Neutropenic Fever
advertisement
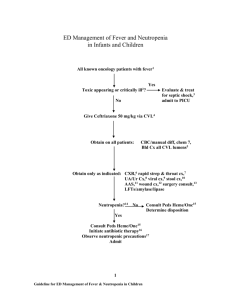
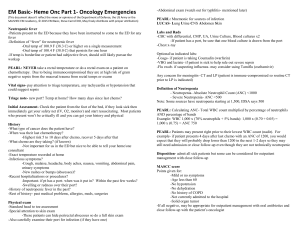
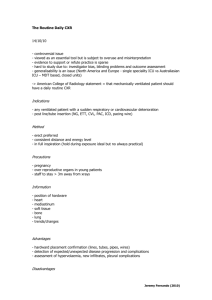
Resident Version Neutropenic Fever Module Created by Dr. Wendy Gerstein Updated 5/09 Objectives: 1) Be able to state definition of neutropenic fever. 2) List two appropriate antibiotics for empiric therapy in a febrile neutropenic patient. 3) Be able to identify appropriate timing for starting empiric antifungal therapy in neutropenic patient. References: 1) Hughes WT, Armstrong D, Bodey GP, et al. 2002 Guidelines for the Use of Antimicrobial Agents in Neutropenic Patients with Cancer. CID 2002:34:730-51. 2) Pizzo PA, Hathorn JW, Hiemenz J, et all. A randomized trial comparing ceftazidime alone with combination antibiotic therapy in cancer patients with fever and neutropenia. N Engl J Med 1986; 315:552. 3) Aoun M. Review: Additional anti-gram positive antibiotics do not reduce allcause mortality in cancer and febrile neutropenia. ACP J Club 2006: 144:3. 4) Walsh TJ, Pappas P, Winston, DJ, et al. Voriconazole compared with liposomal amphotericin B for empirical antifungal therapy in patients with neutropenia and persistent fever. N Engl J Med 2002: 346:225. 5) Walsh TJ, Teppler H, Donowitz GR, et al. Caspofungin versus liposomal amphotericin B for empirical antifungal therapy in patients with persistent fever and neutropenia. N Eng J Med 2004;351:1391. Case: HPI: Pt is a 51 yo male with h/o myelodysplastic syndrome, who was diagnosed with acute myeloid leukemia 4 weeks prior to admission, admitted for induction chemotherapy with cytabine and idarubicin. Five days after completion of chemotherapy, patient developed rigors, fever, and diarrhea, and was neutropenic with ANC of 100. Patient was started on empiric cefepime, and vancomycin was added three days later when fevers continued due to possible portacath infection. All blood and urine cultures were negative. Fevers continued and voriconazole was added for empiric fungal coverage at day five of hospitalization. CT scan of abdomen revealed changes in colon consistent with typhlitis, and flagyl was also started. Patient was still having significant fevers on day eight, and a new CXR shows developing opacities in the RUL and LUL fields. Pmhx: 1) Diabetes, not well controlled 2) Chronic back pain 3) HTN 4) Anemia 5) Tobacco abuse Medications Voriconazole tylenol/oxycodone GCSF Flagyl Lisinopril Vancomycin Insulin Cefepime NKDA Shx: Lives with wife. Retired truck driver. Tob 1 ppd. Drugs: none in 1-2 years - crack and marijuana in past; no IVDU though was stuck by needles in service. No recent etoh. No distant h/o blood transfusion. Put in jail in 1990s for 2-3 days. No known TB contacts. Pt has lived in CA. No international travel. Unknown if had chickenpox as child. Has a dog at home. PE: Tm 102.8, p 100, bp 129/82, O2 saturation 98%RA Gen: alert and oriented, comfortable HEENT: perrla, conjunctiva clear; oropharynx: dentures on top no lesions below; poor dentition below no swelling/redness/pain; no sinus tenderness; cerumen impaction bilateral ears; nares with crusted mucous; no black eschars. Neck without lymphadenopathy or stiffness; right IJ groshong with tenderness at insertion site, appears slightly red, warm to touch; dressing clean. CV: rrr, no mrg heard. Lungs: clear bilaterally, good air movement, no dullness to percussion Abdomen: soft, min distension, normal bowel sounds, non-tender, no masses Ext: no c/c/e, petechiae present on anterior shins. Neuro: CN's intact; sensation intact to light touch; normal gait Skin: no rashes/lesions except noted petechiae on shins. Rectum: no rectal exam done; external exam without evidence of infection. GU: no penile lesions or discharge noted. Labs/Studies: All urine/blood/sputum