PowerPoint - Honors Human Physiology
advertisement

NROSCI/BIOSCI 1070
MSNBIO 2070
Human Physiology
September 4, 2015
Muscle 1
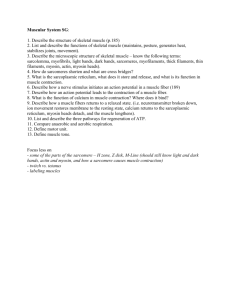
Sarcolemma = cell membrane
Myofibril = basic contractile unit
Myofibril comprised of 1500 myosin
filaments and 3000 actin filaments
Overlap of myosin and actin
produces dark A bands
Actin alone produces light I band
Actin is secured to Z membranes,
which pass from myofibril to
myofibril (hold everything together)
Sarcomere = portion of a myofibril
between two Z membranes
H zone = band produced when
myosin exists without actin (artifact;
not in living muscle)
Sarcoplasm = muscle cell
cytoplasm
Sarcoplasmic reticulum =
Define: A band, I band, H zone, Z
membrane, sarcomere, mitochondria
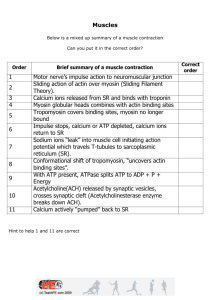
Mechanism of Muscle
Contraction
o When muscle
contracts, the Z
membranes come
closer together, and
the I zones and
sarcomeres decrease
in width. No H zone
is present.
o This is the sliding
filament mechanism
of muscle
contraction.
What Causes Muscle
Contraction?
Actin appears to be “ratcheted inward” by
the actions of the myosin cross bridges
This ratcheting is due to attractive forces
between the actin and myosin
The attractive forces are inhibited when
muscle is relaxed
The activation of the attractive forces
appears to require: Ca++ and ATP
Molecular Characteristics of Myosin
Each myosin molecule is
composed of 6
polypeptide chains: 2
heavy chains and 4 light
chains
The heavy chains form the
tail
The light chains in
association with the heavy
chains form the head
200 or more myosin
molecules form a myosin
filament
Molecular Characteristics of Myosin
The portion of the myosin
tails farthest from the
head form the body of the
myosin filament
The head and adjacent
tail form the cross bridge
The cross bridge is
“hinged” at two points:
where it emerges from the
body and at the junction
with the head
Molecular Characteristics of Actin
Actin filaments are composed of actin, tropomyosin, and troponin
The backbone of the actin filament is comprised of
F-actin protein
Along the F-actin helix are active sites where
myosin has a high affinity
In the resting state, the tropomyosin strand covers
the active sites
Molecular Characteristics of Actin
The actin filament also includes troponin, which is
comprised of three globular proteins
One of the globular proteins has affinity for actin,
another for tropomyosin, and the third for Ca++
It is believed that when Ca++ binds to troponin, a
conformational change occurs, pulling tropomyosin
away from the active sites and exposing them.
THIS INITIATES MUSCLE CONTRACTION.
Interaction of Actin
and Myosin to
Produce Contraction
As soon as the active sites are uncovered, the heads of the
cross bridges immediately attach to the actin molecules at
these points.
A configuration change then takes place in the cross bridge,
causing the head to tilt while pulling the actin filament along
with it.
This tilt of the head of the cross bridge is called the power
stroke, and is the major mechanism in muscle contraction.
After the power stroke is completed (and the configuration of
the myosin molecule has changed), the myosin is no longer
attracted to actin and the two molecules separate.
Interaction of Actin
and Myosin to
Produce Contraction
The myosin then reverts to its original configuration,
and its attraction for actin returns.
The myosin head then attaches to the next available
active site.
Because many cross bridges are cycling out of
phase, when one myosin head detaches the actin
does not slip back to its initial position
Role of ATP in Muscle Contraction
Most of the muscle contraction proceeds without
ATP. The attachment of myosin to actin is not ATP
dependent; neither is the resulting change in
conformation in the myosin molecule
It is believed that this change in shape of the myosin
molecule exposes an ATP binding site. The binding
of ATP to this site causes the myosin to be released
from the actin.
