N221_Concept_Map-Varnier
advertisement

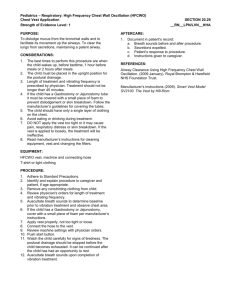
Running Head: PLANNING THE CARE Varnier 1 Planning the care of a patient with ineffective airway clearance related to Cystic Fibrosis Laura M. Varnier Duke University School of Nursing Planning The Care Varnier 2 Table of Contents Introduction………………………………………………………………………………………………………………3 Clinical Database…………………………………………………………………………………………………….4-5 Physical Assessment………..…………………………………………………………………………………………6 Physical Plan of Care……………………………………………………………………………………………...7-10 Psychological Plan of Care………………………………………………………………………………………...11 Evidence Base Practice Article Review…………………………………………………………………12-13 Conclusion………………………………………………………………………………………………………………..14 Anticipatory Guidance……………………………………………………………………………………………….15 References…………………………………………………………………………………………………………...16-17 Duke Standard of Care Information…………………………………….................................................18-20 Evidence Based Article………...………………………………………………………………….attached to email Growth Charts (statue for age, BMI, weight for age)……………...scanned and attached to email Planning The Care Varnier 3 Introduction During the second week of my pediatric clinical experience, I worked with a 17-year old, white female, admitted five days prior (9/12/2011) with a CF exacerbation with increased work of breathing. The patient’s mother began to notice her daughter becoming increasingly sick, the patient displayed trouble breathing, and the mother suspected pneumonia. The mother called the adolescent’s primary care provider and she was instructed to take her daughter to the ER at Duke University Medical Center. The patient’s medical history includes several hospitalizations for CF exacerbations, G-Tube placement, Infusaport placement and a RUL lobectomy. Regarding her CF, the patient has been compliant in completing daily physical therapy sessions while at the hospital, but could not communicate medication or PT regimen that she completes at home. Currently, her CF is pharmacologically managed, with enzymes, and physically managed with a Hill-Rom vest, which she wears twice a day to mobilize secretions as a form of chest PT. Currently, the adolescent is 3-days status post bronchoscopy and in the process of five 7-day antibiotics, that were susceptible to the cultures found in her sputum. The patient is a junior in home school and an active adolescent involved in several outside activities; her main interest is in drama club and recently played the lead role in the local production of Snow White. C. M. is an animated child that displays an extroverted nature and good interpersonal relationship with friends through stories she relays and phone calls she received throughout the shift I spent with her. Her family has not been present since their C.M.’s admission, though the patient relays a close relationship with parents and two siblings, an older brother (20) and a younger brother (12). The patient displays no need for assistive devices. Planning the Care 4 N221 Pediatric Nursing --- Clinical Database De-identified Patient Information Patient's Age: 17 LOS: 5 days Gender: F Reason for Admission: CF exacerbation with increased WOB Past Medical History: CF, pancreatic insufficiency, RUL lobectomy, GT placement and infusaport placement. Surgical Procedure: Bronchoscopy POD #3. Unique Code Student Initials: LMV Week: 2 Name of Agency: Duke 5300 F/Sat Advance Directives: DNR Status: Full Code Source of Information: Patient Family Composition: Father and Mother household with older brother to patient (20) and younger brother to patient (12). Treatments: CPT vest treatment with RT 4X daily; Isosource 1.5 at 100mL / h; antibiotic therapy. Assistive Devices: No assistive assistance necessary. Pertinent Diagnostic TestsTobramycin 1.4 mcg/mL (normal 0.5-10 mcg/mL); Sodium 137 mmol/L (normal 135-145 mmol/L); Potassium 3.7 mmol/L (normal 3.8-5.2 mmol/L); Chloride 102 mmol/L (normal 98-108 mmol/L); Carbon Dioxide 29 mmol/L (normal 21-30 mmol/L); BUN 8 mg/dL (normal is 7-20 mg/dL); Creatinine 0.5 mg/dL (normal is 0.3-1.1 mg/dL); Calcium 0.5 mg/dL (normal 8.7-10.2 mg/dL); Glucose 199 mg/dL (normal is 70-140 mg/dL). PFT on 9-15-2011: FVC 2.51 L which is 74% of predicted, FEV-1 is 1.73 L which is 57% of predicted, FEV1/FVC ratio is 69% compared to last test on 8-1-2011: FVC 2.81 L which is 83% of predicted and FEV-1 was 1.97 L which is 65% of predicted. (levels of most current test were worse than previous levels) Pathology Report or Infection Precautions: Contact and Droplet precaution; 9/16/2011 Bronchoscopy reported positive for 4+ Gram Negative rods, 1+ Oropharyngeal flora Allergies- Medications and Food: Cefotaxime (anaphylaxis), Colistimethate sodium (anaphylaxis), and Colistin (anaphylaxis) Medications: Fexofenadine 180mg PO Q day; Prozac 60 mg PO q day; Flonase 2 sprays intranasal Q day; Magnesium Oxide 400mg PO Q 12 hours; Multivitamin Source CF tablet Q day; Pancrealipase 5 capsules taken with meal PO Q TID; Protonix 40 mg PO Q BID; Phytonadione Tab 5 mg PO Q day; Miralax 8.5 mg PO Q day; Minocin 200 mg PO Q 12 hours; Ticarcillin Clavulanate IV 3.1 g Q 6 hours; Tobramycin Sulfate 500mg PO Q 12 hours; Azithromycin 500mg PO Q day; Itraconazole 250mg VT Q day Level of Development Prior to Admission: Prior to admission, Pt stated that she had “nothing wrong other than my CF”; patient displays intact gross and fine motor skills, intact language and communication skills and relays stories of socialization outside the hospital in interactions with friends and family members. Current Level of Development: Adolescent female; no assistance required to complete ADLs; patient displays intact gross and fine motor skills, intact language and communication skills and relays stories of