cultures negative to date. Wbc 0.2, hct 25, plt 18 Bun/cr: 7/1.2 Lfts: tp 5.2, alb 2.8 all others nl, ldh 664 Portable CXR: patchy opacities right upper lobe and left upper lung, consistent with pneumonia. Normal head CT CT abdomen/pelvis: bowel wall thickening and inflammatory changes in the cecum and ascending colon c/w typhlitis and ascending colitis. Based on the new findings on CXR, what would be your next step in management? Anything else concerning to you based on physical exam? Discussion Outline: 1) Definition: Fever 38.3° Celsius (101 F) or ≥ 38° Celsius (100.4 F) for one hour. ANC (absolute neutrophil count) < 500 2) Risk factors: -ANC <100 (20% of these patients are bacteremic if febrile) Rapid decline in ANC Prolonged neutropenia (>10 days) Leukemia induction Cancer not in control Other underlying illnesses 3) Pathogenesis Direct effects of chemotherapy on the mucosal barriers: o Mucositis occurs from mouth to anus, potentially allowing endogenous flora from GI tract to seed the bloodstream. It occurs in about 1/3rd of all patients receiving chemotherapy. Immune defects from underlying hematologic disorders and immunosuppressive effects of chemotherapy increase risk of infection: o Decrease in chemotactic and phagocytic activity of neutrophils, abnormal antibody production or clearing, T cell defects. 4) Causes 30% of patients with neutropenic fevers have an identified source. o Bacterial: GPC > GNR (due to prophylactic antibiotics, lines). o Fungal: candida, aspergillosis, fusarium, mucormycosis. 69% of febrile neutropenic patients at autopsy had evidence of systemic fungal disease. o Also think about reactivation of endemic fungal diseases or TB. o Viral: HSV 1 or 2, EBV, disseminated VZV, HH6, CMV, RSV, Influenza o Anaerobes should be considered if evidence of necrotizing mucositis, sinusitis, periodontal abscess, perirectal abscess, intraabominal infection, or typhlitis. 5) Physical Exam: focus on vitals, skin, HEENT, lungs, abdomen, peri-rectal, line sites, surgical sites. o Remember, if low ANC, minimal signs of inflammation will be present. o Labs/studies: CBC, CMP, cultures (including line), CXR (50% of pts with normal cxr will have an infiltrate seen on CT scan). Have a low threshold for ordering CT scan; bronchoscopy if clinically/radiographically indicated. o Sinus symptoms: CT scan o Abdominal symptoms: CT scan – think about typhlitis (necrotizing neutropenic colitis) o CNS symptoms: MRI, consider LP if not at bleeding risk o Skin biopsy any suspicious lesions. Look for ecthyma gangrenosum – seen with Pseudomonas and S. aureus. o Repeat blood cultures every 48 h if still spiking on therapy, reassess therapy/investigation. 6) Treatment: o Monotherapy or dual therapy (start as soon as cultures drawn) – this is a lifethreatening situation: o Cefepime, imipenem, piperacillin/tazobactam, or ceftazidime for monotherapy (unless patient is septic there is no evidence that dual therapy improves outcome). o B-lactam plus aminoglycoside or B-lactam plus fluoroquinolone if dual therapy needed (septic, history of resistant gram negative rod). o Vancomycin as part of initial therapy only if line appears infected, patient w/ signs of cardiovascular compromise, blood cultures with GPC, or MRSA colonization. Otherwise, not shown to reduce mortality when part of empiric therapy. Linezolid was shown to be non-inferior in RCT if patient cannot tolerate vancomycin. o Antifungal: after 5 days of fever and neutropenia: Liposomal amphotericin is still first line therapy. Caspofungin non-inferior to amphotericin in RCT, but not effective against fusarium, endemic fungi, filamentous molds. Voriconazole if evidence of aspergillus infection based on CT chest or serum galactomannan antigen test. o Antiviral: only based on physical exam, culture results. o G-CSF: shortens duration of neutropenia and hospitalization, but no evidence that it reduces infection-related mortality. o Remove line if tunnel infected, or no response after 2-3d of antibiotic therapy for known catheter infection/bacteremia. 