The ATP molecule then degrades to ADP, and the
energy released causes the myosin molecule to
return to its original conformation. The myosin is
then ready to bind to the next actin binding site.
Role of ATP in Muscle Contraction
The rate-limiting step in muscle contraction is
breaking of the ATP high energy bond by the enzyme
myosin ATPase in the myosin head. The faster that
myosin ATPase works to break the high-energy bond,
the faster the cross bridges ratchet the actin
inwards.
The factor that typically leads to a failure in muscle
contraction (muscle ‘fatigue’) is depletion of ATP.
Role of ATP in Muscle Contraction
If ATP were to be depleted, as occurs
following death, then the actin and
myosin molecules would not separate,
and would be permanently fixed together.
This would cause the muscle length to
become fixed, and the muscle would
appear to be very stiff. In fact, this
phenomenon explains “rigor mortis”.
Like most cells, muscle generates ATP
from both glycolysis and oxidative
phosphorylation.
Creatine Phosphate
Muscle cells often require more
ATP than can be produced
through typical mechanisms.
Thus, muscle cells have a
special immediate precursor for
the generation of ATP: creatine
phosphate. Creatine
phosphate is a high-energy
molecule that can rephosphorylate ADP to ATP.
Creatine phosphate levels drop
during muscle contraction; some
athletes consume this chemical
as a “performance enhancer”.
Creatine Phosphate
Creatine can be found in many forms. Muscle contains
approximately 0.5% creatine by weight, although some of
this will be degraded by cooking. Commercial supplements
are also available. It has been suggested that human
muscle has a maximum capacity of roughly 150 mmol
creatine/kg muscle, making supplementation in excess of
20g/day pointless.
A number of studies have examined the effect of creatine
supplementation on performance. The consensus appears
to be that, while not increasing peak force production,
creatine can increase the amount of work done (8%) in the
first few short duration, maximal effort trials. The
mechanism of this enhancement is not yet clearly
documented, but is most likely by increasing the available
pool.
Initiation of Muscle Contraction
An action potential that propagates along the
sarcolemma induces muscle contraction
The muscle action potential is triggered by the
release of acetylcholine from a moto-neuron
terminal, at the neuromuscular junction
The activity of the central nervous system
tightly controls the initiation of muscle action
potentials, and thus muscle contraction
Initiation of Muscle Contraction
The muscle action
potential quickly
propagates deep into a
muscle via transverse
tubules (T-tubules)
The terminal cisternae
of the sarcoplasmic
reticulum abut the T tubules, and become
depolarized when an
action potential
invades.
Initiation of Muscle Contraction
The depolarization of the
sarcoplasmic reticulum
opens voltage-gated Ca++
channels.
Ca++ flows down its
concentration gradient into
the sarcoplasm, binds to the
C (calcium)-troponin
subunit, and initiates
muscle contraction
After 300 msec, an ATP-dependent pump returns the Ca++ to the
sarcoplasmic reticulum, and contraction stops unless another
action potential courses along the muscle membrane.
Length-Tension Relationship in Muscle
Muscle contracts best
when a maximal number
of myosin heads can bind
to actin.
If the resting length of
muscle is too great or too
small, the actin-myosin
relationships are not
optimal and contraction
strength diminishes.
Length-Tension Relationship in Muscle
This concept can also be applied
to a whole muscle.
If the muscle is stretched,tension
develops due to elastic components in the muscle. However,
if contraction is induced in a
stretched muscle, the tension
produced by the contraction will
be small due to minimal overlap
between actin and myosin at the
onset of contraction.
Similarly, if a muscle is compressed, very little tension will
be produced during contraction
because of the altered relationship between actin and myosin.
Motor Units
Motor Unit = Motoneuron +
Muscle Fibers it Innervates
Muscle Unit=Muscle Fibers
Innervated by a Particular
Motoneuron
How many muscle fibers are innervated by a
motoneuron?