socialization outside the hospital in interactions with friends and family members. Mobility: Pt is ambulatory without need for assistive aids and completes ADLs independently. Psychosocial Assessment: Patient displays age-appropriate physical, communication, emotional, and cognitive skills; Pt displays struggle in identity vs. role confusion and displays signs of increased peer influence and separation from parental guidance; family unit consist of mother and father, older brother (20) and younger brother (12). Family lives in a two story house and patient states that both her and her brother have “master Planning the Care 5 bedrooms in the house”; patient states that she gets “along well with both my brothers” and with her parents; father is a construction worker; mother is primary care provider to adolescent and homeschool teacher; no visitors were present during care provided by student nurse; Pt states compliance with all scheduled doctor’s appointment, but has displayed current and past problems with medication compliance as evidenced by patient stating that she forgets to take her “enzymes with her meals”, could not state to the emergency department intake nurse any of the medications that she is taking, and cannot state her chest PT schedule as manifested by patient’s several hospitalizations in recent years. Pt does not state difficulty in adapting to illness but does display behaviors, such as non-compliance with medication and frustration with constant “trips to the hospital” which keep the adolescent from other activities; Pt does not state that she feels scared or threatened in any way; Pt does not report any other stressors. Risk Assessment: Braden score of 28 (low risk for pressure ulcers); Low falls risk according to the Morse falls risk scale (score 20). High risk for nutritional deficiencies due to CF leading to decreased absorption of nutrients and fat and increased work of breathing, however BMI of 22.3. Planning the Care 6 *N221 Pediatric Nursing --- Physical Assessment Chief Complaints: “I felt a little dizzy when taking my medications this morning.” Current Level of Independence: Full independence; pt states she turns self when she “needs to”. Pt displays full ability to complete fine and gross motor skills to complete ADLs. Respiratory System SpO2= 99% RA; Lt lobes CTA, Rt upper lobe absent, right middle and lower lobes clear; infrequent, strong productive cough with small amounts of yellow/green sputum, natural airway, relaxed depth, symmetric chest movement, breathing RRR; Inspiration to expiration ratio 1:1; AP: Transverse 2:1. No accessory muscle use; no nasal flaring; no grunting; no wheezing. Activity Order: OOB 2 times a day; exercises with PT once daily. Cardiovascular System Neurological System HR 87 at 0800. Cap refill < 3 sec bilaterally in all extremities, nail bed color pink with apparent clubbing of the nails; skin warm and dry; S1, S2 audible, no audible S3 or S4 or murmurs; no edema; all pulses intact bilaterally in all extremities 2+. No audible bruits; No JVD at 45 degrees. Apical pulse RRR; no pulsations, lifts, or thrills. A&OX4; Pt alert, awake and calm, follows tiered commands, pupils PERRL, motor intact in all extremities, sensory intact in all extremities, sensation intact, all deep tendon reflexes intact. CN 2-12 motor and sensory intact. Speech/voice clear. Gastrointestinal System No N/V. Flat abdominal contour; soft, nontender abdomen, active bowel sounds in all 4 quadrants; no guarding upon palpation; pt denies flatus; rectal elimination route; last BM at 0600 on 9/17/2011, pt reported feces sunk; High calorie/High protein diet, feeds by mouth; GT feeds overnight (2145-0745) Isosource 1.5 at 100 ml/hr. Genitourinary System Frequently voids clear, yellow urine into commode; per MD order patient reports occurrences; pt reported 3 voids and 2 BM over 8 hour shift. IV fluid intake total 220 in 8 hours. TANNER stage 5. Vital Signs Time: 0800 B/P: 116/70; T: 36.6 Oral; P: 87; R: 26; O2: 99% Height: 155 cm Weight: 53.6 kg HC___N/A__ (< 36 mos.) Musculoskeletal Active ROM in all extremities with no discomfort noted; L=R strong handgrips (3+), L=R strong dorsiflexion (3+); active movement, steady gait. EENT Pt. denies use of glasses; PERRL, peripheral vision intact; no tearing; no vision lesions. Ears contained intact outer structures, no lesions or excess cerumen; conversational hearing intact. Nose mucosa pink and clear, no lesions or excess mucus, both nostrils patent. Lips pink and dry with no cracking. Mouth moist and pink, no lesions, good tonsillary pillar movement, no erythema. Teeth intact without dental caries, gums pink and moist, no tongue lesions; uvula midline. Integumentary System Skin color appropriate for race, Braden score of 21 (low risk for pressure ulcers); Skin dry, intact, warm, no tenting or tenderness. Clubbing present in nail beds. Wt Percentile: 40th Ht Percentile: 10th BMI Percentile: appr. 60th (> 2 y.o) IV Access: D5 ½ NS + 20 KCL at 5 ml/hr through Iport Midchest (CDI with occlusive dressing); dressing change 9/18/2011. Planning the Care 7 N221 Pediatric Nursing --- Concept Map Plan of Care- Physical Collaborative Problem list: Cystic Fibrosis; RUL lobectomy; G-tube placement; Infusaport placement; Ineffective airway clearance related to increased production of thick mucus as manifested by change in level of consciousness during activity; Activity intolerance related to imbalance between oxygen supply and demand as manifested by change in level of consciousness related to activity; Anxiety related to dyspnea, oxygen deprivation manifested by patient display of fearful behavior; Chronic sorrow related to presence of chronic disease manifested by feelings related to CF; Disturbed body image related to changes in