Fever Neutropenia - Navy Emergency Medicine
advertisement

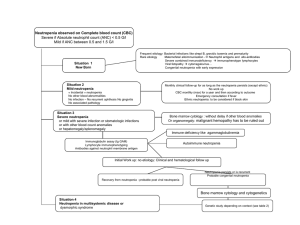
ED Management of Fever and Neutropenia in Infants and Children All known oncology patients with fever1 Yes Toxic appearing or critically ill2? Evaluate & treat for septic shock,3 admit to PICU No Give Ceftriaxone 50 mg/kg via CVL4 Obtain on all patients: CBC/manual diff, chem 7, Bld Cx all CVL lumens5 Obtain only as indicated: CXR,6 rapid strep & throat cx,7 UA/Ur Cx,8 viral cx,9 stool cx,10 AAS,11 wound cx,12 surgery consult,13 LFTs/amylase/lipase Neutropenia?14 No Consult Peds Heme/Onc15 Determine disposition Yes Consult Peds Heme/Onc15 Initiate antibiotic therapy16 Observe neutropenic precautions17 Admit 1 Guideline for ED Management of Fever & Neutropenia in Children Notes: 1 Fever=temp. > 38.0 C. X 2 or > 38.5 C. X 1 within past 24 hrs 2 Toxicity=altered mental status; poor eye contact; inappropriate response to stimuli; abnormal vital signs; poor skin perfusion; cyanosis; grunting 3 For septic shock: a. obtain CBC/manual diff, blood cx all CVL lumens or peripheral if no CVL present, Type & Hold, PT/PTT, fibrinogen, fibrin degradation products b. support BP with isotonic crystalloid (20 mL/kg boluses of NS or LR), vasopressors (dopamine 10-25 mcg/kg/min, epinephrine 0.1-1.0 mcg/kg/min, norepinephrine 0.05-0.5 mcg/kg/min) as indicated c. administer antibiotics: Vancomycin 40 mg/kg/day IV div Q8H + Cefepime 50 mg/kg/dose IV Q8H (max dose 2 gm) 4 If PCN or cephalosporin allergy, discuss with Heme-Onc. 5 Regarding peripheral blood cx: avoid if CVL is present; obtain only if no CVL. 6 Obtain CXR for: persistent cough; SaO2 < 97% (RA); abnormal lung exam; tachypnea; increased work of breathing (flaring/grunting/retractions) 7 Obtain rapid strep & throat cx for: throat pain; tonsillar or pharyngeal erythema/exudate. Send throat cx only if rapid strep negative. 8 Obtain clean voided specimen if possible (avoid catheterization) for symptoms or signs of UTI. 9 Obtain viral cx of discrete oral/pharyngeal lesions. Treat with IV acyclovir if history of HSV. Consider IV acyclovir if no history of HSV. 10 Obtain fecal leukocytes & stool cx for diarrhea 11 Obtain AAS (acute abdominal series), LFTs, amylase/lipase for: abdominal pain; abnormal abdominal exam (tenderness, distension, abnormal bowel sounds, masses or organomegaly). Evaluate for free air or signs/sx consistent with typhilitis. 12 Obtain wound cx of any exudate at CVL site 13 Obtain surgical consult for: free air; or signs/sx consistent with typhilitis 14 Neutropenia = ANC < 500/mm3 or < 1,000/mm3 with predicted decline to < 500/mm3 15 Peds Heme-Onc pager: 669-2131 16 Two options for inpatient antibiotics (unless cephalosporin or PCN allergy, then discuss with Heme/Onc): a. Cefepime (50 mg/kg/dose, max dose 6 gm/day) + Vancomycin (40 mg/kg/day div Q6-8H, max dose 1 gm) if any of the following: (1) clinically obvious and serious CVL-related infection (2) substantial mucosal damage (3) known colonization with β-lactam resistant S. pneumoniae or S. aureus (4) growth of a gram-positive organism from the blood (pending identification and susceptibility testing) 2 Guideline for ED Management of Fever & Neutropenia in Children (5) hypotension or other evidence of cardiovascular dysfunction (6) recent treatment with systemic antibiotics b. Otherwise cefepime (monotherapy) 17 Neutropenic precautions: a. No IM injections UNLESS requested or approved by Heme/Onc. Apply pressure following all IM injections in thrombocytopenic patients. b. No rectal temps. or exams c. No suppositories d. No I&D procedures without Heme/Onc approval e. No NG tubes, urinary catheters, suprapubic bladder aspirates or LPs without Heme/Onc approval f. No venipuncture or IV placement without betadine prep References: Hughes WT, Armstrong D, Bodey GP et al: 1997 Guidelines for the use of antimicrobial agents in neutropenic patients with unexplained fever. Clin Infect Dis 1997;25:551-573 [Practice guidelines for treatment of febrile neutropenic patient.] Mustafa MM, Carlson L, Tkaczewski I, et al. Comparative study of cefepime versus ceftazidime in the empiric treatment of pediatric cancer patients with fever and neutropenia. Pediatr Infect Dis J 2001;20:362-9 [Cefepime appears to be safe and effective compared with ceftazidime for initial empiric therapy of febrile episodes in neutropenic pediatric cancer patients. Chuang YY, Hung IJ, Yang CP, et al. Cefepime versus ceftazidime as empiric monotherapy for fever and neutropenia in children with cancer. Pediatr Infect Dis J 2002;21:203-9 [Cefepime appears to be as effective & safe as ceftazidime for empiric treatment of febrile episodes in neutropenic pediatric cancer patients.] Bruckner LB, Korones DN, Karnauchow T, et. al. High incidence of penicillin resistance among