General Anesthetics - Department of Pharmacology
advertisement

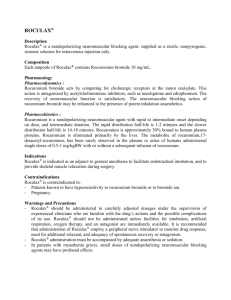
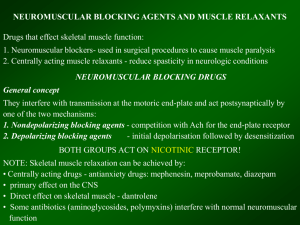
Neuromuscular Blocking Drugs Michael H. Ossipov, Ph.D. Department of Pharmacology Neuromuscular blocking drugs • Extract of vines (Strychnos toxifera; also Chondrodendron species) • Used by indegenous peoples of Amazon basin in poison arrows (not orally active, so food is safe to eat) • Brought to Europe by Sir Walter Raleigh, others • Curare-type drugs: Tubocurare (bamboo tubes), Gourd curare, Pot curare • Brody (1811) showed curare is not lethal is animal is ventilated • Harley (1850) used curare for tetanus and strychnine poisoning • Harold King (1935) isolates d-tubocurarine from a museum sample – determines structure. Neuromuscular blocking drugs • Block synaptic transmission at the neuromuscular junction • Affect synaptic transmission only at skeletal muscle – Does not affect nerve transmission, action potential generation • Act at nicotinic acetylcholine receptor NII Neuromuscular blocking drugs (CH3)3N+-(CH2)6-N+(CH3)3 Hexamethonium (ganglionic) (CH3)3N+-(CH2)10-N+(CH3)3 Decamethonium (motor endplate) Neuromuscular blocking drugs • Acetylcholine is released from motor neurons in discrete quanta • Causes “all-or-none” rapid opening of Na+/K+ channels (duration 1 msec) • Development of miniature end-plate potentials (mEPP) • Summate to form EPP and muscle action potential – results in muscle contraction • ACh is rapidly hydrolyzed by acetylcholinesterase; no rebinding to receptor occurs unless AChE inhibitor is present Non-depolarizing Neuromuscular blocking drugs • Competetive antagonist of the nicotinic 2 receptor • Blocks ACh from acting at motor end-plate – Reduction to 70% of initial EPP needed to prevent muscle action potential • Muscle is insensitive to added Ach, but reactive to K+ or electrical current • AChE inhibitors increase presence of ACh, shifting equilibrium to favor displacing the antagonist from motor end-plate Nondepolarizing drugs: Metabolism • Important in patients with impaired organ clearance or plasmacholinesterase deficiency • Hepatic metabolism and renal excretion (most common) • Atracurium, cis-atracurium: nonenzymatic (Hoffman elimination) • Mivacurium: plasma cholinesterase Depolarizing Neuromuscular blocking drugs • Succinylcholine, decamethonium • Bind to motor end-plate and cause immediate and persistent depolarization • Initial contraction, fasciculations • Muscle is then in a depolarized, refractory state • Desensitization of Ach receptors • Insensitive to K+, electrical stimulation • Paralyzes skeletal more than respiratory muscles Succinlycholine: Pharmacokinetics • Fast onset (1 min) • Short duration of action (2 to 3 min) • Rapidly hydrolyzed by plasma cholinesterase Succinlycholine: Clinical uses • Tracheal intubation • Indicated when rapid onset is desired (patient with a full stomach) • Indicated when a short duration is desired (potentially difficult airway) Succinylcholine: Side effects • Prolonged neuromuscular blockade – In patients lacking pseudocholinesterase • Treat by maintaining ventilation until it wears off hours later Succinylcholine: Phase II block • • • • Prolonged exposure to succinlycholine Features of nondepolarizing blockade May take several hours to resolve May occur in patients unable to metabolize succinylcholine (cholinesterase defects, inhibitors) • Harmless if recognized Acetylcholinesterase inhibitors • Acetylcholinesterase inhibitors have muscarinic effects – – – – Bronchospasm Urination Intestinal cramping Bradycardia • Prevented by muscarinic blocking agent Selection of muscle relexant: • Onset and duration • Route of metabolism and elimination Monitoring NM blockade • Stimulate nerve • Measure motor response (twitch) • Depolarizing neuromuscular blocker – Strength of twitch • Nondepolarizing neuromuscular blocker – Strength of twitch – Decrease in strength of twitch with repeated stimulation