physical appearance, treatment of chronic lung disease (clubbing, barrel chest, home oxygen and vest therapy, manifested by patient comments about physical changes; Imbalanced nutrition (less than body requirements) related to decreased absorption of nutrients and increased work of breathing manifested by 30th percentile ranking on CDC weight-for-age chart; impaired home maintenance related to extensive daily treatment and medication regimens manifested by current infection; Risk for fluid volume deficit related to decreased fluid intake and increased work of breathing manifested by patient constant request for more fluids; Risk for infection related to thick mucus harboring bacteria and Immunocompromised state manifested by pathology report results; Risk for skin breakdown related to malnutrition manifested by 30th percentile ranking on CDC weight-for-age chart; impaired social interactions and social isolation related to forced separation from peers manifested by need to constantly be interacting with others in person, on the phone or on the computer; Ineffective coping related to daily medication demands and Eriksonian stage of development manifested by patient non-compliance to medication regimen. Identified Priority of Care Key Problem / Nursing Diagnosis: Ineffective airway clearance related to CF etiology of increased production of thick mucus as manifested by change in level of consciousness during activity and excessive production of sputum. Supporting Subjective and Objective Data: Pt displays work of breathing between taking morning medications. Pt. displays several spontaneous, productive coughs and expels greenish/brown sputum into cup. Pt. assessment reveals signs of nail clubbing and increased work of breathing, approximately 26 times per minute. Pt states that she is able to “spit out secretions” but that this task is easier once she has worn her vest (which helps to mobilize secretions). Goals General Goal to achieve through Nursing Interventions: Pt will be able to effectively expel secretions, verbalize decreased work of breathing and maintain SpO2 levels >93%. Patient Behavioral Outcome Objective(s): The patient will maintain respiratory rate within 12 to 20 breaths per minute; pt response to interventions will be gauged based on auscultation of breath sounds and patient response; Patient will maintain SpO2 levels greater than 93% throughout the day; Pt will display proper return demonstration of incentive spirometry and express reasoning behind use; Pt will maintain HOB greater than 45 degrees and express reasoning behind the intervention; Pt will complete all 4 sessions of Hill Rom vest chest PT and communicate reasoning for the benefits of completing each session of chest PT. pt will display activity tolerance with PRN and PT exercises; pt will maintain adequate fluid intake to help mobilize secretions. Patient Educational Needs: Educate on signs and feelings of ineffective airway clearance and strategies to help manage this problem; Pt will maintain an arsenal of ideas to relieve ineffective airway clearance and can select the intervention that works most appropriately; Pt will be able to cough and deep breathe effectively. Plan and Interventions Nursing Interventions Monitor respiratory patterns, including rate, depth, and effort, q 4 hours during vitals checks and before and after interventions. Scientific Rationale “A normal respiratory rate for an adult without dyspnea is 12-16 breaths per minute. With secretions in the airway, the respiratory rate will increase” (Simpson, 2006). Patient Response/evaluation During 0800 vitals, Pt displayed regular rhythm and rate in respirations with increased work of breathing at 24 breaths per minute. After chest PT, respirations decreased to 18 breaths per minute. Pt reported that chest PT helps slow her breathing and help her to cough up secretions. During 1200 vitals, Pt again displayed an increase in respiratory rate at 20 breaths per minute. Response was expected. Planning the Care Auscultate lung sounds for baseline measures during morning assessment at 0800 and before/ after interventions. Monitor pulse oxygen saturation levels q 4 hours with vital checks and before/after interventions. Encourage the client to use incentive spirometry every commercial break in her television show for 1 hour (approximately q 15 minutes). Pt will be showed proper use of equipment and will return demonstrate the activity. Monitor Hill Rom Vest compliance as instructed by PT, as a form of chest PT, at a vest pressure of 4, frequency of 13, time 25 minutes, four times a day, before meals and before bedtime. Educate patient on need for Hill-Rom chest PT and the benefits of this procedure to help assist sputum excretion, typical of CF patients. Position patient with head of bed elevated at least 45 degrees to allow for maximal lung expansion and optimal respirations, throughout the day; patient can be at 15-20 degrees at night, but should not be lying flat. Encourage activity and ambulation, without causing exhaustion, as tolerated and PRN. 8 Breath sounds are normally clear or scattered fine crackles at bases. These crackles typically clear when the patient is asked to deep breathe or cough. “The presence of coarse crackles during late inspiration indicates fluid in the airway; wheezing indicates a narrowed airway” (Simpson, 2006). “An oxygen saturation of less than 90% (normal is 95-100%) … indicates significant oxygenation problems” (Clark, Giuliano & Chen, 2006). “The incentive spirometer is an effective tool that can help prevent atelectasis and retention of bronchial secretions” (Guimaraes & Atallah, 2007). Return demonstration is one way to evaluate learning related to a psychomotor skill (Bastable, 2008). “High-frequency chest-wall