Acute Subdural Hematoma
advertisement
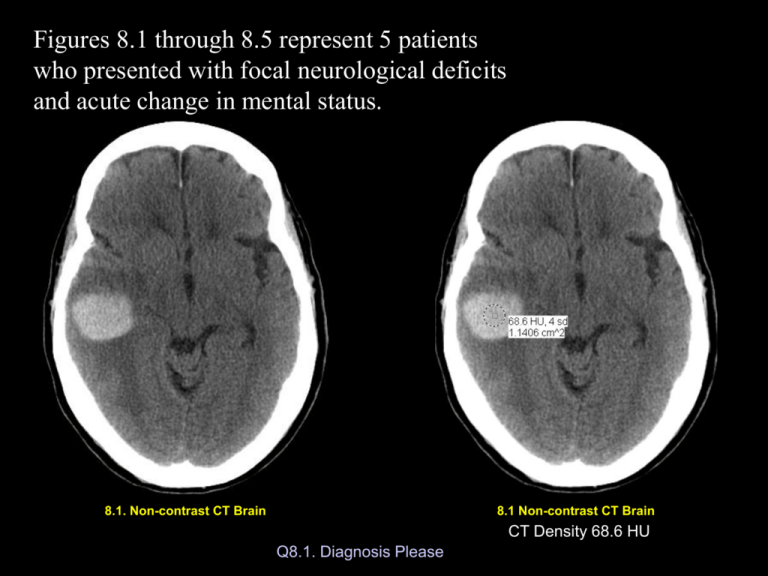
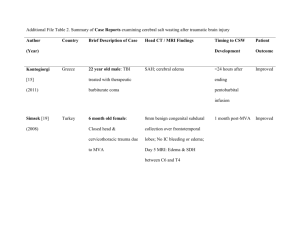
Figures 8.1 through 8.5 represent 5 patients who presented with focal neurological deficits and acute change in mental status. 8.1. Non-contrast CT Brain 8.1 Non-contrast CT Brain CT Density 68.6 HU Q8.1. Diagnosis Please 8.2. Non-contrast CT Brain 8.2 Non-contrast CT Brain CT Density 72.9 HU Q8.2. Diagnosis Please 8.3a. Non-contrast CT Brain 8.3b&c. Non-contrast CT Brain 09/02/2003 CT Density 25.0 HU 09/21/2003 Q8.3. Diagnosis Please 8.4a. Non-contrast CT Brain 8.4b. Non-contrast CT Brain Q8.4. Diagnosis Please 8.4c. Non-contrast CT Brain 8.5 Non-contrast CT Brain Q8.5. Diagnosis Please Figure 1: Acute intracerebral hematoma within the right temporal lobe (arrow) with surrounding edema (E). 60 year-old patient with melanoma. Hemorrhage is from metastatic tumor bleed. E 8.1 Non-contrast CT Brain CT Density 68.6 HU (Hounsfield Units) Acute Intracerebral hematoma: Acute hematoma is seen by non-contrast imaging as an area of high density with density numbers ranging from 40 to 90HU. CT can detect acute intracerebral blood as small as 2mm, due to contrast between high-density of blood and low-density of surrounding brain (arrows). Acute Subdural Hematoma: Subdural hematoma is located between the layers of dura and arachnoid mater, covering the cerebral hemispheres whereas intracerebral hematoma is localized within the brain substance. 8.2 Non-contrast CT Brain Acute subdural hematoma is recognized by CT as an area of peripheral zone of crescentic shaped increased density, outside the surface of the brain (arrows). Most subdural hematoma is caused by tear of bridging cortical veins. Acute subdural hematoma covering the right cerebral hemisphere (arrows), more prominent posteriorly. CT density of blood is 74HU consistent with acute blood. Patient with history of recent fall. Acute subdural hematoma can evolve over a period of time and thus classified as acute, subacute and chronic hematoma. Acute Subdural Hematoma: Up to 7 day old High CT density (40-90HU) Subacute Subdural Hematoma (7 to 21 days old) The CT density of acute blood gradually decreases and becomes isodense with adjacent brain, thus less readily visible and can be easily overlooked. A: Left frontal chronic subdural hematoma (arrowheads) seen as an area of low-density with crescentic inter margin, compressing the adjacent brain. B: Left frontal subdural hematoma was completely evaluated using burr holes in the skull, but the right chronic subdural hematoma has increased in size in the follow-up CT done 19 days later (arrows) which was also subsequently evaluated. 55 year-old patient with chronic myelogenous leukemia with low platelet count. 