02. and 03. Cell Gro..
advertisement

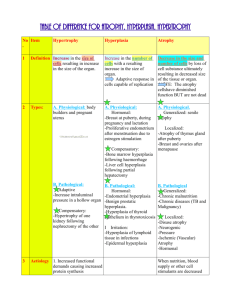
Fundamentals of Systemic Pathology *** Please study the REQUIRED slide simulations at the IOWA website: http://www.path.uiowa.edu/virtualslidebox/iowa_histopathology/ Click on links: Table of Contents Skeletal System 1) Skeletal muscle – Atrophy (View 1 an Normal) Heart 2) Heart – Malignant Hypertension ( Myocardial hypertrophy: View 1 and Annotation) Adaptation & accumulations 3) Endometrium – Hyperplasia 4) Endometrium – Senile atrophy CELL GROWTH, REGENERATION AND REACTION OF CELL TO INJURY INTRODUCTION One of the main goals of the pathology student is to master the new vocabulary involved in describing what one sees underneath the light microscope. When viewing a slide, the student needs to translate the visual image into words. These words need to be specific, exact and expressed in standard terms in medicine and particularly pathology. Your time spent in lecture and in review sessions viewing the histopathology slides will give you the opportunity to become more familiar with converting the visual image into a correct pathologic description of the cellular processes. THE CELL Every cell, tissue and organ of the human body is derived from one single cell, the fertilized egg or zygote. Following fertilization of the female egg with the male sperm, the diploid number of 46 chromosomes is established and this zygote begins to divide. Since these mitotic divisions are occurring while the zygote is floating free through the female fallopian tube, each division produces double the number of cells, however, these cells are now half their original size. This type of division is referred to as cleavage. As the zygote divides, or cleaves, from one to two cells and then from two to four cells, it looks just like an orange being cut first in half and then into quarter sized pieces. By the third day following fertilization, it is a solid ball of 16-32 cells and is now referred to as a morula as it enters the uterus. This solid ball of cells then begins to have its center fill with fluid to create a fluid-filled, hollow ball of cells, the blastocyst. At one end of the blastocyst, the cells begin to divide, or cleave, at a faster rate than the cells at the other end of the blastocyst. This produces an unequal distribution of cells. The end with the cells that are dividing faster will have more, smaller-sized cells. The other end with the cells that are dividing more slowly will have fewer, larger-sized cells. The end, or pole, with more, smaller cells is called the “inner cell mass” or the “embryoblast”. These cells will eventually grow to form the embryo itself. The end, or pole, with the fewer, larger-sized cells is called the “trophoblast” (consisting of trophoblastic cells) and it will grow to become the supporting tissues of the placenta. On approximately day 10 following fertilization, the cells of the inner cell mass form three distinct layers. These three “germ layers” are the (1) ectoderm, (2) mesoderm, and (3) endoderm. The ectodermal cells will eventually develop into skin and nervous tissue. The mesodermal cells will eventually develop into the muscles and bones. The endodermal cells will eventually develop into the inner body linings, such as the lining of the bladder and urinary system; the lining of the digestive system; and the lining of the respiratory system. There is great significance in these three germ layers in that only now at this time in embryonic development do these cells show determination in that they are committed to differentiate into a specific specialized cell and tissue. There are three main processes going on during development of the embryo and fetus: Differentiation, Migration, and Morphogenesis. CELLULAR COMPONENTS It would certainly be useful to spend a little time on your own reviewing the functions of the different parts of a human cell. Since you will be viewing human tissues, what you will need to identify as either normal or abnormal components of a human cell include: Phospholipid Bilayer: This material is used as the cell membrane; nuclear membrane; endoplasmic reticulum; Golgi apparatus; lysosomal membrane; mitochondrial membranes and all types of vesicle or vacuole membranes. Nucleus with the 46, 23-pair, of double-stranded DNA molecules bound with histone proteins, the “chromatin”. The nucleus also contains the “nucleolus”. Ribosomes: Protein and structural