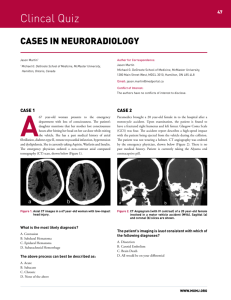
Traumatic Head Injury (Ponder)
advertisement
Traumatic Head Injury Paula Ponder MSN, RN, CEN (Relates to Chapter 63 “Management of Patients with Neurologic Trauma” in the textbook) Learning Objectives • Differentiate head injuries according to mechanism of injury and clinical signs and symptoms • Identify diagnostic testing, and treatment options • Describe the nursing management of patients with head injury • Discuss the need for injury prevention Head Injury • Any trauma to the – Scalp – Skull – Brain • Head trauma includes an alteration in consciousness, no matter how brief Head Injury • Causes – Motor vehicle accidents • Account for ½ of all traumatic brain injury in the US – – – – – – Falls Assaults Firearm-related injuries Sports-related injuries Recreational accidents Highest risk group is ages 15-24, males 2x as likely as women • Advise drivers to obey traffic laws, and to avoid speeding or driving when under the influence of drugs or alcohol. • Advise all drivers and passengers to wear seat belts and shoulder harnesses. Children younger than 12 years of age should be restrained in an age/size-appropriate system in the back seat. • Caution passengers against riding in the back of pickup trucks. • Advise motorcyclists, scooter riders, bicyclists, skateboarders, and roller skaters to wear helmets. • Promote educational programs that are directed toward violence and suicide prevention in the community. • Provide water safety instruction. • Teach patients steps that can be taken to prevent falls, particularly in the elderly. • Advise athletes to use protective devices. Recommend that coaches be educated in proper coaching techniques. • Advise owners of firearms to keep them locked in a secure area where children cannot access them. Head Injury • High potential for poor outcome • Deaths occur at three points in time after injury – Immediately after the injury • From the injury itself – Within 2 hours after injury • From a progressive injury or internal injury – 3 Weeks after injury • MODS • Primary injury – Contusion, puncture, ect. – Only the stuff that happens at the injury, the stuff that happens right then and there • Secondary Injury – Happens afterward – IICP, inadequate oxygenation Head Injury Types of Head Injuries • Scalp lacerations – Can bleed profusely • Skull fractures – Linear or depressed • Linear is from a low velocity injury – Simple, comminuted, or compound • Simple with or without fragments is low velocity • Comminuted is a direct blow, high momentum impact. The bone is fragmented into many pieces. • Compound fracture is a severe head injury. Usually a depressed skull fracture with scalp laceration with a communicating pathway into the intracranial cavity – Closed or open • Frontal fracture – May see air in the forehead tissue, CSF coming out of their nose • Orbital fracture – Raccoon eyes, may have optic nerve injury • Parietal fracture – Battle signs, facial paralysis • Basilar fracture – CSF out ears, nose, battle signs, trouble hearing or tinnitus, facial paralysis, conjugate gaze, vertigo. There is a tear in the dura so there is an open pathway. B/c of where the break/tear is you wouldn’t put an NG tube in, it’s an open pathway from your nose/ear to your brain!! Might give them meningitis • Minor head trauma Head Injury Types of Head Injuries – Concussion • Temporary loss of neurological functioning with no apparent structural damage! May or may not have loss of consciousness • May have amnesia – Mild and Classic • Mild – may lead to a period of reported or observed confusion, memory lapse, possible loss of consciousness, can include a seizure, HA, dizziness • Classic – does result in a loss of consciousness, usually less than 6 hours. Always accompanied by some degree of post injury amnesia! No apparent structural damage on either one of these guys • Major head trauma – Contusion • Moderate to severe head injury, bruise. Impact of the brain against the skull. Loss of consciousness (associated with stupor and confusion). – Lacerations • Involve actual tearing of the brain tissue, not just the dura. Head Injury • Diffuse axonal injury (DAI) – Widespread axonal damage occurring after a mild, moderate, or severe TBI – Process takes approximately 12 to 24 hours – Damage occurs around • Axons in subcortical white matter of the cerebral hemispheres • Basal ganglia • Thalamus • Brainstem • Associated with prolonged coma, poorest prognosis of any other brain injury we have. Usually come in in a coma already, they are posturing, global cerebral edema, diagnosis is made with CT or MRI. Shearing type thing, as the brain shears there are little tears. Then injury stops and settles back down, doesn’t look like an injury on the initial scan, but