8.3a. Non-contrast CT Brain 09/02/2003 8.3b&c. Non-contrast CT Brain CT Density 25.0 HU (Hounsfield Units) 09/21/2003 Chronic Subdural Hematoma: Over 21 days old: Acute blood as it evolves, it undergoes liquefaction, and also mixes with cerebrospinal fluid from adjacent subarachnoid space, thus converting into a serosanguineous fluid. This fluid has low CT density reaching close or similar to cerebrospinal fluid. Slow movement of subarachnoid fluid into the subdural hematoma can give rise to gradual expansion of subdural hematoma that can exert mass effect upon the adjacent brain with or without brain edema. This can produce herniation of the brain resulting in sudden decompensation of the patient leading to coma. Thus even a chronic subdural hematoma might need an emergent neurosurgical intervention. 8.4a,b,c. Non-contrast CT Brain Subarachnoid Hemorrhage: Subarachnoid blood is recognized by visualizing the high-density of acute blood outlining the cerebral sulci and subarachnoid cisterns. Subarachnoid Blood Subarachnoid blood filling the right cerebral sulci (arrow), related to recent pituitary surgery Shunt-induced (arrow), intraventricular blood (v). Intraventricular blood is recognized by replacement of normal CSF density by highdensity of blood. v Intraventricular Hemorrhage: Intraventricular blood is easily recognized by high-density blood outlining the lateral ventricles, III ventricle and IV ventricle. 8.5 Non-contrast CT Brain Questionaire #8.6 Common cause of intracranial hemorrhage in a county hospital emergency room. a) Rupture of arterio-venous malformation b) Rupture of cerebral aneurysm c) Trauma d) Hypertension e) Stroke Questionaire #8.6 Common cause of intracranial hemorrhage in a county hospital emergency room. a) Rupture of arterio-venous malformation b) Rupture of cerebral aneurysm c) Trauma d) Hypertension e) Stroke Questionaire #8.7 Likely cause of nontraumatic intracranial hemorrhage in an 8 year-old girl. a) b) c) d) Rupture of arterio-venous malformation Rupture of cerebral aneurysm Hypertension Stroke Questionaire #8.7 Likely cause of nontraumatic intracranial hemorrhage in an 8 year-old girl. a) Rupture of arterio-venous malformation b) c) d) Rupture of cerebral aneurysm Hypertension Stroke Questionaire #8.8 35 year-old man developed severe headache and drowsiness while having sex. The patient was taken to the emergency room and a CT scan showed subarachnoid hemorrhage. Most likely cause for subarachnoid hemorrhage to be considered is: a) b) c) d) e) Rupture of arterio-venous malformation Rupture of small vessel within the brain from excitement, nothing to worry about. Rupture of cerebral aneurysm Acute migraine Stroke Questionaire #8.8 35 year-old man developed severe headache and drowsiness while having sex. The patient was taken to the emergency room and a CT scan showed subarachnoid hemorrhage. Most likely cause for subarachnoid hemorrhage to be considered is: a) b) Rupture of arterio-venous malformation Rupture of small vessel within the brain from excitement, nothing to worry about. c) Rupture of cerebral aneurysm d) e) Acute migraine Stroke Common Etiology for Nontraumatic intracranial Hemorrhage Congenital: Arterio-venous malformations Cerebral berry aneurysms Tumors: Primary: Glioblastoma Vascular: Embolic Infarction Venous Sinus Thrombosis Hypertension Coagulopathy Metastasis: Melanoma Thyroid Carcinoma Renal Cell Carcinoma Chorio Carcinoma