RNA. Cytoskeletal Structures: Microtubules; Intermediate Filaments; Microfilaments Also, what is outside and in between the cells: Collagen; Reticular Fibers; Elastic Fibers; Glycoproteins; Proteoglycans. GIVING COLOR TO THE CELLS We could certainly view every component of any cell with excellent detail if we viewed them using the electron microscope. However, this is not practical. You will be viewing pictures taken using a light microscope. Since the cells in their natural state have very little if any color or contrast, we will need to dye or ‘stain’ the cells and tissues before we can see their components using the light microscope. Over time, many dyes, or stains, have been found to work well. There are specific dyes that stain RNA, protein, elastic fibers and so forth very well. Two very common stains are hematoxylin and eosin. They are commonly used together, producing the commonly seen “H&E” stain. Hematoxylin is a blue dye that is positively charged (cationic). It will then bind to molecules with a negative charged group. It binds, or stains, DNA and RNA very well. It then stains the nucleus well. With an H&E stain, the nucleus appears blue to purple (basophilic). Eosin is a pink dye that is negatively charged (anionic) and therefore will bind to molecules with positively charged groups. Typically the cytoskeleton, some proteins, and collagen fibers bind, or stain, pink with eosin. With the H&E stain, the cytoplasm and extracellular spaces appear pink to red (eosinophilic). FOUR TISSUE TYPES We can divide the entire human body into groups of cells that “look the same” and “act the same”: 1. Nervous tissues (neurons) 2. Muscle tissue (muscle fibers) 3. Epithelial tissues: cells with exposed surfaces. In some cases, these lining cells are secretory. In this case we consider them ‘glandular’. All glands are epithelial tissue. (Examples of epithelial tissue include the skin or epidermis; the linings of the urinary system; linings of the respiratory system; linings of the digestive system; endocrine glands; blood vessels; kidney tubules; pancreas.) 4. Connective tissues: The material that is found between all the solid organs. Few cells, many fibers, fluid and dissolved proteins. (Examples include the dermis, blood, cartilage and bone.) Of the four tissue types, only some cells are programmed to continue to divide throughout the life of the person. Some cells can start to divide if chemically instructed to. And others will never divide again. These three categories are defined as: 1. Labile cells: Continue to divide (Example: bone marrow, skin). 2. Stable cells: Will leave a resting state and begin to divide (Example: liver cells, fibroblasts). 3. Permanent cells: Will never divide again (Example: neurons, cardiac muscle). Labile cells are always going through an orderly sequence of events in order to divide. This orderly sequence of events is defined as the “Cell Cycle”. The cell cycle = G1→S→G2→M; where M in turn is followed by G1. (G1=Gap#1; S=S-phase with DNA replication; G2=Gap#2; M=M-phase or mitosis). Remember that mitosis itself consists of prophase, metaphase, anaphase, and telophase. Interphase is everything that is not M-phase: Interphase = G1+S+G2. Stable cells can enter into the cell cycle from their resting state, which is designated as “G0”. In order to enter the cell cycle, at G1, the stable cells turn on their growth control genes. This is important to remember since it is when these growth control genes ‘go wrong’ that cells will divide ‘out of control’ or become cancerous. CELLULAR RESPONSE TO INJURY There are many causes of cellular injury: -Viruses -Toxins -Ischemia (lack of O2) -Radiation How the cell appears at any specific point in time will be at some place along a continuum of reactive steps that the cell must take to adapt and survive. No → → Little → → Moderate → → Excessive → → → → Cell Injury Injury Injury Injury │ Death │ │ Reversible │ Irreversible Cell Injury │ Cell Injury Remember that throughout this course all you will be looking at and trying to accurately describe are human cells underneath the light microscope. This is probably the most difficult part of mastering histopathology. The only features you have to describe are colors, sizes and shapes of the cells, their interiors, and their arrangements together – that’s it. All you need to do is simply learn how to do this as a pathologist would, so that everyone you communicate with will