Kalpesh Dixit (Acute on Chronic Subdural
advertisement

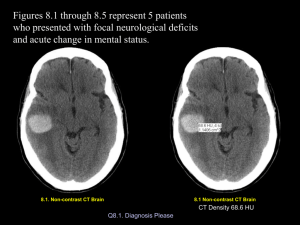
KALPESH DIXIT AIMS CASE DETAILS DISCUSSION ON THOUGHT PROCESSES AND REPORT FURTHER ISSUES OUTCOME OF CASE FUTURE PROBLEMS FINAL DIAGNOSIS CONCLUSIONS AND LEARNING CASE BA, 8 months. Visit Royal Oldham, August, Trivial fall in July and then August Swelling left side of head- increasing Referral to RMCH- neurosurgery CT – previous craniotomy, burr hole, subdural hematomas bilateral L > R, dual attenuation of subdurals, hematoma under scalp left parietal region. Acute bleed and cranial swelling hyperdense but equal in density Case MR SCAN- acute on chronic subdural collection with more recent bleed, bilateral extending into the posterior inter-hemispheric fissures. Dating of subdural collections about 3 weeks before scan, intensity of acute subdural collection and scalp hematoma – same Increased intensity ? Due to sedimentation ? Acute bleed. Left temporal and parietal atrophy compared to right CP medical Dad unaware of fall Previous history in Pakistan about 3 months ago. D & V- pale, low Hb, fits followed by Rt sided weakness. Glasgow coma scale -4/15 CT- left large extradural hematoma with no fractureevacuation- improvement History of fall??. Skeletal survey normal. First cousins, close family ties. Case CP medical Findings normal apart from left parietal swelling. Normal neurology. No other bruises. Opinion Facts: Extradural hematoma with no history and Ix done in Pakistan Trivial falls Boggy increasing swelling CT and MR reports acute on chronic bleeds? NAI or other? Discussion Consideration of NAI in view of MR scan report Discussion with Neurosurgeon in Pakistan Correspondence obtained Reports Bloods normal, Coagulation normal. Case conference – in foster care Subsequent events Parents denied causation Further opinions Further presentations with bruises Further discussions with hematologists Normal clotting, normal factor 8 and VW factor. Platelet assay normal. Meetings at solicitors with evidence base. Multiprofessionals meeting Note previous neurosurgery Subdurals common 1st event in july trivial fall could have caused bleed 2nd event from settee further injury and scalp bleed Thus acute on chronic appearances However why bilateral appearances Literature evidence revisited. Literature Intentional: Shaken baby +/-impact Non-intentional: RTA Neurosurgery Perinatal events and traumatic birth Cranial malformations-arachnoid cystsminor trauma can cause SDH Infections Coagulation disorders (factor 8, VWD, DIC, sickle, Leukemia, ITP, HDN) Metabolic- Glutaric aciduria, Galactosuria Hypernatremia- salt poisoning. Evidence Americal Journal of Paediatrics: Fatal abusive head injuries in infants and children: rebleeding spontaneous should not be offered as explanation in absence of previous injury and re injury which may be trivial. Paediatric chronic subdural hematoma: a retrospective analysis; Paediatric Neurosurgery 1992 Waxing and waning during course and so re bleeding with trivial trauma/impact. Literature Trial of Randall Alexander -Georgia v Brady: during organisation of subdurals- blood vessels which are forming are still fragile and with minor bump one can get a fresh bleeding. Re bleeds are venous and gradual so often there may not be symptoms. Classic thinking “Sometimes identification of a chronic and acute SDH makes the well-paid ‘prosecution experts’ jump to the conclusion that his finding must mean recurrent abuse when in fact the opposite conclusion may be more appropriate. The simple fact that the baby was well-cared for and had no visible external injuries when seen repeatedly for routing paediatric care , while having a subdural haemorrhage, is strong evidence against inflicted trauma”- Shaken or not: that is the question- Edward Yazbak Final answer Repeat and extensive hematology tests Factor 13 deficiency detected. Note no previous bleed Explanation more easy Child back with parents Factor 13 deficiency Factor 13 responsible for crosslinking of fibrin clot. Hence instability of clot and delayed haemorrhage. Typically D 1 trauma- bleeding after 12-36 hours(pathognomonic of Factor 13 deficiency) Often mild bruising seen Delayed separation of cord with bleeding Poor wound healing. CNS haemorrhage is frequent and occurs spontaneously after trivial trauma(25-30%) Soft tissue bleeding and bruising very common. Bleeding oral and gums during teething. Ix- normal INR and aPTT. clot stable for 24 hours if no deficiency. Factor assay. Rx-FFP, cryoppt, Factor 13 concentrate. Learning Detailed history of bleeding tendencies needed Acute on chronic subdurals report may not always mean multiple insults There are many causes of subdural effusion or bleed and one needs to consider them when writing a report. Mixture of CSF with blood causing mixed effects. When and what to do in an extended hematology screen History if suspicious of a disorder Bruising or hematoma which is delayed in appearance after injury. What tests are to be done: FBC + Film PT, APTT, Fibrinogen PFA-100 Factor VIII, von Willebrand Antigen and Activity Urea Clot Lysis screen and a Factor XIII assay. ‘Injustice anywhere is a threat to justice everywhere’ Martin Luther King Jr