compression is a commonly used airway-clearance technique with efficacy similar, if not superior to conventional manual percussion and postural drainage” (Kempainen et al, 2010). “The Vest Airway Clearance System facilitates mobilization and removal of secretions from the lungs. The device utilizes an Air Pulse Generator and a Single Patient Use disposable, inflatable vest to deliver high-frequency chest wall oscillation (HFCWO). HFCWO creates oscillatory airflow that has been found to loosen and mobilize pulmonary secretions… indications for use of the Vest Airway Clearance System… diagnosis of disease such as cystic fibrosis” (Duke Nursing Process Standards, 2009). “An upright position allows for maximal lung expansion; lying flat causes abdominal organs to shift toward the chest, which crowds the lungs and makes it more difficult to breathe” (Ackley, 2008). “Body movement help mobilize secretions and can be a powerful means to maintain lung health” (Pruitt, 2006). At 0800, all left lobes, right middle and lower lobes were clear to auscultation during the 0800 assessment and remained clear both before and after Hill-Rom vest chest PT. Response was expected. Pt oxygenation remained above 95% throughout the day; specifically, 99% at 0800 and 98% at 1200. Response was expected. Pt responded well to return demonstration, teaching another person how to use the equipment, how incentive spirometry helps, and how often machine needs to be used to be effective. Pt stated that during her 1 hour television show she used the incentive spirometer during each commercial break. Pt expressed that it helped to have a goal of each commercial break to gauge frequency. Response was better than expected. Patient complied with each session of chest PT using the Hill Rom vest; during the first session of the day, patient finished with 8 productive coughs of green, dime sized sputum. Patient states that the procedure does not hurt but does take “a lot of time.” Patient correctly identifies reasoning behind the procedure and the need to complete the chest PT. Pt HOB remained greater than 60 degrees throughout the day and expressed that she likes to sleep at approximately 45 degrees at night. She relayed that she sleeps on 3 pillows when sleeping in her own bed. Response was expected Pt able to ambulate throughout her room and participate in PT activities without expressed exhaustion; SpO2 remained greater than 95% throughout activity. Education provided on the importance of activity to mobilize secretions and pt expressed understanding by repeating. Response was better Planning the Care 9 Encourage fluid intake of 2000 mL/day or more as requested. “Fluids help minimize mucosal drying and maximize ciliary action to help move secretions” (Smith-Sims, 2001). than expected. Pt intake of 1200mL of water and 246 mL of IV fluids throughout 8 hour shift. Pt expressed drinking “a lot” of water both in and out of the hospital; praise and reasoning given for the benefits of this practice. Response was better than expected. Summary of Patient Progress / Overall Goal Evaluation What is your impression of your patient's progress toward goal from your nursing care? How might you change the plan of care to improve patient outcomes? My patient responded well to the ideas I wanted to implement and displayed positive responses to the implemented nursing interventions. The patient was able to return demonstrate and re-teach many of the interventions back to me, which showed that not only could she use the skill, but she could verbalize what she was doing and what type of positive effect the intervention could have. On future care plans, I would like to implement the “huff technique” that I discovered through my research. This technique, specifically targeted to respiratory disorders such as CF, asks the client to use forced expiratory coughing while saying the word “huff” to “prevent the glottis from closing during the cough and is effective in clearing secretions from the central airway” (Goodfellow & Jones, 2002). Planning the Care 10 N221 Pediatric Nursing --- Concept Map Plan of Care- Psychosocial Collaborative Problem list: Cystic Fibrosis; RUL lobectomy; G-tube placement; Infusaport placement; Ineffective airway clearance related to increased production of thick mucus as manifested by change in level of consciousness during activity; Activity intolerance related to imbalance between oxygen supply and demand as manifested by change in level of consciousness related to activity; Anxiety related to dyspnea, oxygen deprivation manifested by patient display of fearful behavior; Chronic sorrow related to presence of chronic disease manifested by feelings related to CF; Disturbed body image related to changes in physical appearance, treatment of chronic lung disease (clubbing, barrel chest, home oxygen and vest therapy, manifested by patient comments about physical changes; Imbalanced nutrition (less than body requirements) related to decreased absorption of nutrients and increased work of breathing manifested by 30 th percentile ranking on CDC weight-for-age chart; impaired home maintenance related to extensive daily treatment and medication regimens manifested by current infection; Risk for fluid volume deficit related to decreased fluid intake and increased work of breathing manifested by patient constant request for more fluids; Risk for infection related to thick mucus harboring bacteria and Immunocompromised state manifested by pathology report results; Risk for skin breakdown related to malnutrition manifested by 30th percentile ranking on CDC weight-for-age chart; impaired social interactions and social isolation related to forced separation from peers manifested by need to constantly be interacting with others in person, on