understand immediately what it is you see when you put it into simple words. When cells are injured, their appearance changes as they react to the injury. As you might expect, since the cells are small machines, many different types of injury will still cause the cells to react in similar ways. Important terms in describing pathologic changes to cells and tissues: I. Hypertrophy: As a result of cellular adaptation to some sort of environmental challenge, injury, or insult, certain cells in the body will undergo an increase in their individual size. And since all the cells themselves will increase in size, the entire tissue, or organ, will increase in size. A good example is skeletal and cardiac muscle. When you exercise your muscles, they become bigger. Why is that? They adapt by manufacturing more actin and myosin. The more actin and myosin cross bridges, the more force of contraction for that muscle cell. So each muscle cell is enlarged with all these additional actin and myosin protein molecules. Overall, the entire muscle is bigger and stronger. This is ‘physiologic hypertrophy’. To have a ‘strong heart’ implies that each cardiac muscle fiber is filled with plenty of actin and myosin so that the heart as a pump can expel blood with speed and force, thus producing a large cardiac output. However, to have the heart pumping against a large resistance (narrowed blood vessels from atherosclerosis) the heart will adapt by undergoing too much hypertrophy. This will produce an extremely strong heart muscle, but all this extra heart muscle tissue will extend into the heart chambers limiting the amount of blood that can fill the two ventricles. This excess hypertrophy reduces the volume of blood ejected from the ventricles and severely diminishes cardiac output. As you see in the following picture, the cross section of the myocardium shows a great deal of cardiac muscle tissue, but very little space for blood to fill the left ventricle. This is considered ‘pathologic hypertrophy’. Link to Iowa web site Virual slide box gross hypertrophy II. Atrophy: Just as hypertrophy was the increase in size of an organ due to the increased size of each cell individually, atrophy is just the opposite. Each cell decreases in size, thereby decreasing the size of the tissue or organ overall. Atrophy, like hypertrophy, is a cellular response or adaptation to its environment. A common example of atrophy is the disuse atrophy seen in the skeletal muscles of an arm or leg that has been immobilized in a cast. Nervous tissue will also atrophy as can be seen below comparing the brain of an 82 year old male on the left with the brain of a 32 year old male on the right. Note the enlarged sulci on the brain on the left. Link to Iowa Web site atrophy of brain III. Hyperplasia: Simply put, hyperplasia would be an increased number of cells. Now compare and contrast that with hypertrophy. With both hyperplasia and hypertrophy, the organ or tissue is enlarged. As previously discussed, in hypertrophy the organ or tissue is enlarged due to increased size of each cell. With hyperplasia, the organ or tissue is enlarged due to increased numbers of cells. Only cells that can actively divide can undergo hyperplasia. For example, epidermal cells of your skin, epithelial cells, hepatocytes, fibroblasts and bone marrow cells can undergo hyperplasia. However, nerve cells, cardiac and skeletal muscles cells cannot undergo hyperplasia. One thing to also keep in mind, the cells appear normal in a hyperplastic tissue. Another thing to keep in mind is that both hypertrophy and hyperplasia commonly occur simultaneously. For example, the dramatic growth of female breast tissue during hormonal stimulation exhibits both hypertrophy (increased size of each milk producing glandular cell) and hyperplasia (increased numbers of these milk producing cells). By turning on increased cellular divisions, there is now the possibility of something going biochemically wrong and a slightly increased risk of these hyperplastic cells transforming into cancerous cells. Link to Iowa web site hyperplasia IV. Dysplasia: A good way to remember what dysplasia describes it to consider it as ‘atypical hyperplasia’. As was just discussed, hyperplasia is an increased number of normally appearing cells. If there is an increase in the number of cells AND some of these cells now show histologic changes, the term to describe this finding is ‘dysplasia’. So what sort