface function: reabsorbs molecules from filtrate and secretes molecules into filtrate e. collecting ducts (also called collecting tubules) receive DCT of several nephrons extend from cortex down into medulla form renal pyramids terminate at renal papilla and empty into calyx made of simple cuboidal e. functions: conserve water by reabsorbing it from the filtrate carry urine to renal calyces review of components: glomerular capsule proximal convoluted tubule loop of the nephron distal convoluted tubules collecting duct Strong/Fall 2008 glomerulus Anatomy Lecture Notes Chapter 23 review of function: afferent arteriole glomerular capsule glomerulus efferent arteriole proximal convoluted tubule peritubular capillaries loop of the nephron vasa recta distal convoluted tubules peritubular capillaries collecting duct veins renal calyx 8. juxtaglomerular (jg) apparatus a. jg cells of afferent arteriole modified smooth muscle cells mechanoreceptors that monitor blood pressure secrete renin when blood pressure is low b. macula densa cells of DCT modified epithelial cells chemoreceptors that monitor filtrate composition signal JG cells when filtrate solute concentration is low c. overall effect: increase blood pressure when renal pressure is too low Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 9. the filtration membrane has three layers: a. capillary endothelium fenestra have no membranes (diaphragm) b. basement membrane c. podocytes filtration slits covered by diaphragm functions: it permits the free passage of small molecules it filters plasma as it passes through the kidney the filtrate collects in the glomerular capsule B. ureters begin as a continuation of the renal pelvis medially out of kidney run retroperitoneally towards the urinary bladder join the urinary bladder at its posterolateral corners angle prevents backflow structure: mucosa - transitional e. muscularis - two layers of smooth m.; peristalsis propels urine adventitia - c.t. C. urinary bladder 1. location: posterior to pubic symphysis anterior to: vagina and uterus in females rectum in males 2. the opening into the urethra is located anterior to the openings of the ureters trigone = triangular area formed by openings of ureters and urethra 3. structure: a. mucosa - transitional e. b. muscularis (called detrusor m.) - 3 layers of smooth m. c. adventitia (c.t.) and serosa (visceral peritoneum) Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 4. function - stores urine at about 300 mL, stretch receptors initiate micturition reflex and notify cerebrum can hold 500 mL to 1 L 5. urethral sphincters a. internal = smooth m. surrounding opening to urethra; involuntary b. external = skeletal m. surrounding urethra below urinary bladder; voluntary D. urethra function: drains urine from urinary bladder structure: mucosa - transitional e. near urinary bladder changes to stratified squamous e. near orifice muscularis adventitia in females 3 to 4 cm long bound to anterior wall of vagina orifice located anterior to vaginal opening in males prostatic urethra inside prostate gland just inferior to urinary bladder membranous urethra inside urogenital diaphragm spongy/penile urethra inside corpus spongiosum of penis orifice at end of penis shared by urinary and reproductive systems Strong/Fall 2008