the phone or on the computer; Ineffective coping related to daily medication demands and Eriksonian stage of development manifested by patient non-compliance to medication regimen. Identified Priority of Care Key Problem / Nursing Diagnosis: Impaired social interactions and social isolation related to forced separation from peers manifested by need to constantly be interacting with others in person, on the phone or on the computer. Supporting Subjective and Objective Data: Pt spent time with student nurse communicating stories of friends and family; Pt would ask nurse “when are you coming back?” and “do you have to leave?”; Pt also spoke online and on the phone with friends. Pt did not have support system at bedside, since the first night she was admitted. Goals General Goal to achieve through Nursing Interventions: Pt will identify and express feelings of social isolation and verbalize methods to combat/cope with social isolation. Patient Behavioral Outcome Objective(s): The patient will establish a therapeutic relationship with student nurse and be able to express feelings regarding illness and hospitalization; pt will take medication for depression as prescribed; patient will utilize computer and telephone as forms of communication with friends and family to reduce feelings of social isolation; the client will invite friends and family members to the hospital when she feels visitation is the best way to combat social isolation. Patient Educational Needs: Pt will be able to know what social isolation feels like; pt will understand visitation policy and the benefit friends and family can have on feelings of social isolation; patient will understand the importance of medication and the role SSRI medications play in combating depression. Plan and Interventions Nursing Interventions Establish a therapeutic relationship by being emotionally present and authentic at the beginning of the shift. Scientific Rationale “Being emotionally present and authentic fosters growth in relationships and decreases isolation” (Jordan, 2000). Provide computers and Internet access to children with chronic disabilities that limit “Computers and ICT may be the solution to support development in children in need of Patient Response/evaluation The student nurse and patient were able to begin a relationship immediately through common interest and developing a comfortable relationship from the beginning of the shift. Response was better than expected. Student nurse encouraged computer use of pt to speak with friends and entertain other interest. Adolescent expressed that Planning the Care socialization throughout the shift at the child’s request. Discuss causes of perceived or actual isolation with the adolescent through conversation throughout the shift. Encourage visitation for a client who is hospitalized by both friends and family as warranted by the patient and staff at the facility, as the patient feels necessary. 11 special support if the technology is used as an integrating tool hospitals and acute care facilities” (Brodin & Lindstrand, 2004). “The individual’s experience of illness; the circumstances of everyday living that influence quality of life; and emotions, fear and concerns all have a bearing on the way illness is managed” (Anderson, 1991). “Visits from those in an emotionally close network were associated with perceived support, and this was associated with a decrease in depression” (Oxman & Hull, 2001). Establish trust one on one and then gradually introduce the client to others. Allow the client the opportunities to introduce issues and to describe his or her daily life. “Individualization of care, or tailoring of care, involves taking into account the client’s individuality and allowing that individuality to determine interpersonal approaches and healthillness management actions” (Brown, 1994). Medicate, as prescribed at 0900, to help adolescent with feelings of depression or isolation. “The FDA suicidality warning was associated with an overall decrease in antidepressant treatment for youth with a clinician-reported diagnosis of depression, but not for those with MDD. Also, following the warning, psychotherapy without medication increased” (Valluri et. al., 2010). she G-mail chats with most of her friends and uses Skype to virtual chat with her parents. Response was better than expected. Pt seemed please that she was able to utilize this option. Student nurse questioned adolescent’s feelings of isolation from friends and family members throughout her hospital stay and outside of the hospital. Pt reports that she feels “alone when she is in the hospital by herself”, but that her family and friends “visit a lot, when they can”. Response was expected. Upon conversation about perceived isolation, student nurse encouraged visitation from friends and family to help avoid social isolation. Pt stated that her family was “coming tomorrow” and that her friend was hoping to come “next week”. Pt displayed excitement with the upcoming visitation from friends and family. Response was not effective. Encouraged patient to describe daily routine and daily life with CF. By ascertaining information on daily schedule and interests, student nurse able to customize care plan; for example, incorporate incentive spirometry into commercial breaks of favorite television shows, develop a plan to maintain medication compliance within lifestyle, etc. Response was not effective. Administered SSRI medication as prescribed, according to the 6 rights of medication administration, for depression related to chronic disease and social isolation. Response was expected. Summary of Patient Progress / Overall Goal Evaluation What is your impression of your patient's progress toward goal from your nursing care? How might you