of histologic changes are we looking for? Generally dysplasia occurs in epithelial tissue (but not always). So some features would include the loss of normal orientation or thickness of epithelial layers; alterations in cell sizes and shapes; or nuclear changes. The following picture illustrates the difference between hyperplasia and dysplasia. On the left you see normal stratified squamous epithelium. Note the first, or basal, layer of cells with some showing signs of undergoing mitosis. As the subsequent layers are seen above the basal layer, the cells become larger, clearer, and eventually flatten out at the top layer. Now compare that to the dysplastic cells on the right. Certainly the epithelial layer is thickened, meaning that there is hyperplasia occurring. But look at the cells themselves. The basal layer of cells is thickened noticeably. The normal layering is no longer present. And if you look closely, you can observe some cells undergoing mitosis in the middle and upper layers of the skin, something that would never normally occur in simply hyperplastic skin. Link to Iowa web site dysplasia of squamous epithelium V. Metaplasia: Let me paint you a mental picture to best explain what metaplasia describes. Normally the trachea is lined with ‘pseudostratified ciliated columnar epithelium’. Tall, thin columnar cells with tiny little cilia on their surfaces line the trachea. As a result of long term exposure to the toxins in cigarette smoke, these cells adapt by developing into stratified squamous epithelium, like your skin, for protection. What was normally coated with columnar cells is now lined with squamous cells. There is a loss of function also due to the loss of the ciliary action inside the trachea. This alteration from one fully differentiated cell type into a completely different cell type is ‘metaplasia’. If one considers this alteration from a cellular point of view, it is a huge change genetically and biochemically to take cells that are programmed to differentiate into one type of cell and now reprogram it to differentiate into a different type of mature cell. This extensive reprogramming can frequently result in mistakes, thus helping to explain why metaplastic cells can commonly transform into cancerous cells. How can you identify metaplasia? Well, if you were to see a histologic view of the trachea, or a bronchus and saw not columnar cells, but stratified squamous cells, that’s ‘metaplasia’. So now a formal definition of metaplasia: where one fully differentiated cell type is replaced by another fully differentiated cell type. Interestingly enough, metaplasia is reversible. You will notice if you look back in your notes that either dysplastic or metaplastic cells frequently transform into cancerous cells. VI. Hydropic Swelling: A shift of extracellular fluid into the cell is usually the first manifestation of almost all forms of injury to cells. The cell will appear swollen with excess fluid (water). Link to iowa web site edema. Reversible Cell Injury: Let’s take a look at some changes that are observable in cells that have undergone persistent sublethal injury. Remember that all of our cells spend a great deal of ATP energy pumping ions (Ex: Na+, K+, H+, Ca++) across all of their membranes; including their plasma membrane, mitochondrial membranes (both inner and outer), endoplasmic reticulum, Golgi complex, lysosomal membranes, and nuclear membrane. When stressed, our cells suffer both the compounded effects of lacking sufficient ATP to keep the pumps working, and leakage of ions across membranes. This not only disrupts the membranes themselves, this upsets the ionic gradients across membranes and causes water molecules to flow by osmosis in the incorrect directions. Generally, the cell and many of its organelles will swell. The cytoplasmic swelling will disrupt the cytoskeleton and organelle swelling will change their shapes, appearances and compromise their function. (From: Wheater’s Basic Pathology by Burkitt, et. al., 3rd Ed. Pg. 5, Figure 1.3, Churchhill Livingstone) The first drawing above depicts healthy cellular structures, while the second drawing shows expected changes seen in an injured cell. Replace with rough drawing of some. Here are some examples of changes in the ultrastructure of reversibly injured cells. (From: Pathology by Rubin & Farber, 1st Ed., Pg. 6, Lippincott) To the left you see normal hepatocytes with tightly organized, parallel