SKELETAL MUSCLE RELAXANTS, SPASMOLYTICS AND LOCAL

Skeletal Muscle Relaxants
Dr. Rene Anand
Reference: Bertram Katzung et al,
"Basic and Clinical Pharmacology",
12th edition, McGraw-Hill Lange, Chapter 27
1
Learning Objectives
Describe the pharmacological properties of drugs classified as relaxants
Describe the transmission process at the skeletal neuromuscular end plate and the points at which drugs modify this process
Identify the major non-depolarizing neuromuscular blockers and one depolarizing neuromuscular blocker, compare their pharmacokinetics
Describe the differences between depolarizing and non-depolarizing blockers from the standpoint of tetanic and post-tetanic twitch strength
Describe the reversal of non-depolarizing blockade
List drugs for treatment of skeletal muscle spasticity and identify their sites of action and adverse effects
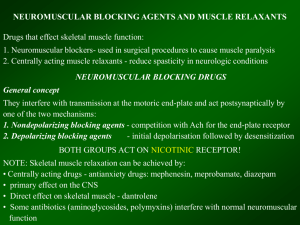
Skeletal Muscle Relaxants
Skeletal muscle relaxants interfere with the contraction of skeletal muscles:
1.
2.
Neuromuscular blockers are used to completely paralyze skeletal muscle during surgical and orthopedic procedures in the controlled environment of a hospital.
Spasmolytics are used to elicit a more modulatory effect on muscle contraction and do not completely block the activity of the skeletal musculature. These agents are used to reduce muscle spasms and are commonly used in ambulatory patients.
3
Classification of Skeletal Muscle Relaxants
Peripherally acting drugs
Neuromuscular blocking drugs.
Direct acting spasmolytic.
Centrally acting spasmolytics.
4
I Summary of Neuromuscular Transmission
An action potential depolarizes the nerve terminal and Ca2+ enters. AChcontaining vesicles fuse with the prejunctional membrane releasing the ACh by exocytosis into the junctional space.
The released ACh diffuses across the synaptic gap and binds to nicotinic (Nm) receptors leading to depolarization of the muscle end-plate region. The nicotinic receptor is a complex of 5 protein subunits. There are 2 a subunits, and one each of b, g and d subunits in embryonic muscle. In the adult d is replaced by an e subunit.
When one molecule of ACh binds to each of the a subunits there is an increase of the fluxes of Na+ in, Ca2+ in, and
K+ out.
5
II Summary of Neuromuscular Transmission
There is propagation of a muscle action potential through the conducting system of the myofibrils, with release of Ca 2+ from the sarcoplasmic reticulum. This triggers off the troponinactin-myosin interaction and muscle contraction.
Relaxation is associated with restorage of Ca 2+ in the sarcoplasmic reticulum which is driven by energy supplied by an ATPase. There is a refractory period until repolarization of the muscle end-plate.
ACh is inactivated by ACh esterase (AChE).
6
Quick Review: Model of Nicotinic
Receptor
Quick Review
7
Quick Review
Quick Review
Curare
Curare is a generic term that refers to a mixture of naturally occurring alkaloids found in various South American plants and is used to make arrow poison by some South American
Indians. The most important alkaloid is dtubocurarine. First used in surgery in 1942.
http://waynesword.palomar.edu/ecoph23.htm
9
Peripherally acting drugs
Neuromuscular Blocking Drugs
Chemically most are bisquaternary ammonium compounds
Interaction with the acetylcholine (ACh) receptor appears to be one to one but the exact nature is unknown. It is speculated that the charged compounds span and bind to the nicotinic
(Nm) receptor and prevent ACh from reaching it.
-N +______________ N + -
+
Pancuronium
Characteristics of quaternary compounds considering their positive charge
Poorly absorbed from the gut and generally rapidly excreted
Administered
IV
Will not cross the blood-brain barrier
Will not cross the placenta
11
Indications for Neuromuscular Blocking
Drugs
Adjunct for surgery to reduce muscle tone and fasciculation at the site of surgery
(permit tracheal intubation).
Electroshock therapy for psychiatric disorders (prevent bone breakage).
Control convulsive disorders (status epilepticus, tetanus, eclampsia and toxic reactions to local anesthetics).
Control respiration when the patient is unable to ventilate.
12
Classification of Neuromuscular Blocking
Drugs
Nondepolarizing Blocking
Drugs (competitive, stabilizing, or antidepolarizing drugs).
Depolarizing Blocking
Drugs.
13
1. Nondepolarizing Blocking Drugs
Block neuromuscular junction nicotinic receptors competitively.
They compete for the receptor with
ACh.
14
I Classification of some neuromuscular blocking agents based on duration of action
Drug Effect on Autonomic
Ganglia
Effect on Histamine
Release
Effect on Cardiac
Muscarinic Receptors
Nondepolarizing Drugs
Long-acting (>35 min)
Pancuronium
Intermediate-Acting
(20-35 Min)
Vecuronium
Atracurium
Rocuronium
Cisatracuium
None
None
None
None
None
None
None
Slight
None
None
Moderate Blockade
None
None
None
None
(-ium)
15
Nondepolarizing Blocking Drugs
Because they are competitive blockers their action can be reversed by increasing the concentration of endogenous ACh at the NMJ.
Use ChE inhibitors such as neostigmine, physostigmine, edrophonium together with atropine to protect muscarinic receptors against excessive stimulation by increased levels of
ACh.