change the plan of care to improve patient outcomes? The patient responded positively to conversations that were had and made a plan to implement several of the suggestions into her daily routine in order to avoid social isolation and feelings of being alone. Regarding social interactions, there are several other implementation methods I could have considered; for example, music therapy, distraction, guided imagery and writing/typing feelings and desires down could have acted as a distraction from social isolation. Planning the Care 12 Evidence Based Practice Review- Investigating High-Frequency Chest Wall Compression Control Most Advantageous to CF patients One of the most rigorous responsibilities of all CF patients, along with medication compliance, is adhering to strict physical/respiratory therapy prescriptions of chest physiotherapy to assist with expectoration of secretions. If RT/PT is unavailable, it is the nurse’s responsibility to follow the prescribed system regimen and administer the procedure (Duke Hospital Protocol, 2009). In recent years, it was determined that “high-frequency chest-wall compression is a commonly used airway-clearance technique with efficacy similar, if not superior to conventional manual percussion and postural drainage” (Kempainen, 2010). Through modern use of technology, Hill-Rom created a vest that produces a mimicking of chest wall PT at a higher frequency. Furthermore, Duke Hospital protocol supports the use of the Vest Airway Clearance System, particularly in CF patients “to facilitate mobilization and removal of secretions from the lungs… creating oscillatory airflow that has been found to loosen and mobilize pulmonary secretions” (2009). However, with this new technology, the “Vest® Airway Clearance System [only] received FDA clearance to market for bronchial secretion clearance in 1988 and for sputum induction in 2000” alluding to the fact that large amounts of research particular to disease etiology needs to be conducted to determine optimal control settings for the Vest expectoration system (Hill-Rom, 2011). In 2010, Kempainen, Milla, Dunitz, et al. attempted to determine the optimal control settings in pressure and frequency that allow for maximum efficacy particularly in CF patients, by assessing higher-pressure (6-10 on the Hill-Rom vest 1-10 scale) with variable mid-frequency (8, 9 ,10 and Hz, plus 18, 19, and 20 Hz) chest wall compression compared to lower-pressure (5 Planning the Care 13 on the 1-10 scale) paired with constant mid-frequency settings (14-16 Hz). The controlled randomized crossover study chose 16 individuals, over 18 years of age that had been diagnosed with CF according to the Cystic Fibrosis Foundation criteria. The participants were asked to use the vest system, while remaining uninformed to which chest wall settings were being utilized. Effectiveness of each frequency method was assessed using sputum weight, incentive spirometry, pulmonary function test and lung viscoelasticity. The researchers found that the “use of the higher-pressure/variable-frequency settings resulted in significantly greater median sputum wet weight expectoration (6.4 g, range 0.4922.0g, versus 4.8 g, range 0.24-15.0g for lower-pressure/mid-frequency HFCWC, P=0.02)” (Kempainen, Milla, Dunitz, et al, 2010). Both pressure and frequency systems produced similar results in incentive spirometry, PFT’s and lung viscoelasticity measures. The researchers made it a point to note the small sample size of the study, the mild-to-moderate nature of the participant’s CF, and that all subjects were adults (over the age of 18). My 17-year-old patient’s Hill-Rom chest PT settings were set at a vest pressure of 4 and a frequency of 13, utilizing the lower-pressure, constant mid-frequency parameters. As an active member in patient care, as an administrator of the vest system and as an advocate for my patient, I would like to encourage prescribers, RT, PT and hospital authorities to investigate the evidence regarding higher pressure/variable frequency chest wall compression, specifically for CF patients, using the Hill-Rom Vest Clearance system. To provide the best care for our patients, we need to investigate the most appropriate, evidenced-based information for Vest control, specific to disease etiology and patient constraints, and begin implementing these control adjustments into hospital-wide policy. Planning the Care 14 Closing Comments The link between classroom knowledge and implementation of skills surfaced throughout my interactions with my pediatric patient. With this patient, I was able to spend time sitting and talking, while gathering assessment data simultaneously. By viewing this patient from a developmental standpoint, I could apply Erikson’s stage of identity vs. role confusion in her attempts to separate from parents by staying at the hospital independently (at my patient’s request), the importance of connection with peers through interpersonal stories and interpret her non-compliance with medication as a form of rebellion, typical in this age group and characteristic of adolescents with progressive, chronic diseases. Through a developmental lens, I was able to ascertain the information that I needed while acquiring the best way to connect with her. I could identify the role her peers play in her life and note the shift from parental influence to peer influence. Also, a developmental perspective allowed me to build a quick rapport, by relating to something that she was interested in and allowing her to tell me about her interests. Finally, working with this patient allowed me to get outside of the textbook and apply concepts and theories first-hand into my interactions with my patient. This approach led me to subsequent success in establishing trust