aligned RER. The round and oval circles are healthy mitochondria. To the left you see ‘hydropic swelling’ of an injured liver cell. Notice that the RER are now dilated by excess fluid. Even though the sizes and shapes of the mitochondria on the right may appear normal, notice that the inner membranes are no longer intact. (From: Pathology by Rubin and Farber, 1st Ed., Pg. 7, Lippincott) Again on the left is a healthy hepatocyte, exhibiting the small bumps (ribosomes) running along the parallel lengths of the endoplasmic reticulum. On the right, an acutely injured liver cell showing the detachment of the ribosomes from the endoplasmic reticulum and the deposition of free ribosomes in the cytoplasm. (From: Pathology by Rubin and Farber, 1 st Ed., Pg. 7, Lippincott) In this figure we see mitochondrial changes. A healthy cell is seen on the left; mitochondrial swelling seen in the ischemic cell on the right. Notice also the disruption of the inner mitochondrial membrane (cristae) in the ischemic cell on the right. Now keep in mind that these are electron micrographs, pictures taken with an electron microscope. You will not be able to see these cellular changes when looking at cells photographed with a light microscope. But it is instructive for you to know that these changes are occurring. IRREVERSIBLE CELL INJURY Here is a brief list of some of the microscopic changes you would expect to see in cells that have undergone irreversible cell injury and are dead or dying: Plasma membrane pinches off, forming “blebs”. Cell swells due to increased inflow of water by osmosis (loss of membrane Na+ and Ca++ pumps primarily, causes an imbalance in ionic gradients). High intracellular Ca++ causes an increase in intramitochondrial Ca++ levels, shutting down the mitochondrial ATP production. Mitochondrial swelling. Cytoskeletal clumping. Ribosomes fall off of endoplasmic reticulum. See an increase in free ribosomes. Swollen endoplasmic reticulum (may look like a vesicle or vacuole). Nucleus no longer round. Nucleus contains dark staining spots (condensed chromatin). (From: Pathology by Rubin and Farber, 1 st Ed., Pg. 14, Figure 1-12, Lippincott) Specific terms for nuclear changes: Pyknosis: Nucleus small, dark blue staining Karyorrhexis: Fragmented nucleus Karyolysis: Dissolution of nucleus (chromatin fragmented or extruded out of cell, nucleus no longer stains) Apoptosis: In many cases in the body, some cells will die without any insult, shock, injury or trauma. This “programmed cell death” is refereed to as apoptosis (a-po-to-sis). The cells have an active participation in their own demise. The cell activates a cascade of molecular events that result in an orderly degradation of cell constituents with minimal impact of the neighboring cells and tissues. Examples: Loss of interdigital webs in embryology. Metamorphosis of amphibians Proper retinal development Involution of lactating breast tissue Removal of self-reacting T-cells Differences between Apoptosis and Necrosis: Apoptosis On Single cell dies Spared Certain genes expresses Tissue changes Mitochondria Necrosis Off Groups of cells die Swelling and destruction None Cells shrink Intact Karyorrhexis Blebbing, intact Tissue Response Cell Volume Organelles Nucleus Cell membrane Inflammation Cells swell Disrupted Karyolysis Blebbing, loss of integrity TYPES OF NECROSIS: What dead cells or tissue look like depends upon many factors (where in the body, what was the cause of cell death, etc.). There are three common and easily distinguishable types of necrosis seen histologically. They are: I. Coagulative Necrosis: The outline of the cell remains, but the nucleus has disappeared. Commonly seen in the heart. Cell death results from lack of oxygenated blood flow to specific cardiac myocytes, with the surrounding cells surviving. II. Liquefaction Necrosis: Following aggressive immune cell lysis, the cells are destroyed and the focus of necrosis appears more fluid-like. Commonly seen in necrotic brain tissue as a result of infection. III. Caseous Necrosis: Characteristic of a tuberculosis infection of the lungs, there is a sphere whose center is filled with dead and dying cells and macrophages, with an outer rim of chronic and acute inflammatory cells (a granuloma). (From: Robbins Pathologic Basis of Disease by Cotran, Kumar and Robbins, 4 th Ed., Pg. 17, Figure 1-16.) (From: Pathology by Rubin & Farber, 1st Ed., Pg. 17, Figure 1-16, Lippincott)