Neuromuscular Junction
Synaptic Security at the Neuromuscular Junction is
Very High, So Muscle Always Contracts when a
Motoneuron Fires Unless Something Goes Wrong:
Drug/Condition
Effect on Neuromuscular
Junction
Curare
Blocks ACh receptors
Botulinum toxin
Blocks ACh release
Myasthenia gravis
Autoimmune disease that
results in a loss of ACh
receptors
Question for
Discussion
What is the best
treatment for a patient
with Myasthenia gravis ?
Receptor Subtypes
Binding of a neurotransmitter at one site can
have vastly different effects than at another.
Typically, receptors with differing responses
to the binding of a particular
neurotransmitter also have different
configurations, and affinities for that
neurotransmitter.
It thus may be possible for a particular drug
to bind to one neurotransmitter receptor
“subtype” and not another. This is how
neurotransmitter subtypes are differentiated.
Muscarinic and Nicotinic
Acetylcholine Receptors
The acetylcholine receptor has two major
subtypes: nicotinic and muscarinic
receptors.
The nicotinic receptors bind the plant
alkaloid “nicotine,” whereas the muscarinic
receptors bind the toadstool toxin muscarine.
The agonist for both receptors in the body is
the same (acetylcholine), but the selective
affinity of the subtypes for one drug can be
exploited by pharmacologists.
Nicotinic Receptors
Are composed of 5 protein building
blocks.
All the building blocks have a
similar chemical structure, but
there are some differences.
12 different building blocks and 17
different types of nicotinic
receptors have been discovered.
Depending on the exact
combination of building blocks, the
affinity of a nicotinic receptor for a
particular drug can differ.
Affinity of Different Subtypes of
Nicotinic Receptors for Drugs
Location
Agonists
Antagonists
Neuromusclar
Junction
acetylcholine,
carbachol,
suxamethonium
curare, pancuronium,
α-conotoxin,
α-bungarotoxin
Autonomic
Ganglia
acetylcholine, carbachol,
nicotine, epibatidine
mecamylamine,
α-bungarotoxin,
hexamethonium
Brain
acetylcholine, nicotine,
epibatidine
α-conotoxin,
mecamylamine
Increases in Muscle Force
Muscle force can be increased by two
mechanisms: frequency modulation
(increasing the discharge rate of the
motor unit) or recruitment (activation of
inactive motor units).
If a motoneuron fires before the tension
produced by the previous contraction has
dissipated, then the force of the second
contraction will add to the first.
The faster the firing rate of the motoneuron, the more cumulative force will be
produced until the maximal contractile
ability of the muscle is reached.
Increases in Muscle Force
If a motoneuron fires rapidly enough, a
“plateau” of muscle tension will occur.
This plateau is referred to as a tetanus.
However, recruitment of new motor units
is required for a muscle to develop a
reasonable amount of force; there is a
limit as to how much force a single motor
unit can produce.
Distribution of Muscle Fibers
Innervated by a Single
Motoneuron:
Motor Unit Types
Initial Differentiation: Red vs. White
Muscle (Ranvier)
Motor Unit Types
WHITE
FF (IIb)
FR (IIa)
RED
S (I)
Tension produced
High
Inter
Low
Contraction time
Fast
Inter
Slow
Myosin ATPase speed
High
Inter
Low
Resistance to fatigue
Low
Inter
High
Sparse
Inter
Rich
Oxidative enzymes
Low
Inter
High
Glycolytic enzymes
High
Inter
Low
# of mitochondria
Low
Inter
High
Capillary supply
Motor Unit Types (Burke):
Slow vs. Fast (S or F designation)
Fast contracting < 55 ms
Slow Contracting > 55 ms
Fatigue Index = % Muscle Tension Retained
When Stimulating Continuously for 120 sec
(R {resistant to fatigue} and F {fatigable}
designation)
Motor Unit Properties
Question for
Discussion
Relaxation of Muscle
By definition, relaxation occurs when there is
no contraction, and the muscle returns to its
normal resting length.
This must be done smoothly, but requires no
active expenditure of energy.
When the myosin heads disengage from
actin, relaxation occurs. This process is
“smoothed” by the elastic elements in the
body, both in the muscle itself and structures
to which it is attached.
Clinical note: muscular dystophy