with my patient and provided an overall positive feeling regarding our interactions. Planning the Care 15 Anticipatory Guidance with a 17-year-old Patient Initials: C. M. Child Age- 17 years 5 months Date of Assessment: 9-17-2011 What activities child can currently perform (according to category): Personal Social skills o Pt engages in stories of relationships with friends and family. o Pt reflects extroverted personality by engaging in a school play, participating in conversations with caregivers and friends, and displaying Fine Motor Adaptive skills o Pt displays fine motor skills through computer skills and personal care activities. Language skills o Speech is understandable and clear, with a wide range of vocabulary and intonation. o Pt has developed age-specific jargon and jargon within peer group. Gross Motor o Pt able to walk, perform physical therapy, and initiate all self-care activities. Anticipatory Guidance: Pt will continue in Erickson’s psychosocial skill of identity vs. role confusion by appearing concerned with how they appear to others and role identification within groups, personal, sexual roles, and emotional situations. Pt may display an increase in sleep and may develop acne. The adolescent will need adequate amounts of sleep, approximately 10-12 hours. Adolescents will develop high frontal lobe cognitive functions and continue to achieve independence from parent; begin asking for or needing guidance regarding personal behaviors such as sex education, STD, stress reduction; screening for anorexia, obesity, and mental health concerns; remain up to date on immunizations and continue to receive regular yearly checkups; needs education on the risk of risky behaviors such as substance abuse, tattoos, teen pregnancy. The adolescent responds best to praise. Adolescent may show signs of resistance to authority and impulsivity; more influence from peer groups than from adults at this age. Safety Concerns with 17 year-olds: Parents aware of the leading causes of death for this age group, including 1) unintentional injury including motor vehicles accidents, 2)homicides, and 3) suicide; parents need to be informed on the importance of proper gun storage and firearm safety and children need to know the dangers of firearm; aware of the risk of sports injuries. Prevention is the most effective tool to implement to avoid injury. Patient’s assessed developmental age: 17 years (appropriate developmental age corresponds to numeric age). Planning the Care 16 References Ackley, B. & Ladwig, G. (2008). Nursing diagnostic handbook: an evidence-based guide to planning care. St. Louis, MO: Mosby, Inc. Anderson, J. M. (1991). Immigrant women speak of chronic illness: the social construction of the devalued self. Journal of Advanced Nursing, 16, 710. Bastable, S. B. (2008). Nurse as educator: principles of teaching and learning for nursing practice. Sudbury, MA: Jones and Bartlett Publishers. Brodin, J. & Lindstrand, P. (2004). Are computers the solution to support development in children in need of special support? Technology and Disability, 16, 137-145. Brown, S. (1994). Communication strategies used by an expert nurse. Clinical Nursing Research, 3 (1), 43. Clark, A. P., Giuliano, K., & Chen, H. M. (2006). Pulse oximetry revisited: “but his O (2) sat was normal!”. Clinical Nursing Specialist, 20 (6), 268-272. Duke Nursing Process Standards (2009). Vest airway clearance system procedure. Durham, NC: Duke University Health System. Goodfellow, L. T. & Jones, M. (2002). Bronchial hygiene therapy. American Journal of Nursing, 102 (1), 37-43. Guimaraes, M. F., Atallah, A. N., & El Dib, R. P. (2007). Incentive spirometer for prevention of postoperative pulmonary complications in upper abdominal surgery. Cochrane Database of Systematic Reviews (2): CD0068058. Hill-Rom Services Inc. (2011). The vest airway clearance system. Research and Evidence. http://www.thevest.com/research/. Planning the Care 17 Jordan, J. V. (2000). The role of mutual empathy in relational/cultural therapy. Journal of Clinical Psychology, 56 (8), 1005. Kempainen, R. R., Milla, C., Dunitz, J., Savik, K., Hazelwood, A., Williams, C., Rubin, B. K., & Billings, J. (2010). Comparison of settings used for high-frequency chest-wall compression in cystic fibrosis. Respiratory Care, 55 (6), 695-701. Oxman, T. E. & Hull, J. G. (2001). Social support and treatment response in older depressed primary care patients. Journal of Gerontology Series B, Psychological Sciences and Social Sciences, 56 (1), P35. Pruitt, B. (2005). Help your patient combat postoperative atelectasis. Nursing, 35 (5), 64. Simpson, H. (2006). Respiratory assessment. British Journal of Nursing, 15 (9), 484-488. Smith-Sims, K. (2001). Hospital-acquired pneumonia. American Journal of Nursing, 101 (1), 24. Valluri, S., Zito, J., Safer, D., Zuckerman, I., Mullins, C., & Korelitz, J. (2010). Impact of the 2004 food and drug administration pediatric suicidality warning on antidepressant and psychotherapy treatment for new-onset depression. Medical Care, 48(11), 947-954. doi:10.1097/MLR.0b013e3181ef9d2b Planning the Care Neurosciences Services Procedure Title: Vest® Airway Clearance System Procedure Effective Date: June 2008 Revised: January 2009, December 2009 Purpose: To ensure appropriate and safe use of The Hill-Rom Vest to assist appropriate neurological patients with airway clearance. Level: * Interdependent. MD Order for PT consult for Airway Clearance required. PT may recommend the Vest after patient evaluation. Refer to Physical Therapy Airway Clearance Decision Process for Neurologically impaired patients. Supportive Data: The Vest® Airway Clearance System facilitates mobilization and removal of secretions from the lungs. The device utilizes an Air Pulse Generator