α-hemolytic streptococci isolated from the blood of children with cancer. J Pediatr 2002;140:20-6 [Blood culture isolates of alpha-hemolytic streptococci obtained from children with cancer are frequently resistant to β-lactam antibiotics. Clinically relevant AHS isolates should be tested for antibiotic susceptibility & β-lactam antibiotics may not be optimal empiric therapy for fever & neutropenia in children with cancer who have a high risk of AHS infections.] Haslam DB. Managing the child with fever and neutropenia in an era of increasing microbial resistance. J Pediatr 2002;140:5-7 [Laboratory investigations include a complete blood cell count, culture of urine, and cultures of blood obtained from a 3 Guideline for ED Management of Fever & Neutropenia in Children peripheral vein and indwelling catheters. Comparison of quantitative colony counts from blood cultures from these 2 sites may distinguish catheter-associated infection from another source. Automated blood culture systems currently in use will detect most fungi and anaerobic bacteria. Nevertheless, in the setting of profound neutropenia and compromised mucosal surfaces, it is advisable to culture blood specifically for anaerobic bacteria and fungi. In certain instances, imaging studies such as CXR, ultrasonography, CT, or MRI of the abdomen, sinuses, or other sites may be indicated, particularly if fever is prolonged and no apparent source is identified. Empiric ceftazidime plus an aminoglycoside is one regimen widely used in the treatment of children with fever and neutropenia. Previously, gram-negative organisms accounted for the majority of cases of septicemia in neutropenic children. Recent studies demonstrate the ascension of grampositive organisms. Among the most common isolates, coagulase-negative staphylococci and α-hemolytic streptococci (AHS) account for a large proportion of isolates. Coagulase-negative staphylococcal bacteremia usually arises from contaminated intravascular catheters. AHS, often referred to as viridans streptococci, reside predominantly in the oropharynx and gastrointestinal tract. Damage to mucosal surfaces that often occurs during chemotherapy provides a portal of entry for AHS. Despite the lack of classic virulence factors, these organisms are sometimes associated with fulminant infections. Resistance to β-lactam antibiotics among AHS results from alterations in penicillin-binding proteins rather than from production of a β-lactamase. Consequently, addition of a β-lactamase inhibitor, such as sulbactam or tazobactam, to a β-lactam agent would have no effect on AHS susceptibility. Vancomycin is commonly used to treat serious AHS infections when the isolate is known to be β-lactam resistant because no other antibiotic available currently has predictable activity against such organisms. Although some studies demonstrated a higher treatment failure rate among patients infected with AHS who did not receive empiric vancomycin compared with those who did, overall mortality rates were not different. These observations are considered in the context of emerging vancomycin resistance among some gram-positive organisms, particularly enterococci. It should be recalled that < 20% patients with febrile neutropenia will have documented bacteremia; of these, approximately 25% will be caused by AHS. With the resistance rates presented here, approximately 1 of 40 children with fever and neutropenia could be expected to have bacteremia as a result of β-lactamresistant AHS. Unfortunately, some of these cases will be fulminant and fatal. However, initial therapy with vancomycin by no means guarantees of a cure. Two cases presented by Bruckner et al.highlight the fact that blood cultures may remain positive for AHS, or infection may relapse, despite vancomycin therapy. A study by Marron et al. reported that, among 8 patients with serious AHS bacteremia who were treated empirically with vancomycin, 5 died. Guidelines for the empiric use of vancomycin that were published 5 years ago by the Infectious Disease Society of America remain valid.] They suggest that only select patients receive vancomycin as part of their initial therapy. Indications include (1) clinically obvious and serious catheter-related infections, (2) substantial mucosal damage, (3) known colonization with β-lactam resistant Streptococcus pneumoniae or Staphylcoccus aureus, (4) growth of a gram-positive organism from the blood (pending identification and susceptibility testing), and (5) hypotension or other evidence of cardiovascular dysfunction. On the basis of the data presented by Bruckner et al. recent treatment with systemic antibiotics might be an additional consideration.] 4 Guideline for ED Management of Fever & Neutropenia in Children 5 Guideline for ED Management of Fever & Neutropenia in Children