7) Duration: o Afebrile 48 hours, ANC > 500, no source found: discontinue antibiotics. If source found, treat appropriately. o Afebrile, ANC < 500 (no source found): if low risk, discontinue antibiotics after afebrile for 5-7 days. If high risk (had ANC <100, mucositis, unstable vitals) – continue antibiotics until ANC > 500. o If fevers and or neutropenia continue, patient needs to be re-assessed on a regular basis. o Role of oral antibiotic prophylaxis in neutropenic patients: recent meta-analysis showed reduction in death and all cause mortality in hematologic cancer patients, but increase in adverse events and resistance. Still not in IDSA guidelines, decision made on case by case basis. Review Questions: 1) 63 yo male with diabetes, hypertension, and acute myeloid leukemia is hospitalized with neutropenic fevers after induction chemotherapy. Patient is started on cefepime empirically. Three days later vancomycin is added due to presence of Hickman catheter and mild tenderness along insertion site. Blood and urine cultures are negative from 48 hours ago, and his Hickman catheter is now non-tender without any purulence. After six days, fevers continue, and physical exam is remarkable for T max 38.5 C, BP 120/70, P 80, RR 12; no oral lesions, lungs, cardiovascular and abdominal exam are normal, and skin without lesions. ANC is 50, hematocrit 25, platelets 9. Chemistries are notable for normal liver enzymes, normal electrolytes, and baseline creatinine of 2.0 which is unchanged. CXR from two days ago is unremarkable. The next most appropriate management would be: A) Pull the hickman catheter and stop the vancomycin. B) Change the cefepime to piperacillin/tazobactam. C) Start amphotericin after repeating all cultures and CXR. D) Stop all antibiotics, reculture, and obtain chest and abdominal CT scans. E) Start voriconazole after repeating all cultures and CXR. 2) A patient is being treated for leukemia, and has been pancytopenic for several weeks (due to chemotherapy). She has been on prophylactic antibiotics as an outpatient. She is admitted to your service due to onset of fevers. She also has a headache and sinus congestion. On exam you notice some black crusting in her nares, and some palatal erythema. Your next step should be: A) Obtain xrays of the sinuses to evaluate for sinusitis, and start empiric therapy for neutropenic fever with cefepime. B) Obtain stat CT scan of the head/sinuses while calling ENT for immediate consultation, start IV cefepime and high dose liposomal amphotericin. C) Start cefepime and liposomal amphotericin empirically, and base further management on response to therapy. D) Perform LP to evaluate for meningitis, and start empiric vancomycin, ceftriaxone and ampicillin. Post Module Evaluation Please place completed evaluation in an interdepartmental mail envelope and address to Dr. Wendy Gerstein, Department of Medicine, VAMC (111). 1) Topic of module:__________________________ 2) On a scale of 1-5, how effective was this module for learning this topic? _________ (1= not effective at all, 5 = extremely effective) 3) Were there any obvious errors, confusing data, or omissions? Please list/comment below: ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ 4) Was the attending involved in the teaching of this module? Yes/no (please circle). 5) Please provide any further comments/feedback about this module, or the inpatient curriculum in general: 6) Please circle one: Attending Resident (R2/R3) Intern Medical student