and a Single Patient Use disposable, inflatable vest to deliver High-Frequency Chest Wall Oscillation (HFCWO). HFCWO creates oscillatory airflow that has been found to loosen and mobilize pulmonary secretions. Content: Determine patient eligibility for use of the Hill-Rom Vest (Refer to Vest Decision Process Algorithim) Indication for use of The Vest® Airway Clearance System: 1. Documented need for airway clearance as defined by the American Association for Respiratory Care (AARC) 1 clinical practice guidelines. These guidelines include: a. Evidence of difficulty with secretion clearance. b. Difficulty clearing secretions with expectorated sputum production. c. Evidence or suggestion of retained secretions in the presence of an artificial airway. d. Presence of atelectasis caused by or suspected of being caused by mucus plugging e. Diagnosis of disease such as cystic fibrosis, bronchiectasis, or cavitating lung disease f. Need for sputum sample for diagnostic evaluation Absolute Contraindications: 1. The Vest® Airway Clearance System is contraindicated if the following conditions are present. a. Mechanical Ventilation. b. Unstable Head /neck/spine injury. c. Active hemorrhage with hemodynamic. Relative Contraindications: The decision to use The Vest® Airway Clearance System for airway clearance therapy in the presence of the conditions listed below requires careful consideration and assessment of the individual patient’s case. a. Intracranial pressure (ICP) >20 mm Hg, or patients in whom increased intracranial pressure is to be avoided. b. Uncontrolled hypertension. c. Hemodynamic instability. d. Pulmonary edema associated with congestive heart failure. 18 Planning the Care e. Bronchopleural fistula. f. Subcutaneous emphysema. g. Large pleural effusions or empyema. h. Recent esophageal surgery. i. Active or recent gross hemoptysis. j. Pulmonary embolism. k. Uncontrolled airway at risk for aspiration such as tube feeding or recent meal. l. Distended abdomen. m. Bronchospasm. n. Suspected pulmonary tuberculosis. o. Recently placed transvenous pacemaker or subcutaneous pacemaker. p. Recent epidural spinal infusion or spinal anesthesia. q. Recent spinal surgery or acute spinal injury. r. Rib fractures, with or without flail chest. s. Surgical wound, healing tissue, recent skin grafts, or flaps on the thorax. t. Burns, open wounds, and skin infections on the thorax. u. Lung contusion. v. Osteomyelitis of the ribs. w. Osteoporosis. x. Coagulopathy. y. Complaint of chest wall pain. z. Chest or thoracic circumference measurements outside of the recommended minimum or maximum dimensions for each size vest. Reportable Conditions: 1. Use of The Vest® Airway Clearance System should be evaluated or modified if the following circumstances occur: a. Pulmonary hemorrhage. b. Hypoxia. c. Increased intracranial pressure. d. Vomiting and aspiration. e. Acute hypotension during the procedure. f. Bronchospasm. g. Pain or injury to muscles, ribs or spine. h. Cardiac dysrhythmias. Equipment 1. Single patient use Wrap SPU Vest. 2. Air Pulse Generator. 3. Air Hoses (to connect the Single Patient Use disposable, inflatable vest to the Air Pulse Generator). Procedure 1. Verify order required: PT consult for Airway Clearance. 2. Plug Air Pulse Generator (Model 205) into a known good, properly grounded power outlet. 3. Instruct patient about the treatment that will be performed. 4. At initial therapy measure patient for appropriately sized vest to assure proper fit 19 Planning the Care and confirm proper thoracic dimensions. 5. With the Wrap SPU Vest deflated, adjust the inflatable vest to fit comfortably close to the underarms. Have the patient take a deep breath and secure the hookandloop fasteners to close the Wrap SPU Vest. Adherence to these steps should be followed as closely as the user’s condition allows. 6. Connect the Air Hoses to the Air Pulse Generator and to the Air Hose Ports of the inflatable vest. 7. Assemble nebulizer and other equipment needed for the delivery of aerosol therapy, if prescribed. 8. . Enter the prescribed settings for the Frequency, Pressure, and Time. 9. *Begin aerosol therapy, if prescribed. 10. Initiate therapy with The Vest® Airway Clearance System as directed by physician’s order. 11. Maintain observation of patient during treatment 12. Unless directed otherwise by the prescribing physician, after completing 5 to 10 minutes of therapy, pause the Air Pulse Generator by pressing the OFF button or squeezing the Remote Control one time. Have the patient cough or suction to clear loosened secretions. 13. To continue treatment, press the ON button, or squeeze the Remote Control once. Treatments commonly involve 10 to 30 minutes of actual HFCWO (oscillation). 14. Press the OFF button one time when no time remains in the treatment session or two times during a session to end the treatment. 15. . Disconnect the Air Hoses from the inflatable vest, and then from the Air Pulse Generator. 16. Loosen the hook-and-loop fasteners and remove the inflatable vest from the user. 17. Store vest wrap in The Vest wrap is single patient use. 18. Discard when patient no longer requires treatment patient room for next treatment. References: 1. Hill-Rom, The Vest Airway Clearance System , www.thevest.com 2. AARC Clinical Practice Guideline: Postural Drainage Therapy, Respiratory Care 1991;36:1418-1426. (2007) 3. Brierly S, Adams C, et al, 2003. Safety And Tolerance Of High-Frequency Chest Wall Oscillation (HFCWO) In Hospitalized Critical Care Patients. Respiratory Care 48 (11): 1112 4. Lange D J, Lechtzin N, et al, 2006. High-frequency chest wall oscillation in ALS. Neurology 2006:67:991-997. Approval: Duke Neuroscience CPC, Duke Neuroscience NLC, Duke Physical Therapy Distribution : 4100, 4200, 4300 20