as time passes you being to see these little blood spots. Usually in white matter associated with acceleration and deceleration injury. Coup/ContreCoup injury. Responsible for most cases of post traumatic dementia, also in conjunction with hypoxic ischemic injury. Most common cause of persistent vegetative state. Slight movements are usually reflexes, but not always. Head Injury Head Injury • Diffuse axonal injury (DAI) – Clinical signs • Decreased LOC • Increased ICP • Decerebration or decortication (posturing) • Global cerebral edema Head Injury • Epidural hematoma – Results from bleeding between the dura and the inner surface of the skull – Neurologic emergency!!! – Venous or arterial origin • 99.9% a tear in the middle meningial arterial artery, the source of bleeding is arterial • Presents with head injury with breif period of unconsciousness followed by a lucid period where consciousness is regained. The lucid period may or may not be there, but if they were out, came back, and went out again you KNOW it’s an epidural hematoma Head Injury • Epidural hematoma – Classic signs include • Initial period of unconsciousness • Brief lucid interval followed by decrease in LOC • Headache • Nausea, vomiting • Focal findings Head Injury • Subdural hematoma – Occurs from bleeding between the dura mater and arachnoid layer of the meningeal covering of the brain – Most common source is the veins that drain the brain surface into the sagittal sinus • Since it’s venous it’s a slower bleed, but still an emergency! • Bleed from the small bridging veins that connect the surface of the cortex to the dural sinuses Head Injury • Subdural hematoma – Usually venous in origin • Much slower to develop into a mass large enough to produce symptoms – May be caused by an arterial hemorrhage Head Injury • Subdural hematoma – Acute subdural hematoma • Signs within 48 hours of the injury • Similar signs and symptoms to brain tissue compression in increased ICP – Drowsy, confused, HA • Patient appears drowsy and confused • Ipsilateral pupil dilates and becomes fixed – Dilates on the side of the bleed and stays dilated – Associated with high mortality b/c of the severe secondary injuries that are associated with it. Often uncontrolled rise in ICP – Caused by crash, moment of impact stuff, hit in the head with a baseball Head Injury • Subdural hematoma – Subacute subdural hematoma • Occurs within 2 to 14 days of the injury • After initial bleeding, subdural hematoma may appear to enlarge over time • Slow as shit bleed, it takes 2 – 14 days to start causing problems. Or from small acute subdural that they thought had stopped, but a little bit of increased ICP re-pops the shiz Head Injury • Subdural hematoma – Chronic subdural hematoma • Develops over weeks or months after a seemingly minor head injury • Peak incidence in sixth and seventh decades of life Head Injury • Subdural hematoma – Chronic subdural hematoma • Presenting complaint often focal symptoms, not signs of increased ICP • Delay in diagnosis in older adults because symptoms mimic those of vascular disease and dementia – Usually older people because there is more space in their heads for swelling or what not, plus as they age their brain atrophies, may be on coumadin, tend to fall more Head Injury • Intracerebral Hematoma – Occurs from bleeding within the parenchyma • Usually occurs within the frontal and temporal lobes • Size and location of hematoma determine patient outcome – Most of the time from a bullet (missile injury), stabbing, Head Injury • Subarachnoid Hematoma – Bleeding into the subarachnoid space • Most common causes are subarachnoid aneurysm, head trauma, or hypertension • Mean age is 50, super bad, people die all the time… Mortality is high, maybe because there is usually something else going on in their body that is messed up that lead them to having the berry aneurysm and bleed in the first place Intracerebral and Subarachnoid Hematoma Berry aneurysm Berry aneurysm Subarachnoid Bleed • Symptoms – – – – Worst HA of their life Photosensitive Nausea Don’t put these guys out in the lobby because you think they have a migrane. They may have a subarachnoid bleed • Vasospasm in the head – narrowing of the lumen of a vessel, serious complication of subarachnoid bleed, leading cause of mortality of people who didn’t initially die with the subarachnoid bleed. Usually 3-14 days after initial hemorrhage. S/S reflect the area of the brain involved, worse HA, decreased LOC, confusion, new focal deficit. Med is Nimotop, also triple H therapy (hypervolemia, induced arterial HTN, and hemodilute them) Head Injury Diagnostic Studies and Collaborative Care • CT scan – Best diagnostic test to determine craniocerebral trauma • MRI • PET • Transcranial Doppler studies – Looking for vasospasm • Cervical spine x-ray – You must see from 1 – 7 to see that they have no injury • Glasgow Coma Scale (GCS) Head Injury Diagnostic Studies and Collaborative Care • Treatment principles – Prevent secondary injury in the brain – Timely diagnosis – Surgery if necessary • • • • Craniotomy Craniectomy Cranioplasty Burr-hole Head Injury Nursing Management • Nursing assessment – Airway • Semi-Fowler’s positioning, really good oral care – Glasgow Coma Scale score – Neurologic status – Presence of CSF leak • Collaborative problem: Increased ICP Eye opening response Best verbal response Best motor response Spontaneous 4 To voice 3 To pain 2 None 1 Oriented 5 Confused 4 Inappropriate words 3 Incomprehensible sounds 2 None 1 Obeys command 6 Localizes pain 5 Withdraws 4 Flexion 3 Extension 2 None 1 Total 13-15 minor brain injury 3 to 15 9-12 is moderate <8 is severe Head Injury Nursing Management • Planning – Overall goals • Maintain adequate cerebral perfusion • Remain normothermic • Be free from pain, discomfort, and infection • Attain maximal cognitive, motor, and sensory function Head Injury Nursing Management • Nursing implementation – Acute intervention • Maintain cerebral perfusion • Prevent secondary cerebral ischemia • Monitor for changes in neurologic status • Treatment of life-threatening conditions will initially take priority in nursing care Head Injury Nursing Management • Nursing implementation – Ambulatory and home care • Nutrition, Bowel / bladder control • Seizure disorders, Personality changes • Family participation and education Pathologic reflexes • Babinski’s sign – Stroke the bottom of the foot and the toes go up towards the nose means it’s positive, but positive is bad! – Kids is positive until 12 mo or if their bearing weight • Grasp – You put something in their hand nad they don’t let go • Snout – When you touch their lip and they purse the lips, that’s pathological, meaning it’s bad • We need to check noxious stimuli, meaning pinching their nail bed, sternum rub, pinching arm, BUT NO NIPPLES Oculocephalic Reflex • “Doll’s Eye Movement” • Normal Doll’s Eye (brainstem intact) – Eyes move opposite direction of head rotation (remain focused on what pt may be viewing) • Abnormal Doll’s Eye (brainstem injury) – Eyes follow direction of head rotation – Poss. loss of gag & cough reflex • http://medstat.med.utuh.edu • Chart as normal or abnormal 38 Doll’s eyes Oculovestibular Reflex • “Cold Caloric Testing” • Intact brainstem – Nystagmus, w/ eyes slowly move toward ear irrigated w/ cold water & rapid movement away • Severe brainstem damage – Both eyes fixed midline position • Inhibition of reflex – Neuromuscular blockers – Barbiturates 40 Persistent Vegetative State • • • • • absence of awareness of self inability to interact with others lack of language comprehension brain stem function to maintain life condition has continued for at least 1 month Brain Death • Brain death is defined as the irreversible loss of function of the brain, including the brain stem • Brain death is a clinical diagnosis, and a repeat evaluation at least 6 hours later is recommended • Medical documentation should include cause and irreversibility of the condition Brain Death • • • • • Corneal reflex Gag reflex Apnea Angiography Consider an EEG • Cardinal signs of brain death are coma, absence of brain stem function, apnea Life Gift • 806-798-5568 • www.lifegift.org • Organ Procurement Organization – OPO Tissue One donor can help 70 people • • • • • • Bone Skin Tissue – ligaments, tendons Veins Heart valves Eyes/corneas Organs One donor can save 8 lives! • • • • • • Heart Lung (can be single or double) Liver Kidneys (2) Pancreas Intestine Background • Texas law: you are brain dead “when your doctor says you are brain dead” – Family doesn’t have the choice to leave a brain-dead pt on vent indefinitely Brain Death Testing • Clinical exam – GCS 3 – No brain stem reflexes • Apnea test – Baseline ABG is obtained – Vent removed, supplemental O2 provided Brain Death Testing • Cerebral Blood Flow – Scan assesses for entry of dye into brain • Cerebral Arteriogram – 4 vessel study – Absolute determination • EEG – Artifact may cause false interpretation – Slow turnaround on results of study Donor Management • “What’s good for the patient is good for the donor” – Normal labs, ABGs, CXRs – Normal vital signs – Urine output 50-300 ml/hour • Adequate oxygenation How do You sign up? • Register as a donor at www.donatelifetexas.org – Centralized state registry – First person consent – Coordinators can search the registry with the pt’s information, speeding up the donation process Summary • • • • Maintain airway Early diagnosis and treatment Prevention of secondary injury Maintain cerebral perfusion pressure