Febrile Neutropenia - University of Yeditepe Faculty of Medicine, 2011

Neutropenic Fever
Dr. Meral SÖNMEZOĞLU
Yeditepe University Hospital
1
Learning objects
1.
Know the general terminology
2.
Learn clinical significans and main organisms
3.
Know predisposing factors
4.
Explain the risk assessment (scorring) system
5.
Understand the management strategies and prevention
• Febrile Neutropenia is a medical emergency and must be dealt with immediately.
• Any temperature over 100.1 F (Fahrenheit) or 37.3
C (Celsius) should be reported to the medical oncologist without delay.
• Hours and minutes are critical.
3
Definition
• Febrile Neutropenia
• • Fever
• A single oral Temp > 38.3ºC or ³ 38.0ºC over at least one hour
• • Neutropenia
• Neutrophil count < 500/mm3 or < 1,000/mm3 with a predicted decline to £ 500/mm3
4
When Does Neutropenia Occur?
• Most chemotherapy agents/protocols cause neutropenia nadir at 10-14 days
• But can see anytime from a few days after chemotherapy to up to 4-6 weeks later depending on the agents used
Key Points
• 50% to 60% neutropenic have documented infection
• • Bacteremia noted in ¼ with ANC <100
• • Signs & symptoms are subtle
• • More gram-negative organisms
• • Neutrophil recovery determines treatment
• • Typically 2 to 7 days to respond to antimicrobial therapy
6
Neutrophil?
• Most common white blood cell
— Filled sacs of lysosomes
— Produced in bone marrow
— Half-life approximately 8 hours
— 60 billion produced each day
— Age & race varies production
— Production slower in elderly
— Slightly lower counts in African
7
Role of Neutrophils
• primary defense against bacterial infections
8
Absolute Neutrophil Count
(ANC)
• Is derived by multiplying the WBC count times the percentage of neutrophils in the differential WBC count.
• The percent of neutrophils consists of the segmented (fully mature) neutrophils) + the bands
(almost mature neutrophils)
• ANC = WBC x (% neutrophils + bands)
• The normal range for the ANC = 1.5 to 8.0 (1,500 to 8,000/mm3)
9
ANC Risks
• ANC predicts risk for serious (fatal) infections
• • ANC < 1000/mm3 increases risk of infection
• • ANC < 500/mm3 dramatically increases risk
• • Risk, frequency and severity of infection related to
• – Degree or depth of neutropenia
• – Duration of neutropenia
• – Rate at which neutropenia occurs
10
Neutropenia is defined as…
• ANC < 500 cells/mm3 or
• ANC <1,000 cells/mm3 with a predicted decline to
<500 cells/mm3
— over the next 48 hours
11
Neutropenia
• • Abnormally low proportion of neutrophils
• • Viral infection, chemotherapy and radiotherapy
• • Lowers immunologic barrier to infections
• • Mild neutropenia – ANC falls below 1500/mm3, not > 1000
• • Moderate neutropenia – ANC falls between 500 -
1000/mm3
• • Severe or profound neutropenia – ANC falls below 500/mm3
12
Types of Neutropenia
• • Severe chronic
• • Cyclic
• • Congenital
• • Chronic idiopathic
• • Acquired nonmalignant
• • Chemotherapy/radiation induced
13
Causes of Neutropenia
• Diseases decreasing production of Neutrophils
• – Leukemia, aplastic anemia & myelofibrosis
• – Infections such as virus, tuberculosis & typhoid
• – Abnormalities of bone marrow
• • Destruction or damage of Neutrophils
• – Drug toxicities & vitamin deficiencies
• – Drugs stimulating immune system to attack cells
• – Autoimmune disorders (SLE, RA)
• – Radiation therapy
• – Severe infections
• • Pooling of neutrophils
• – Overwhelming infections
• – Heart-lung bypass & hemodialysis
• • Hypersplenism
14
Complications
• Febrile neutropenia is a potentially lifethreatening complication of myleosuppressive chemotherapy
15
Neutropenia Complications - Fever
• Temperature is the cardinal symptom
• Often the only sign of infection
• Assess 4 x day or ↑ if symptomatic
• Severely neutropenic – often no fever
• Subnormal temperature – severe sepsis
16
NCI defines Febrile Neutropenia as…
• A condition marked by fever and a lower-thannormal number of neutrophils in the blood.
