cyclic neutropenia Am Report 9/9/2009
advertisement

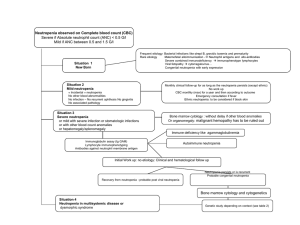
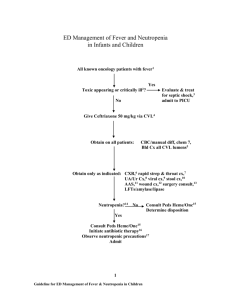
Cat Hathaway Neutropenia Definition of neutropenia is ANC <1500 cells/mm3 African american patients can have ANC of 1000 cells/mm3 w/o complications Severity of neutropenia determines the risk of infection. Mild is 1000-1500, Moderate 500-1000, and severe <500 Neutropenia increases risk of bacterial/suppurative infections. Not parasitic or viral infections. The neutrophil About 60 billion PMNs are produced DAILY! An equal number are circulating in the blood, the half life is 6-8 hrs. Neutropenia occurs if bone marrow production lags behind the amount in circulation, from destruction, ineffective granulopoeisis, or shifts into tissue pools/vascular endothelium Integral in fighting infection of pyogenic bacteria, enteric bacteria, and some fungi Consequences of Neutropenia Drug induced granulocytopenia incurs 610% mortality rate Cancer patients with neutropenic fever have 4-30% mortality rate 21% patients with cancer and neutropenic fever will have serious complications Patients with ANC <500 will develop severe infxn within 1-4 weeks, ANC <1000 is associated with less risk, but still substantial compared to norms Congenital neutropenias Neutropenias associated with immune defects Congenital neutropenia due to mutations Cyclic neutropenia Kostmann Syndrome (Severe Congenital Neutropenia) – Typically die in early childhood Chronic benign neutropenia Neutropenia w/ phenotypic abnormalities Shwachman-diamond-oski syndrome Cartilage-hair hypoplasia syndrome Dyskeratosis congenita Barth Syndrome Chediak Higashi syndrome Congential neutropenia Benign familial neutropenia Don’t mount leukocytosis to infection, but are able to mount fever and inflammatory response. Not associated with higher infection incidence Myeloperoxidase deficiency Not a real neutropenia, lab error because some labs identify neutrophils based on presence of myeloperoxidase Cyclic neutropenia Typically autosomal dominant Found to be due to germline mutations in ELA2 ELA2 encodes neutrophil elastase. Interestingly this protein in molecular studies seems to be an oncoprotein Kostmann syndrome also assoc with ELA2 mutations and GCSF-r mutations and in 10 yrs 21% will go on to develop MDS and or AML Counts cycle every 21 days with nadirs close to 0 and peaks near normal Length of nadir relates to infxs complications Acquired Neutropenia Infections (most common) HIV, erhlichia, parasites, parvo B19, EBV, HepB, HCV Nutritional deficiency B12, copper, folate Drugs/chemicals/chemo (1-3.4 cases/million/yr) Antithyroid, macrolides, procainamide, sulfonamides Clozapine causes agranulocytosis in 1% of patients, but appears to be genetic not immune Immunologic due to BMT or blood tx Felty Syndrome (RA, splenomegaly, neutropenia) Splenic sequestration Complement activation (2/2 ECMO, HD, cardiopulmonary bypass, etc) Other differentials Leukemia (CLL, CML, ALL, AML, hairy cell) Lymphoma (Hodgkin, NonHodgkin) T-LGL – indolent, responds well to immunosuppression PNH Bone marrow failure, MDS MM Autoimmune Neutropenia (Primary and Secondary) SLE, RA are assoc with secondary AIN Primary AIN typically presents in early childhood Work up CBC with diff B12, folate Infectious workup (if fever present) Bcx, ucx, cxr, sputum cx Bone marrow biopsy Esp if anemia/thrombocytopenia also present Can evaluate for maturation arrest, fungal infection, marrow defect, b12/folate deficiency Testing for neutrophil antibodies can be done, but is difficult and false positives and false negatives are common Neutrophil Antibody Assays GIFT (granulocyte immunofluorescent test) – indirect assay using patient’s serum and banked normal PMNs GAT (granulocyte agglutination test) Normal PMNs incubated with serum from pt Tests are difficult secondary to HLA alloantibodies and immune complexes Therefore in routine practice these tests are not recommended Medications/Treatment Depends on etiology of neutropenia Drug related, remove offending agent. Viral related, no treatment typically necessary Avoid rectal exams/give stool softener Neutropenic diet (no fresh fruit/veg) If fever present then broad spectrum abx For chemo related or cyclic neutropenia often tx with GCSF agents Treatment continued Primary AIN Typically not associated with severe infections and often only treated symptomatically for infections w/ abx Secondary AIN Often assoc with SLE/RA – can use GCSF but have to be careful because this can lead to disease flares and leukocytoclastic vasculitis Infections due to neutropenia Management of underlying infxn, supportive abx/treatment Chemotherapy induced neutropenia In patients who have developed prior episodes of neutropenia, often will presumptively treat with GCSF as they are at higher risk for recurrent neutropenia In patients with risk of 20% or more for neutropenia following treatment primary prophylaxis with GCSF may be indicated Danger on the road Resources Neutropenia: Differential Diagnoses & Workup. Author: John E Godwin, MD, MS, Professor of Medicine, Chief Division of Hematology/Oncology, Associate Director, Simmons Cooper Cancer Institute, Southern Illinois University School of Medicine Coauthor(s): Christopher D Braden, DO, Attending Physician, Department of Hematology and Oncology, St. Francis Cancer Center, Indianapolis, Indiana. Updated: Oct 16, 2008. Accessed 9/7/09. Hematology 2004 The American Society of Hematology. Congenital and Acquired Neutropenia Nancy Berliner, Marshall Horwitz and Thomas P. Loughran Jr. Clinical Cornerstone Volume 8, Supplement 5, 2006, Pages S5-S11 Neutropenia: Overview and Current Therapies Congenital neutropenia Robert L Baehner, MD, Last literature review version 17.2: May 2009 | This topic last updated: March 29, 2009. Accessed 9/9/09 Overview of neutropenia Robert L Baehner, MD, Last literature review version 17.2: May 2009 | This topic last updated: February 19, 2009. Accessed 9/9/09