Refeeding Syndrome (173)

Refeeding Syndrome (173)
1) Up to Date - Eating disorders: treatment and outcome
2) Refeeding Syndrome: Recognition Is the Key to Prevention and Management,
JONATHAN TRESLEY; PATRICIA M. SHEEAN, PhD, RD. Journal of the
AMERICAN DIETETIC ASSOCIATION December 2008 Volume 108 Number 12
3) Refeeding syndrome and hypophosphatemia, M Marinella. Journal of intensive care medicine 20(3) 2005. 155-159
4) Nutrition in clinical practice—the refeeding syndrome: illustrative cases and guidelines for prevention and treatment. Stanga et al. European Journal of Clinical
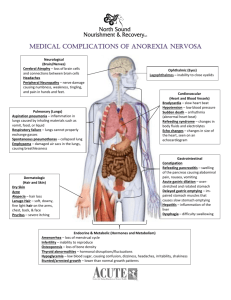
Nutrition (2008) 62, 687–694 o Potentially fatal condition resulting in rapid changes in fluids and electrolytes when malnourished patients are given nutrition o Patients with severe anorexia nervosa (ie, less than 75 percent of ideal body weight) and those who have lost a large amount of weight rapidly are at risk for the refeeding syndrome during the first two to three weeks of refeeding o Pathophysiology of Starvation o 24 to 72 hours of fasting, blood glucose levels begin to decline. Insulin concentrations decrease while glucagon levels increase, resulting in mobilization of glucose stores primarily from glycogen o Due to glucose-6-phosphatase and Glut-2 transporters, skeletal muscle glycogen can only supply glucose to the myocytes, whereas liver glycogen is catabolized and provides glucose for the entire body o 72 hours – glycogen stores from the liver and the skeletal muscle are fully and partial depleted, respectively, glucose synthesis occurs predominantly from lipid and protein breakdown products o Hepatic fatty acid-oxidation results in the formation of ketone bodies
(acetoacetate, -hydroxybutyrate and acetone) which can be reconverted to acetyl-coenzyme A to produce energy via the Krebs cycle o Energy in the form of glucose is also synthesized from endogenous glycerol, the gluconeogenic amino acids (primarily alanine and glutamine) and lactate and pyruvate produced by glycolysis via the Cori cycle o this adaptation to altered sources of energy can result in profound fat and muscle wasting, in addition to total body depletion of electrolytes, magnesium, potassium, and phosphate o Defined primarily by manifestations of severe hypophosphatemia (including cardiovascular collapse, rhabdomyolysis, seizures, and delirium) o Hypophosphatemia o Phosphate is the most abundant intracellular anion available for transcellular shift b/e intra and extracellular spaces o Dietary PO4 is absorbed in the jejunum and is filtered at the glomerulus
75% of filtered PO4 is reclaimed at the proximal and distal convoluted tubule o Phosphorus is used as a component in cellular membranes, enzymes, nucleic acids and nucleoproteins BUT most importantly is its role in the formation of
ATP
o There are a number of abnormalities that produce the above symptoms o Malnourished patients can have depleted intracellular phosphate stores
With refeeding and a shift from fat to carbohydrate metabolism, hypophosphatemia can occur as part of glycolysis, which includes the formation of phosphorylated carbohydrate compounds in the liver and skeletal muscle
Hypophosphatemia can result in impaired energy stores due to depletion of intracellular adenosine triphosphate (ATP) and tissue hypoxia due to reduced levels of erythrocyte 2,3 diphosphoglycerate (2,3-DPG) o Increased oral intake leads to an increase in circulatory volume, while myocardial function is depressed secondary to decreased myocardial mass and secondary to hypophosphatemia. This can lead to heart failure o Respiratory failure due to weakness of the diaphragm has been described o Hypophosphatemia-induced manifestations of muscle dysfunction include a proximal myopathy (affecting skeletal muscle) and dysphagia and ileus (affecting smooth muscle). o acute hypophosphatemia superimposed upon preexisting severe phosphate depletion can lead to rhabdomyolysis
Rhabdomyolysis with the associated release of phosphate from the damaged muscle cells has two clinical consequences: it may mask the underlying hypophosphatemia and it may therefore protect against the development of other hypophosphatemic symptoms o Hypokalemia and hypomagnesemia can lead to cardiac arrhythmias. Hypokalemia results from insulin secretion in response to a caloric load, which shifts potassium into cells. The etiology of hypomagnesemia in this setting is not known o Wernicke's encephalopathy, manifesting as delirium, can occur with refeeding in thiamine deficient patients o Risk Factors o Patients with weight loss of _10% within a 2- to 3-month period o Individuals who are _70% of ideal body weight (eg, cancer patients, the elderly, third-world populations) are at greatest risk for refeeding syndrome
Proposed Refeeding
Guidelines