• A single oral temperature of >38 .3
ْ C
• or a temperature of >38 C measured twice over a
1-hour period in a patient with neutropenia of
<1,000 cells/mm3 with a predicted decline to <500 cells/mm3 over the next 48 hours
17
Facts on Febrile Neutropenia
• First identified chemo-induced FN in 1970s, mortality rate was >50%
• Currently mortality rate<5% with proper identification and management
• Only 30-50% of patients have identified sources of infection
18
Clinical Consequences
• • Clinical
• – ↑ risk life threatening infection → death
• – Dose-limiting toxicity of chemotherapy
• – Compromised treatment effectiveness
• – Dose delays and reductions
• – Long-term survival reduced
• • Quality of Life
• – ↑ in anxiety and fatigue
• • Economic
• – Significant ↑ in direct & indirect costs 19
Pathogenesis
• • Normal immune response
• • T & B cells are produced
• • Foreign proteins recognized
• • Neutrophils primary phagocytic responder
• • Neutropenia decreased circulating leukocytes
• • T-lymphocyte function is suppressed
• • Reduced ability to recognize foreign tissue, atypical microbes & viruses
20
the normal action of neutrophils 21
Predisposing Factors
• Treatment Related
• •
Previous history
• • Chemotherapy regimen
• – Anthracyclines
• – Dose-dense regimens
• – Planned relative dose intensity >80%
• • Preexisting neutropenia
• • Extensive prior chemotherapy
• • Concurrent/prior radiotherapy to marrow-containing bone
• • Concurrent use of antibiotics, antifungals, sulfas,
• allopurinol and/or corticosteroids
22
Predisposing Factors
• Patient-Related
• • Age >65 & female
• • Degeneration of immune function
• • Poor performance & nutritional status
• • Open wounds or active tissue infection
• Cancer-Related
• • Bone marrow involvement with tumor
• • Elevated lactic dehydrogenase
• • Advanced or uncontrolled cancer
23
Predisposing Factors
• Comorbidities
• • COPD
• • Cardiovascular disease
• • Hepatic disease ( bili & alk phos)
• • Renal insufficiency (creat. < 30 mL/min)
• • Diabetes mellitus
• • Low baseline hemoglobin
• • Active tissue infection
• • Mucositis
24
Examination of Neutropenic Patient
• Look for a source of the sepsis
• –
General examination
• – Ear, mouth, and nose examination
• – Fundoscopy
• – Gastrointestinal tract
• – Respiratory system
• – Genitourinary tract
• – Cardiovascular system
• – Neurological – eg, neck stiffness
• Remember immunosuppressed patients may not mount clinical signs
25
Common Infection Sites
• • Mucosal damage
• • Primary anatomic sites of infection
• • Skin damage – invasive procedures
• • Bloodstream (15% – 20%)
• • GI tract (enterocolitis & perirectal)
• • Integument (skin, vascular access sites)
• • Respiratory (sinusitis & pneumonia)
26
Evaluation
• Clinical Features
• •
Minimal or absent signs of infection
• • Lack of inflammatory response
• • No erythema, induration or purulence
• • Mental status changes
• • Restlessness and fatigue
• • Diagnostic findings
• – Low albumin level (<3.5 mg/dL)
• – Elevated LDH
• – Elevated Alkaline phosphatase
• – Hyperglycemia
• – Elevated bilirubin
27
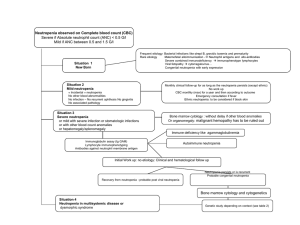
Risk Assessment
• • Two classification systems
• – MASCC
• – Talcott
• • Low Risk
• – Presents with fever only
• – No focus of bacterial infections
• – No chills or hypotension
• – Treatment - oral antibiotics/outpatient
• • High Risk
28
Diagnostic Testing
• • Complete blood count
• • Bone marrow biopsy
• • Immunologic testing
• • Liver function tests
29
Diagnostic Testing
• • CBC, D-dimers and fibrinogen
• • Liver function tests
• • Coagulation screen
• • Chest X-ray
• • Blood cultures
• • Urine dipstick, C & S and cytology
• • Stool C & S, OCP, Clostridium difficile toxin
• • Skin lesions for culture
• • Bronchoscopy and CT scans
30
Diagnostic Testing…
• Cultures
• Practice Guidelines in Oncology – v. 1.2008
• •
Collect during or immediately after spike
• • Two blood samples obtained
• – 1 peripheral & 1 central
• – 2 peripheral or 2 central
• • If indicated, consider
• – nose, oropharynx, urine, stool & rectum
• – vascular access site
• – new or undiagnosed skin lesions
