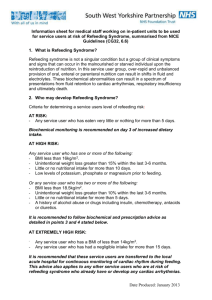
Refeeding Syndrome
advertisement

Refeeding Syndrome 24/8/10 Boateng, B.S., et al (2010) “Refeeding syndrome: Treatment considerations based on collective analysis of literature case reports” Nutrition 26:156-167 Ormerod, C. et al (2010) “Refeeding syndrome: a clinical review” British Journal of Hospital Medicine, Vol 71 (12) page686-690 RFS = a group of clinical findings that occur in severely malnourished individuals undergoing nutritional support. - more common than we think. - prolonged starvation -> provision of nutritional supplementation from any route. - chronic malnutrition leads to protein catabolism with total body phosphate depletion despite normal serum phosphate - introduction of carbohydrates leads to an anabolic state which unmasks total body phosphate depletion and leads to precipitous drop in serum phosphate - insulin + glucose = massive uptake of phosphate, K+ and Mg2+ into cells RISK FACTORS – any one who may be malnourished: Decreased intake - eating disorders alcoholism depression fasting vomiting dysphagia Crohns malabsorption chemotherapy short bowel syndrome prolonged NBM bariatric surgery Increased catabolism - inflammatory process - cancer CLINICAL FEATURES CVS: arrhythmia, HT, CHF GI: abdo pain, constipation, vomiting, anorexia MUSCU: weakness, myalgias, rhabdomyolysis, osteomalacia Jeremy Fernando (2011) RESP: SOB, ventilator dependence, respiratory muscle weakness -> requiring intubation and ventilation NEURO: weakness, paraesthesia, ataxia, delirium, coma, central pontine myelinosis, seizures, Korsakoff’s syndrome or Wernicke’s encephalopathy (confusion, ataxia, ophthalmoplegia) METABOLIC: infections, thrombocytopaenia, haemolysis, anaemia HAEM: reduced 2,3 DPG production -> left shift of oxyHb dissociation curve OTHER: ATN, Wernicke’s encephalopathy, liver failure INVESTIGATIONS - hypophosphataemia hypokalaemia hypomagnesaemia hyperglycaemia thiamine deficiency (erthryocyte transketolase or thiamine level) trace elements deficiencies MANAGEMENT Summary of Management Jeremy Fernando (2011) (1) recognize patients at risk (2) provide adequate electrolytes, vitamin (thiamine, water and fat soluble) and micronutrient (Zn, Fe, Se) supplementation (3) careful fluid resuscitation to avoid fluid overload (4) cautious and gradual energy restoration (5) monitoring of critical laboratory indices Resuscitate A – may need intubation for encephalopathy and bulbar dysfunction with aspiration B – ventilation because of respiratory muscle weakness with hypercapnic respiratory failure C – correction of electrolytes c/o arrhythmias, cautious slow volume resuscitation, central access and invasive monitoring if haemodynamically unstable D – may have profound weakness, cerebellar dysfunction, delirium and coma -> responds to slow correction of electrolytes Electrolyte abnormalities + Acid Base Disturbance Hypophosphataemia (<1.0 mmol/L) – replace either IV or PO Hypokalaemia (<3.5mmol/L) – replace IV or PO Hypomagnesaemia (<0.7mmol/L) – replace IV or PO Hyponatraemia – don’t correct rapidly unless symptomatic (less than 10mmol/L/day) Hyperglycaemia - monitor -> insulin if required Anti-dote Nil – supportive care Underlying cause - screen those at risk Feed - <20% of basal energy expenditure to start 10kcal/kg/day aim to get to normal nutrition over 1 week titrate feed to resolution of symptoms and laboratory parameters Vitamins (minimum of 10 days) Vitamin B1 (thiamine) – 300mg IV LD prior to starting nutrition -> 100mg/day Vitamin B6 (pyridoxine) – 1.7mg/day Vitamin B12 (cobalamine) – IM injection Folate – 400mcg/day Fat soluble vitamins – DEKA – can be replaced via feed Micronutrients Selenium – 100-400mcg/day LD -> 20-70mcg/day Zinc – 10-30mg/day LD -> 2.5-5mg/day Iron – no loading dose required -> 10mg/day PO Jeremy Fernando (2011) Disposition - managed in an HDU/ICU environment if severe Jeremy Fernando (2011)