16
II Classification of some neuromuscular blocking agents based on duration of action
Drug Effect on
Autonomic
Ganglia
Effect on
Histamine
Release
Effect on
Cardiac
Muscarinic
Receptors
Depolarizing
Drugs
Short-Acting (5-15 min)
Succinylcholine
Stimulation Slight Stimulation
Succinylcholine (Anectine®) structurally looks like two molecules of ACh end-toend. It is a relatively short duration (5-15 min) ACh-like agonist at nicotinic receptors.
17
Progression of pharmacological response to succinylcholine
18
Metabolism of succinylcholine
ACh
+
(CH
3
)
3
-N-CH
2
-CH
2
-O-OC-CH
3
Succinylcholine
+
(CH
3
)
3
-N-CH
2
-CH
2
-O-OC-CH
2
-CH
2
-CO-O-CH
2
+
-CH
2
-N-(CH
3
)
3 plasma ChE succinylmonocholine 1/2 activity plasma ChE succinic acid + choline
Note . ACh metabolism takes place primarily in the NMJ, while succinylcholine metabolism takes place in the plasma
19
Plasma ChE
20
I Adverse Effects of neuromuscular blocking drugs
21
II Adverse Effects of neuromuscular blocking drugs
Nondepolarizing Drugs
• Atracurium (occasionally succinylcholine)
Release of endogenous histamine into the circulation- bronchospasm, increased excretions, vasodilation resulting in decreased blood pressure.
• Treatment - antihistamines
Pharmacological response Potentiated by:
Some general anesthetics (methoxyflurane) and local anesthetics.
Antibiotics (aminoglycosides; neomycin and streptomycin have a tendency to inhibit
Ca2+ fluxes).
Fluid and electrolyte imbalance.
22
Direct-Acting (myotropic) Spasmolytics
Dantroline
• Interferes with release of Ca2+ from the sarcoplasmic reticulum which is required for muscle contraction.
Indications
• Chronic disorders characterized by muscle spasms.
• Spinal cord injury
• Stroke
• Cerebral palsy
• Multiple sclerosis
• ( Potential toxicity: Hepatotoxicity)
Malignant Hyperthermia: Genetic disorder, autosomal dominant. Triggered by halogenated anesthetic and/or succinylcholine. Sudden rise of Ca2+ in muscle fiber with increase of body temperature, rigidity.- 50% mortality.
23
I Centrally Acting Spasmolytics Antispastic action
Exerted mainly on the spinal cord by inhibiting mono- and poly-synaptic activation of motor neurons.
Baclofen. GABAB receptor agonist. Activates GABAB receptors on nerve endings that release excitatory neurotransmitters and prevents the release of the excitatory neurotransmitters (glutamate) onto motor neurons.
Diazepam. Belongs to the benzodiazepine class of drugs.
Enhances the actions of the inhibitor neurotransmitter GABA in the spinal cord.
Indications: Chronic disorders characterized by muscle spasticity.
• spinal cord injury
• stroke
• cerebral palsy
• multiple sclerosis
Side effects: Sedation and drowsiness
24
II Centrally Acting Spasmolytics
Tizanidine.
• Mechanism of action is unclear.
• Derivative of clonidine and has significant α2- adrenoceptive agonist activity.
• Appears to reinforce pre- and postsynaptic inhibition in the cord.
• Also inhibits nociceptive transmission in the cord.
Indications:
• Chronic disorders characterized by muscle spasticity.
Side effects: Sedation, drowsiness, hypotension, dry mouth, and asthenia.
25
I Drugs used for acute local muscle spasm
There are a large number of sedative drugs that are promoted for the relief of acute temporary muscle spasm caused by local trauma or strain.
Side effects: Most are sedative hypnotics and some have antimuscarininc activity.
The drugs include:
• Carisoprodol
• Chlorzoxazone
• Cyclobenzaprine
• Metaxalone
• Orphenadrine
26
II Drugs used for acute local muscle spasm
Botulinum Toxin
• Inhibits the release of
ACh from cholinergic nerve terminals.
• Local injection is finding increasing use in the treatment of spastic disorders due to neurologic injury.
• Benefits may persist for weeks after a single injection.
Potential toxicity
• May spread beyond injection site and lead to difficulty swallowing and breathing.
27
Botulinum Toxin (Types A-G).
Botulinum Toxin
(Types A-G).
The heavy chain is similar for all types, the light chains differ.
Botox approved to treat:
Strabismus (Crosseyes)
Unintended consequence:
Appears to be effective for the treatment of some forms of headache
Uncontrollable blinking
Moderate to severe frown lines between eyebrows
Cervical dystonia (a neurological disorder that causes severe neck and shoulder contractions)
29
30
Summary of Key Points to Remember
Two therapeutic groups of muscle relaxants:
A.
Neuromuscular blockers (nondepolarizing and depolarizing)
- Act on nicotinic acetylcholine receptors at neuromuscular junction
- Used in surgical relaxation, endotracheal intubation, control of ventilation and treatment of convulsions
B. Spasmolytics (typically act on targets in the spinal chord)
- Used to treat spasticity associated cerebral palsy, multiple sclerosis, and stroke
31
Thank you for completing this module
Email:
Anand.20@osu.edu
Reference: Bertram Katzung et al,
"Basic and Clinical Pharmacology",
12th edition, McGraw-Hill Lange, Chapter 27
Survey
We would appreciate your feedback on this module. Click on the button below to complete a brief survey. Your responses and comments will be shared with the module’s author, the LSI
EdTech team, and LSI curriculum leaders. We will use your feedback to improve future versions of the module.
The survey is both optional and anonymous and should take less than 5 minutes to complete.
Sur vey