• • If symptomatic, sputum culture followed by x-ray
31
Common Bacterial Pathogens
Associated with FN
• Gram-positive Organisms
• – Staphylococcal species
• • Coagulase-negative
• staphylococci
• • Staphylococcus aureus
• – Streptococcal species
• • Streptococcus
• pneumoniae
• • Streptococcus
• pyogenes
• – Enterococcal species
• – Corynebacterium species
• Gram-negative Organisms
• – Escherichia coli
• – Klebsiella species
• – Pseudomonas aeruginosa
• – Enterobacter species
• – Acinetobacter species
• – Non-aeruginosa
• Pseudomonas species
32
Infection Control
• Educate the patient and family
• – Avoid exposure to risks
• – Control environment risks
• – Avoid invasive procedures
• – Implement measures to lessen severity or longevity
33
Treatment Prophylaxis
Granulocyte-colony stimulating factor
• G-CSF is a growth factor
• Stimulates the bone marrow
• Prophylactic use, eg, following chemotherapy
• Counteract the infection along with antibiotics
• Shortens neutrophil count to recover
• Reserved for high risk neutropenia or recurrent infections
• Evidence does not show any clear benefit for the use of G-
CSF
• Side effects include pain and itchiness at the site of injection
• Can itself cause fever, diarrhea and vomiting
34
Antibiotics –
Broad Spectrum Beta-Lactam
Once cultures collected, begin the following (if no PCN allergy)
• Cefepime (MAXIPIME) 2 gms IV q 8 hr x 7 days or until neutrophil recovery
OR
• Imipenem-cilastatin (PRIMAXIN) 500 mg IVPB over 60 min q 6hrs x 48 hours
OR
• Piperacillin + Tazobactam (ZOSYN) 3.375 gm IV q 6 hrs x
7 – 10 days
35
Antibiotics
• You may also add
• ** Add Vancomycin 1 gm IV q 12hr x 48 hours
(for combination therapy only)
** Clinical Indications for Empiric Vancomycin Therapy
1. Clinically apparent, serious catheter-related infection
2. AML, ALL or NHL
3. Hypotension or septic shock without an identified pathogen
4. Known colonization or past history of MRSA, MRSE, or strep viridians
5. Mucositis (min stage 2) present along with fever
• For patients exhibiting signs of sepsis (according to the SIRS Criteria)
• Gentamicin 5mg/kg IV x one dose
• ( 3 mg/kg if SCr ≥ 1.5 or ≥ 70 years o
36
37
38
39
40
Significance of Febrile Neutropenia?
• Infections in the neutropenic patient can be rapidly fatal if not managed properly
— Mortality rate in the 1960’s was
50%
— With proper management
5% today
Significance of Febrile Neutropenia
• Most patients don ’t have bacterial infection
— 30-50% will have infection
— Primary sites:
GI tract –
Skin
— Risk increases with lower counts (< 0.5 vs. < 0.1) and duration of neutropenia
Significance of Febrile Neutropenia
— But no reliable way of knowing or predicting who is infected
— So all are treated with empiric antibiotics
— Fevers may be due to other infections or to noninfectious causes
Principles of Management of FN
• Risk of documented infection is related to the degree and duration of neutropenia
• Recovery of neutrophil count is critical in response to Rx
• Classic signs and symptoms may be absent
• Untreated infection may disseminate widely
• Broad spectrum antibiotics must be instituted promptly
44
Initial Work-Up of Patients with Fever
And Neutropenia
• Comprehensive history
• • Physical examination (inability to mount an adequate inflammatory response)
• • Diagnostic work-up:
• – CBC
• – Cultures of blood, urine, sputum, wounds, skin lesions etc.
• – CXR
• – Others
45
Presentations of Infection
• Lack of signs and symptoms
• Rapid progression of infection
• Unusual sites of involvement
• Unusual infecting organisms
46
Risks for FN Episodes
• Low-risk pts
• – short-lived neutropenia
• – outpt with no comorbidities
• – access to medical and family assistance
• • High-risk pts
• – prolonged neutropenia
• – uncontrolled cancer
• – comorbidities
• – hematologic malignancies or SCT
• – in the hospital
47
Scoring Index For Identification of
Low Risk Pts
• Extent of illness Score
• – No Sxs 5
• – Mild Sxs 5
• – Moderate sxs 3
• • No hypotension 5
• • No COPD 4
• • Solid tumor or no fungal infection 4
• • No dehydration 3
• • Outpt at onset of fever 3
• • Age < 60 y 2
• Risk index >21 ® low risk pt
48
What Therapy?
Low Risk
— IV combination
— IV Monotherapy
— Oral either inpatient or ??outpatient
— Short admission (24 hrs.) then D/C
High Risk – must be hospitalized
— IV combination or IV monotherapy
— Consider G-CSF
Rx Options for FN
• • Low-risk pts considered for oral in/outpt therapy:
• – FQ ± amox/clav
• • High-risk pts hospitalized for IV AB therapy
50
Selection of Initial Ab Regimen
• Bacterial isolates recovered from other pts at the same
• hospital
• – Type
• – Frequency of occurrence
• – Antibiotic susceptibility
• • Special circumstances (drug allergy, organ disfunction)
• • Inpt or outpt management
• • Future epidemiology depends on the policy in the use
• of antimicrobial agents!!!!
51
Evidence-Based Evaluation of Important
Aspects of Empirical Ab Rx in FN
• No benefit from + of AG to the initial Rx (significantly rate of AE,
• especially nephrotoxicity)
• • No need for empirical + of glycopeptide after 3-4 d of fever
• – In clinically stable pts without resistant or skin/soft tissue
• infections, glycopeptide can be delayed for another 3-4 d
• • The choice of drugs for monotherapy
• – Ceftazidime associated with significantly ¯ response rate vs.
• other Ab (cefepime, pip/tazo, carbapenems)
• • Choice of drug as standard first-line Rx should depend on drug
• costs, local resistance and potential for resistance induction
Glasmacher A . Clin Microbiol Infect 2005;11
52
• Bronchoscopy with BAL
• revealed Pneumocystis jirovecci
• pneumonia
• • He was Rx with
TMP/SMX and
• did well
• • Unusual radiographic findings
• of PCP pneumonia
53
Evidence-Based Evaluation of Important
Aspects of Empirical Ab Rx in FN
54
Other Causes of Persistent Fever
• C difficile colitis
• • Catheter-associated infections
• • Drug fever
• • Graft-versus-host disease
• • Hematomas
• • Pulmonary emboli
• • Splenic infarct
• • TB
• • Underlying disease
• • Adrenal insufficiency 55
Combination IV Therapy
• Combined therapy with at least one drug which covers pseudomonas
— KGH - Cefotaxime & Gentamicin
— Other options: Piperacillin/ aminoglycoside
— Avoid aminoglycosides in those on Cisplatin or other renal toxic agents
Immediate Vancomycin?
• Generally not recommended- add in on basis of cultures
• Recommended for the these situations:
Suspected serious catheter infections
Known colonization with organisms resistant to other antibiotics
+ve blood cultures
hypotension
Monotherapy
• RCT have shown equivalence:
—
Ceftazadime
—
Impenem/Cilastatin
—
Meropenem
Oral Therapy
NEJM July 1999
• Two randomized trials looked at oral vs. IV inpatient therapy in low risk patients
• N= 112 NCI N=356 European
• Slightly different definitions of the low risk group
Oral Therapy
• Both showed that oral therapy with Ciprofloxacin and amoxicillin-clavulanate was equivalent to IV therapy
• Success rates -- oral vs. IV
— 71 vs. 67% / 80 vs. 77%
• No deaths NIH trial
• No differences in the deaths European trial
Duration of Therapy
1.
If ANC
0.5 for two days
+ Afebrile X 48 hrs.
+ No infection
2.
If continued neutropenia continue to 5-7 days of afebrile then D/C
3.
If on IV can be switched to oral medication as directed by cultures or Ciprofloxacin/Clavulin and potentially discharge if stable
Role of G-CSF
• Studies of G-CSF used in febrile neutropenia show:
—
Length of neutropenia but generally not hospitalization
— No mortality advantage
• Generally not recommended
— Exception may be those in high risk group esp. if unstable
Outpatient Therapy
• Can we translate this to the outpatient setting?
— Possibly
Outpatient therapy
• Not considered the standard but is often done
• Must be reliable patient who doesn’t live alone, able to take oral antibiotics
• Re-evaluate q 2days until ANC > 0.5 x 10 9 /L and afebrile x 48hrs.
• If complications or continued fever admit
Neutropenia without fever
• If patient is ill and neutropenic , but doesn’t have fever still treat with same regimens
• Beware in the elderly – might not mount a fever
• afebrile pt. with neutropenia and severe diarrhea –
Ciprofloxacin recommended



![Supplemental: Tables [2] Figures [2] Table 1s. Early Postoperative](http://s3.studylib.net/store/data/007003319_1-b5e4dd5983c70ba65b2a81b50677f101-300x300.png)